-
PDF
- Split View
-
Views
-
Cite
Cite
Fanyi Wu, M Sung Lee, Daniel E Kim, Small bowel obstruction caused by hemorrhagic metastatic melanoma: case report and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac395, https://doi.org/10.1093/jscr/rjac395
Close - Share Icon Share
Abstract
Melanoma is one of the most common cancers and causes of death from skin cancer. It is also one of the most common malignancies to metastasize to the gastrointestinal tract. However, the incidence of gastrointestinal metastases from unknown primary cutaneous melanoma is reported to be 4–9%. Despite advances in diagnostic techniques, only 1.5–4.4% of metastases to the gastrointestinal tract are detected before death. We report a patient with no prior history of melanoma who presented with both gastrointestinal hemorrhage and small bowel obstruction. Diagnostic laparoscopy, followed by small bowel resection, was performed after a red blood cell radionuclide scan showed active hemorrhage. Pathologic examination confirmed metastatic melanoma of the jejunum. Additional small bowel resections were required for recurrent gastrointestinal bleeding, confirming two additional metastases. A review of the literature on small intestinal melanoma causing hemorrhage and obstruction is discussed.
INTRODUCTION
Small intestinal neoplasms are uncommon and are rarely observed in clinical practice. The incidence of small intestinal neoplasms is estimated to be 2.3 per 100 000 people in the USA, accounting for only 0.6% of all cancer diagnoses [1]. Secondary intestinal neoplasias are more common than primary small intestinal neoplasias. Melanoma is an extra-intestinal cancer with the highest tendency to spread to the intestine.
In the USA, melanoma is the fifth most prevalent cancer in both men and women [2]. More than 97% of melanomas are diagnosed with a known primary site, with the skin being the most common location [3]. Primary small bowel melanoma is rare, hence the paucity of published reports. The majority of gastrointestinal melanoma is hematogenous metastasis secondary to a primary lesion. Up to 50% of gastrointestinal metastases are caused by small bowel invasion [4]. The small intestine is the most common site of melanoma metastasis, primarily due to its abundant blood supply [5]. Although ~60% of melanoma patients who die have gastrointestinal metastases, only 1.5–4.4% of gastrointestinal metastases are detected before death [6, 7]. Small intestinal melanoma present with relatively nonspecific symptoms. Consequently, clinical detection rate is low, ranging between 10 and 20% [8]. Radiological studies have been used in diagnosing the small intestinal melanoma, however, imaging the small bowel is difficult because of its length and complex loops.
We report a patient with no history of melanoma, who presented with both gastrointestinal bleeding and small bowel obstruction, who was ultimately found to have multiple metastatic melanomas upon surgical exploration. We reviewed the literature on small intestinal melanoma causing hemorrhage and bowel obstruction.
CASE REPORT
A 71-year-old male active smoker with no prior colonoscopy or abdominal surgery presented to the emergency department after a fall with lightheadedness and dizziness. The patient reported fatigue and dyspnea on exertion for at least 10 weeks. He denied abdominal pain, bright red blood per rectum, melena or hematemesis. The initial hemoglobin was 5.7 g/dl, which increased to 7.7 after two units of red blood cell (RBC) transfusion. An iron panel test showed profound iron deficiency anemia. Gastroenterology was consulted and an endoscopic workup with esophagogastroduodenoscopy and colonoscopy was conducted in which no bleeding lesion was identified. Computed tomography (CT) of the chest, abdomen and pelvis showed multiple bilateral pulmonary nodules suspicious of pulmonary metastases and an enlarged left mesenteric lymph node. Carcinoembryonic antigen and carbohydrate antigen 19–9 were not elevated. Prostate-specific antigen was normal despite an enlarged prostate. Oncology consult recommended a positron emission tomography (PET) scan followed by an image-directed biopsy since the pulmonary nodules were not accessible by bronchoscopy. The gastroenterologist scheduled an outpatient small bowel video capsule endoscopy.
At the time of his PET scan, the patient acutely developed diffuse abdominal pain and vomiting. The scan was aborted and the patient was rushed to the emergency department. An abdominal X-ray and a CT scan of the abdomen and pelvis showed small bowel dilatation, but there was no intestinal mass lesion (Fig. 1). He was placed on nasogastric tube decompression. The patient reported having melena that morning. The hemoglobin was found to be 6.1 g/dl and a tagged RBC nuclear scan showed active gastrointestinal bleeding (Fig. 2) at the approximate location of the transition zone of the small bowel obstruction seen on CT.

