-
PDF
- Split View
-
Views
-
Cite
Cite
Matteo Torresetti, Benedetta Peltristo, Francesco Mauro Junior Taddei, Alessandro Scalise, Giovanni Di Benedetto, Heel reconstruction for a Marjolin’s ulcer in a patient with multiple limb amputations: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac400, https://doi.org/10.1093/jscr/rjac400
Close - Share Icon Share
Abstract
Coverage of the heel defects usually represents a challenge for the proper reconstructive requirements of the weight-bearing area of the foot. The presence of multiple limb amputation may represent a further concern for conventional free flap donor sites and the patient’s functional limitation, thus making reconstruction even more challenging. Amputee patients may be subjected to a higher risk of foot ulcerations and choosing the more appropriate reconstructive option in such patients is crucial. Here we describe the application of the medial plantar flap as a first-line option in a 66-year-old amputee patient with a squamous cell carcinoma arising from chronic ulceration on the left heel, that was successfully treated with limited functional limitations and excellent anatomical contour of the foot. Despite its use has been widely described for heel reconstruction, we believe that medial plantar flap would deserve greater relevance in the reconstructive scenario in such challenging cases.
INTRODUCTION
Marjolin’s ulcer is a malignant degeneration of a chronic wound, typically related to old burn scars, osteomyelitis fistulae, frostbite and amputation stumps [1]. The majority of Marjolin’s ulcers develop squamous cell carcinoma (SCC), even though basal cell carcinomas, melanomas and sarcomas could be identified as well. It is most commonly found in the lower limb, mainly on the plantar foot [2]. We report a case of a SCC arising from chronic ulceration on the left heel in a 66-year-old amputee patient, which was particularly challenging both for the proper weight-bearing requirements for heel reconstruction and the multiple limb amputation.
CASE REPORT
A 66-year-old man presented to our Clinic with recurrent ulceration on the left heel. The patient reported the amputation of the left forearm and a right below-knee amputation for a work accident about 30 years before, with a concomitant injury of the left heel and skin graft reconstruction. Since then, the patient has used a prosthetic leg for walking. Twenty years after the trauma, the patient underwent endovascular revascularization of the posterior tibial artery for peripheral arterial occlusive disease. He reported several ulcerations of the heel through the years which were treated conservatively. Wound examination revealed an ulcer (5.5 × 4.5 cm) with irregular edges and hypertrophic tissue, which was palpably indurated and fixed to the underlying subcutaneous tissues (Fig. 1). Multiple biopsies were performed and the histopathology report showed the presence of SCC. A staging whole-body computed tomography (CT) scan showed no distant metastases, and the lesion was strictly close to the calcaneus (Fig. 2). The patient underwent wide excision of the SCC with partial tangential calcanectomy. The heel defect was reconstructed with a medial plantar flap; the flap donor site was covered using Integra® Dermal Regeneration Template followed by skin grafting after 25 days (Fig. 3A–C). The histologic examination confirmed an ulcerated moderately differentiated SCC with free surgical margins. After tumor board multidisciplinary discussion, the patient started oncological follow-up.

Preoperative picture of the SCC of the heel measuring 5.5 × 4.5 cm, and preoperative markings of the flap. Vessels were marked on the skin with the assistance of a handheld 8-MHz Doppler ultrasound scanner.
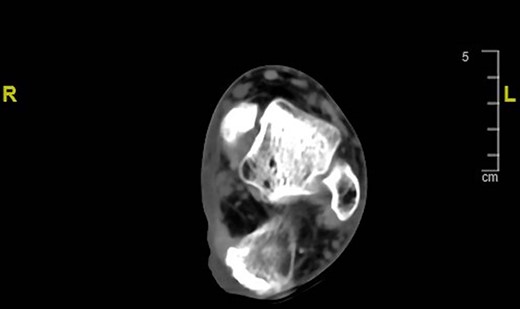
Preoperative CT scan of the left foot showing the lesion strictly close to the calcaneus.
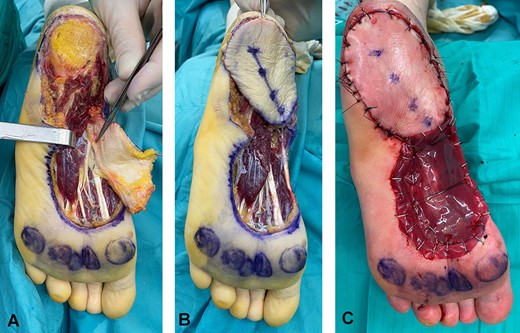
Intraoperative figures showing the defect after tumor excision, and the flap harvested with the medial plantar artery indicated by the forceps (A). Flap coverage of the heel defect (B). Immediate postoperative appearance; the donor site was covered with a meshed Integra® Dermal Regeneration Template (C).