CT of the abdomen and pelvis showing evidence of small bowel obstruction with dilated stomach and loops of the small intestine.
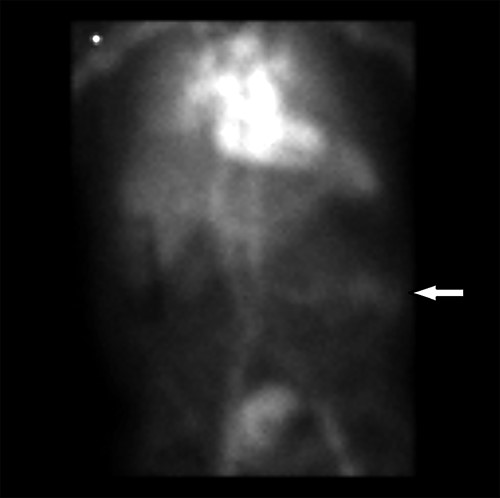
Radionuclide RBC scan showing active hemorrhage within the mid-small intestine (arrow).

An urgent diagnostic laparoscopy was performed during which a hyperchromic, obstructing mass in the ileum was found (Fig. 3). No additional intraabdominal lesions were visualized. The portion of small bowel was extracorporealized, resected, and a primary stapled anastomosis was performed. The specimen revealed malignant melanoma (Fig. 4), positive for Melan A and S100 immunostains (Fig. 5) and for BRAF V600K mutation. A PET scan was finally performed 3 days postsurgery in which increased uptake was seen in the left lateral abdomen and in multiple bilateral pulmonary nodules (Fig. 6). He was discharged to a rehabilitation center.

Resected portion of jejunum containing an obstructing melanoma metastasis.
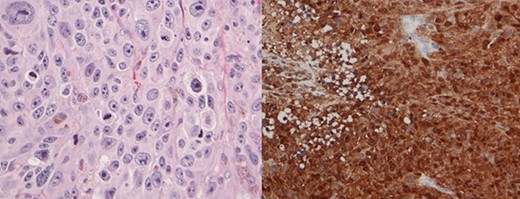
Histology slides showing nests of pleomorphic tumor cells with prominent nucleoli and cytoplasmic pigment (left); positive immunostaining of S-100 protein consistent with malignant melanoma (right).
Nine days after discharge, the patient returned to the emergency department for fatigue and melena and was found to have a hemoglobin level of 5.1 g/dl. A CT angiogram of the abdomen and pelvis was negative for arterial extravasation into the gastrointestinal tract. A tagged RBC scan showed active bleeding corresponding to the area of increased uptake on the previous PET scan within the small bowel, separate from the intestinal anastomosis. The patient returned to the operating room during which an exploratory laparotomy revealed two additional palpable solid masses in the jejunum, which were individually resected. The previous small bowel anastomosis appeared to be intact. As suspected, the additional small bowel specimens were consistent with metastatic malignant melanoma. The patient recovered well after surgery and is undergoing palliative immunotherapy.
DISCUSSION
Common presentations of small bowel melanomas include bowel obstruction, melena, anemia, abdominal pain, anorexia or weight loss [9]. Rarely do they present with both hemorrhage and obstruction. Three online databases, Web of Science, CINAHL and Ovid, were searched on 3 May 2022 for the keywords: melanoma, small intestine, bleeding or hemorrhage and obstruction. The queries were not filtered for publication year or language. The search initially produced 28 citations. Abstracts were reviewed and the list was narrowed to 22 articles. The full texts of the 22 articles were examined and an additional 13 were excluded. Cited references were screened and four additional studies were included. Thirteen studies reporting 17 total patients were found pertinent to our review.
The details of each patient are presented in Table 1. Patients’ ages ranged from 35 to 76, with a median age of 57. Adding our patient, there was an even distribution of females and males. Ten of the 17 cases had a known history of malignant melanoma. CT was the most common radiographic modality in our review. All CT imaging reported an abnormal finding of a mass or intussusception corresponding to the melanoma. Fourteen of the cases reported intussusception as the cause of obstruction. Furthermore, 13 patients had a single lesion, while 4 had multiple metastases within the small bowel. In addition to presenting with both gastrointestinal hemorrhage and bowel obstruction, our patient is further unique from these 17 cases because he had (i) no prior history of malignant melanoma, (ii) multiple CT scans showing no small bowel mass nor intussusception (although one CT showed dilated intestine) and (iii) multiple jejunal and pulmonary metastases.
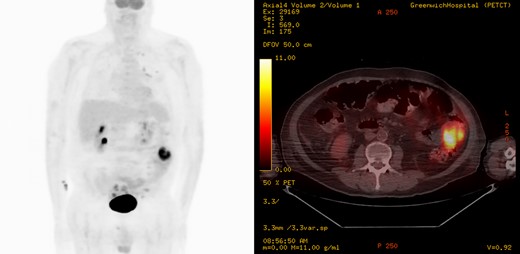
Coronal and axial images of a positron emission tomography showing high metabolic activity in the small intestine within the left lateral abdomen.
Melanoma is known to metastasize hematologically to the small intestine and should be highly suspected in patients who develop gastrointestinal symptoms [4, 10]. Since our patient did not have prior melanoma, he underwent a prolonged evaluation with multiple admissions until urgent surgery was ultimately indicated for hemorrhage and small bowel obstruction. Melanoma in the small intestine leads to gastrointestinal hemorrhage due to erosion of the intestinal mucosa [11]. Signs of hemorrhage range from chronic iron deficiency anemia, hemoccult positivity on rectal examination or melena. Evaluation for the source of gastrointestinal hemorrhage commonly consists of upper endoscopy and colonoscopy, however, they are limited from diagnosing jejunal or ileal tumors [12]. CT with arteriography may reveal active hemorrhage. After the CT arteriography showed no hemorrhage, intussusception or mass lesion, our patient underwent a tagged RBC radionuclide scan, which showed hemorrhage into the small intestine.
A tumor in the small intestine can act as a lead point, causing the intestine to invaginate into itself, creating an intussusception and bowel obstruction. Other mechanisms of obstruction are intraluminal narrowing by the space occupying mass or external compression by a mesenteric mass. Intussusceptions and masses are evident at the time of surgical exploration and typically in radiographic studies during the initial workup.
Case reports of patients with small intestinal melanoma presenting with gastrointestinal hemorrhage and bowel obstruction
| Publish Year . | Author . | Age . | Sex . | Prior site of melanoma . | Evidence of hemorrhage . | Radiographic study type . | Radiographic finding . | Evidence of bowel obstruction . | SB location . | Number of SB lesions . | Additional non-SB lesions . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia . | Melena . | Hemoccult positivity . | Vomiting . | Intestinal distention . | Intussusception . | ||||||||||
| 1964 | DasGupta [19] | 35 | F | Back | + | + | + | Ileum | Single | ||||||
| 37 | F | Maxilla, nasal cavity | + | + | Jejunum and ileum | Multiple | + | ||||||||
| 37 | F | Arm | + | + | Ileum | Single | |||||||||
| 73 | M | Stomach | + | UGI | Kinking, dilatation | + | + | Jejunum | Single | ||||||
| 1984 | Colombo [20] | 63 | M | Anorectal | + | + | Ileum | Multiple | + | ||||||
| 72 | M | Thigh | + | + | Ileum | Single | |||||||||
| 1996 | Kogire [21] | 57 | M | + | US, CT | Intussusception | + | + | Jejunum | Single | |||||
| 1999 | Hao [10] | 51 | M | Chest | + | UGI, US, CT | Mass | + | + | Ileum | Multiple | ||||
| 2007 | Karmiris [22] | 76 | F | + | + | CT, MRE | Mass | + | + | Ileum | Single | ||||
| 2007 | Resta [23] | 45 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| 2009 | Tarcoveanu [11] | 73 | M | + | + | + | Ileum | Single | |||||||
| 2010 | Kasza [24] | 65 | F | Forearm | + | + | CT | Masses | + | Ileum | Multiple | + | |||
| 2014 | Conversano [13] | 49 | M | Leg, cheek | + | + | CT | Mass | + | Jejunum | Single | + | |||
| 2017 | Vrable [5] | 51 | F | + | + | CT | Intussusception | + | + | + | Not specified | Single | |||
| 2019 | Mazzeo [25] | 71 | M | Scalp | + | + | CT | Mass | + | + | Ileum | Single | + | ||
| 2020 | Surjan [26] | 40 | F | + | + | CT | Mass | + | + | Duodenum | Single | ||||
| 2021 | Reddy [27] | 64 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| Publish Year . | Author . | Age . | Sex . | Prior site of melanoma . | Evidence of hemorrhage . | Radiographic study type . | Radiographic finding . | Evidence of bowel obstruction . | SB location . | Number of SB lesions . | Additional non-SB lesions . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia . | Melena . | Hemoccult positivity . | Vomiting . | Intestinal distention . | Intussusception . | ||||||||||