At the 18-month follow-up, no signs of local ulceration were detected. The patient was able to walk using standard shoes and the sensation in the heel area was preserved. The anatomical contour of the foot was excellent and the flap showed optimal strength under normal plantar pressures (Fig. 4).

Eighteen-month follow-up picture showing no ulceration or tumor recurrence, an excellent anatomical contour and a satisfactory aesthetic result.
DISCUSSION
Chronic irritation or repeated trauma on scar tissue can induce cell atypia, anomalous mitotic activity and finally lead to a malignant transformation [3]. The range time for the onset of the malignancy is between 11 and 75 years [4] and SCC is the most frequent tumor identified [2].
Multiple limb amputations involving both an upper and lower limb are really uncommon and represent an extremely life-changing procedure. An altered gait and plantar pressure distribution in the contralateral limb in below-knee amputees may theoretically increase the risk of recurrent plantar ulceration on the weight-bearing areas of the intact foot. The impact of unilateral transtibial amputations on the loading of contralateral foot has been investigated in distinct populations and it is still debated. Kanade et al. demonstrated that the intact foot showed significantly higher mean peak plantar pressures in the transtibial amputations group over the heel compared with non-amputees patients in diabetic patients. Nevertheless, these higher foot pressures seem to be related to diabetic peripheral neuropathy rather than the amputation itself [5]. Even the design of the prosthetic foot has been implicated as a possible influencing factor on the loading of the intact foot in traumatic and dysvascular unilateral amputations [6, 7].
Heel reconstruction is challenging due to the unique anatomical properties of the heel fat pad and its fundamental properties of cushioning and shock-absorbing system during the heel strike. Several reconstructive options have been proposed including local or free flaps, skin grafts and dermal substitutes, each of them with its pros and cons [8]. Nevertheless, no consensus exists and an ‘ideal’ method for weight-bearing reconstruction has not been made clear yet [9].
Microsurgical free flaps such as radial forearm flap, lateral thigh flap or skin grafted muscle flaps remain the best solution for large complicated heel reconstruction [10, 11]. Nevertheless, microsurgical flaps are time-consuming, they have higher postoperative complications and require more postoperative care with higher costs. Moreover, compromised patients with several comorbidities may be not suitable for this type of surgery.
Local flaps have been proposed as the mainstay of treatment for heel reconstruction due to their reliability, constant vascularity, restoration of sensation and their similarity with the anatomical properties of the weight-bearing surface of the foot thus following the golden rule of reconstruction: ‘replace like with like’ [12]. Among them, the medial plantar flap is a sensate flap and is associated with a high flap survival rate (98.2%), low minor flap complications (9.4%) and low donor site complications (5.2%) [13].
In our case, the reconstructive challenge was represented not only by the conventional weight-bearing requirements, but also by the presence of multiple limb amputations, and not least by the presence of peripheral vascular disease.
Subjecting a patient to a free flap reconstruction presupposes adequate compliance of the patient and a limitation, albeit transitory, of the autonomy in basic daily activities. Harvesting a free radial forearm flap or anterolateral thigh flap provisionally reduces the normal mobility of the involved limb. In the case of postoperative complications, this period of temporary ‘disability’ could be lengthened. This could be well tolerated under normal conditions. Nevertheless, in patients forced to use prostheses in two different hemisoma and different limbs (both for the upper and lower extremity), it could represent a serious concern. Moreover, the possibility of using the radial forearm flap was limited to the residual upper limb only in our case. Therefore, we did not consider microsurgical tissue transfer as a first-line option. The presence of peripheral artery disease in the patient’s medical history represented a further concern, even though it was not an absolute contraindication for free flap surgery.
Local flaps such as the medial plantar flap ensure adequate coverage of heel defects. The low risk of complications, the possibility of a ‘like with like’ reconstruction, and the scarce functional limitation related to the surgical procedure, represent the strengths of this flap.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
FUNDING
The authors received no financial support for the research, authorship, and/or publication of this article.
CONSENT
The patient provided written informed consent for surgery and use of pictures for academical and study purpose.