| 1964 | DasGupta [19] | 35 | F | Back | + | + | + | Ileum | Single | ||||||
| 37 | F | Maxilla, nasal cavity | + | + | Jejunum and ileum | Multiple | + | ||||||||
| 37 | F | Arm | + | + | Ileum | Single | |||||||||
| 73 | M | Stomach | + | UGI | Kinking, dilatation | + | + | Jejunum | Single | ||||||
| 1984 | Colombo [20] | 63 | M | Anorectal | + | + | Ileum | Multiple | + | ||||||
| 72 | M | Thigh | + | + | Ileum | Single | |||||||||
| 1996 | Kogire [21] | 57 | M | + | US, CT | Intussusception | + | + | Jejunum | Single | |||||
| 1999 | Hao [10] | 51 | M | Chest | + | UGI, US, CT | Mass | + | + | Ileum | Multiple | ||||
| 2007 | Karmiris [22] | 76 | F | + | + | CT, MRE | Mass | + | + | Ileum | Single | ||||
| 2007 | Resta [23] | 45 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| 2009 | Tarcoveanu [11] | 73 | M | + | + | + | Ileum | Single | |||||||
| 2010 | Kasza [24] | 65 | F | Forearm | + | + | CT | Masses | + | Ileum | Multiple | + | |||
| 2014 | Conversano [13] | 49 | M | Leg, cheek | + | + | CT | Mass | + | Jejunum | Single | + | |||
| 2017 | Vrable [5] | 51 | F | + | + | CT | Intussusception | + | + | + | Not specified | Single | |||
| 2019 | Mazzeo [25] | 71 | M | Scalp | + | + | CT | Mass | + | + | Ileum | Single | + | ||
| 2020 | Surjan [26] | 40 | F | + | + | CT | Mass | + | + | Duodenum | Single | ||||
| 2021 | Reddy [27] | 64 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
Abbreviations: MRE = magnetic resonance enterography, SB = small bowel, UGI = upper gastrointestinal series, US = ultrasound.
Case reports of patients with small intestinal melanoma presenting with gastrointestinal hemorrhage and bowel obstruction
| Publish Year . | Author . | Age . | Sex . | Prior site of melanoma . | Evidence of hemorrhage . | Radiographic study type . | Radiographic finding . | Evidence of bowel obstruction . | SB location . | Number of SB lesions . | Additional non-SB lesions . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia . | Melena . | Hemoccult positivity . | Vomiting . | Intestinal distention . | Intussusception . | ||||||||||
| 1964 | DasGupta [19] | 35 | F | Back | + | + | + | Ileum | Single | ||||||
| 37 | F | Maxilla, nasal cavity | + | + | Jejunum and ileum | Multiple | + | ||||||||
| 37 | F | Arm | + | + | Ileum | Single | |||||||||
| 73 | M | Stomach | + | UGI | Kinking, dilatation | + | + | Jejunum | Single | ||||||
| 1984 | Colombo [20] | 63 | M | Anorectal | + | + | Ileum | Multiple | + | ||||||
| 72 | M | Thigh | + | + | Ileum | Single | |||||||||
| 1996 | Kogire [21] | 57 | M | + | US, CT | Intussusception | + | + | Jejunum | Single | |||||
| 1999 | Hao [10] | 51 | M | Chest | + | UGI, US, CT | Mass | + | + | Ileum | Multiple | ||||
| 2007 | Karmiris [22] | 76 | F | + | + | CT, MRE | Mass | + | + | Ileum | Single | ||||
| 2007 | Resta [23] | 45 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| 2009 | Tarcoveanu [11] | 73 | M | + | + | + | Ileum | Single | |||||||
| 2010 | Kasza [24] | 65 | F | Forearm | + | + | CT | Masses | + | Ileum | Multiple | + | |||
| 2014 | Conversano [13] | 49 | M | Leg, cheek | + | + | CT | Mass | + | Jejunum | Single | + | |||
| 2017 | Vrable [5] | 51 | F | + | + | CT | Intussusception | + | + | + | Not specified | Single | |||
| 2019 | Mazzeo [25] | 71 | M | Scalp | + | + | CT | Mass | + | + | Ileum | Single | + | ||
| 2020 | Surjan [26] | 40 | F | + | + | CT | Mass | + | + | Duodenum | Single | ||||
| 2021 | Reddy [27] | 64 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| Publish Year . | Author . | Age . | Sex . | Prior site of melanoma . | Evidence of hemorrhage . | Radiographic study type . | Radiographic finding . | Evidence of bowel obstruction . | SB location . | Number of SB lesions . | Additional non-SB lesions . | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anemia . | Melena . | Hemoccult positivity . | Vomiting . | Intestinal distention . | Intussusception . | ||||||||||
| 1964 | DasGupta [19] | 35 | F | Back | + | + | + | Ileum | Single | ||||||
| 37 | F | Maxilla, nasal cavity | + | + | Jejunum and ileum | Multiple | + | ||||||||
| 37 | F | Arm | + | + | Ileum | Single | |||||||||
| 73 | M | Stomach | + | UGI | Kinking, dilatation | + | + | Jejunum | Single | ||||||
| 1984 | Colombo [20] | 63 | M | Anorectal | + | + | Ileum | Multiple | + | ||||||
| 72 | M | Thigh | + | + | Ileum | Single | |||||||||
| 1996 | Kogire [21] | 57 | M | + | US, CT | Intussusception | + | + | Jejunum | Single | |||||
| 1999 | Hao [10] | 51 | M | Chest | + | UGI, US, CT | Mass | + | + | Ileum | Multiple | ||||
| 2007 | Karmiris [22] | 76 | F | + | + | CT, MRE | Mass | + | + | Ileum | Single | ||||
| 2007 | Resta [23] | 45 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
| 2009 | Tarcoveanu [11] | 73 | M | + | + | + | Ileum | Single | |||||||
| 2010 | Kasza [24] | 65 | F | Forearm | + | + | CT | Masses | + | Ileum | Multiple | + | |||
| 2014 | Conversano [13] | 49 | M | Leg, cheek | + | + | CT | Mass | + | Jejunum | Single | + | |||
| 2017 | Vrable [5] | 51 | F | + | + | CT | Intussusception | + | + | + | Not specified | Single | |||
| 2019 | Mazzeo [25] | 71 | M | Scalp | + | + | CT | Mass | + | + | Ileum | Single | + | ||
| 2020 | Surjan [26] | 40 | F | + | + | CT | Mass | + | + | Duodenum | Single | ||||
| 2021 | Reddy [27] | 64 | F | + | + | CT | Intussusception | + | + | Jejunum | Single | ||||
Abbreviations: MRE = magnetic resonance enterography, SB = small bowel, UGI = upper gastrointestinal series, US = ultrasound.
CT, PET-CT scan and video capsule endoscopy are recommended for evaluating patients with melanoma history and gastrointestinal symptoms [13]. Contrast-enhanced CT remains one of the most effective preoperative tools for assessing small bowel obstruction [14]. However, CT imaging’s sensitivity to detect intestinal melanoma was only between 60 and 70% [15]. Whole-body PET scan with fluorodeoxyglucose has a higher sensitivity and specificity than conventional CT for detecting gastrointestinal metastases in melanoma patients [16]. In fact, some researchers believe that PET should be the primary staging test for disease recurrence [17]. Capsule endoscopy can examine segments of the intestine which are inaccessible to conventional endoscopy. Capsule endoscopy complements cross-sectional imaging and has greater diagnostic validity than CT and small bowel radiography for identifying the presence and extent of small bowel metastases [18]. Our patient was scheduled for both outpatient video capsule endoscopy and PET scan, but these were canceled due to the onset of acute abdominal pain and bowel obstruction.
In conclusion, our case report demonstrates that despite advancements in diagnostic techniques, early detection of small bowel melanoma continues to be a challenge. It is even more confounding when the patient does not have a history of melanoma. A combination of imaging techniques is recommended as a precise preoperative assessment of the extent of small bowel metastases is crucial for surgical planning [15]. Resection of gastrointestinal melanomas is the treatment of choice for the relief of symptoms and avoidance of future complications even if curative surgery is impossible [4, 19].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was received to assist with the preparation of this manuscript.
CONSENT STATEMENT
Written informed consent was obtained from the patient for the publication of this case report.
References
- positron-emission tomography
- radionuclide imaging
- small bowel obstruction
- hemorrhage
- bowel resection
- cancer
- erythrocytes
- gastrointestinal bleeding
- cause of death
- diagnostic techniques and procedures
- intestine, small
- laparoscopy
- melanoma
- neoplasm metastasis
- jejunum
- metastatic melanoma
- red blood cell scintigraphy
- skin cancer
- small-intestine resection
- gastrointestinal tract
- malignant melanoma, cutaneous
- secondary malignant neoplasm of gastrointestinal tract



