-
PDF
- Split View
-
Views
-
Cite
Cite
Chung-Wei Wu, Tsen-Long Yang, Spleen metastasis of recurrent malignant thymoma, Journal of Surgical Case Reports, Volume 2022, Issue 8, August 2022, rjac375, https://doi.org/10.1093/jscr/rjac375
Close - Share Icon Share
Abstract
Thymoma is a rare tumour that often occurs in the anterior mediastinum. Thymomas are usually diagnosed in middle-aged patients, and nearly half of cases are associated with myasthenia gravis. Thymomas typically progress through direct invasion of the thoracic cavity with extra-thoracic distant metastasis being uncommon. Here we report the case of a male patient who underwent an extensive thymectomy and radiotherapy 10 years before presentation, and in whom we detected a spleen tumour during regular out-patient follow-up. The patient underwent a splenectomy, and a final diagnosis of type B3 malignant thymoma was established.
INTRODUCTION
Thymoma is a rare tumour that often occurs in the anterior mediastinum. Thymomas typically progress slowly, with extra-thoracic metastasis being extremely rare. Only a few cases of thymoma have been reported. Here we present the case of a 49-year-old man who was diagnosed with a recurrent metastatic spleen thymoma; the patient had undergone an extensive thymectomy and radiotherapy 10 years prior. During regular follow-up, a tumour was detected, and therefore, a splenectomy was performed to confirm the diagnosis.
CASE PRESENTATION
A 49-year-old man with a history of myasthenia gravis and malignant thymoma had undergone radiotherapy and an extensive thymectomy in 2011. However, 2 years later, an abnormality was detected on a chest computed tomography (CT) scan, a suspicion of recurrent thymoma. Surgical resection at that time revealed only fibrosis according to the pathology report. An outpatient follow-up within 2 years after surgery revealed an increase in the patient’s acetylcholine receptor antibody levels from 79.5 to 107.12 nmole/L. In December 2021, follow-up CT scan (Fig. 1) revealed a lobulated, less enhanced mass measuring 5.8 × 5.3 cm in the patient’s spleen, along with mixed osteoblastic and osteolytic lesions in the L1 and L3 vertebral bodies. These findings prompted the suspicion of spleen and bone metastasis. Therefore, the patient was referred to our general surgeon and underwent splenectomy in January 2022.
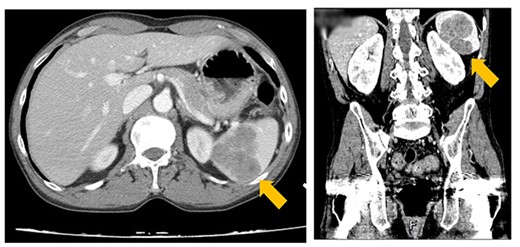
CT image showing a lobulated, less-enhanced mass measuring 5.8 × 5.3 cm in the patient’s spleen, prompting the suspicion of splenic metastasis.
The specimen (Fig. 2) measured 9.0 × 6.0 × 4.5 cm3 and weighed 149.87 g. Two tumours were detected in the spleen, measuring 6.5 × 4.0 × 3.6 cm3 and 5.0 × 4.0 × 4.0 cm3, respectively. Large epithelioid cells admixed with focal small lymphoid cells were also detected, compatible with a type B3 thymoma.
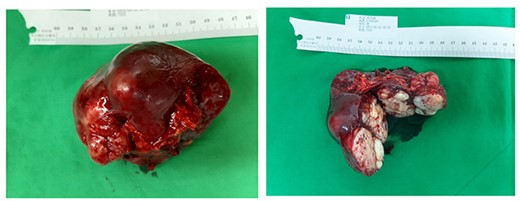
Specimen measuring 9.0 × 6.0 × 4.5 cm3 (spleen) with two encapsulated tumours.
Immunohistochemical staining of the epithelioid cells (Fig. 3) revealed positive staining for p40 and negative staining for CD5 and CD117. In addition, terminal deoxynucleotidyl transferase (TdT) indicated abundant focal immature T cells.
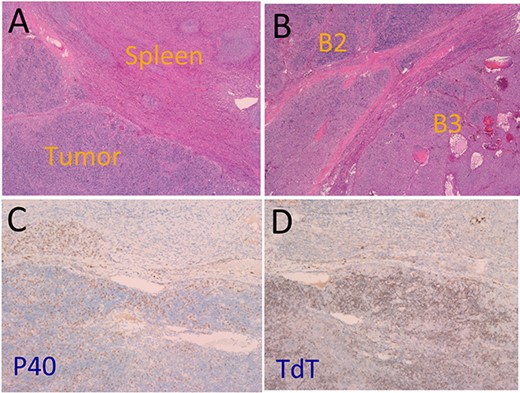
(A) Tumour (lower left) and spleen tissue (upper right). (B) Type B2 thymoma (upper left) and type B3 thymoma (lower right). (C) Positive staining P40. (D) Positive staining for TdT.
After the surgery, the patient experienced an uneventful recovery process and was discharged 10 days later.
DISCUSSION
Metastatic spleen thymoma is rare in clinical practice. Diagnosing thymic metastasis is a challenging task because of the rarity of extrathoracic metastasis (~3–6% incidence rate [1]) polymorphic difficulties in histology. In a study of 283 patients with thymoma, Lewis [2] reported that only eight of them (3%) developed extrathoracic distant metastasis. In another study, Nickels and Franssila [3] reviewed 29 case reports and concluded that the epithelial subtype of metastatic thymoma was the most common type (67%).
The most common sites of metastasis are the lymph nodes, liver, bone, brain, spleen, kidneys, pancreas, gastrointestinal tract, ovary and other soft tissues. This is in line with the study of Tudor who concluded that the liver, lymph nodes and soft tissues are the most frequent sites of metastasis. Only a few reports of splenic metastasis in cases of thymic carcinoma have been documented [5–7].
In the previously mentioned study, Tudor indicated that the most common subtype of thymoma that presents with metastasis is type B thymoma. This is because in type B thymoma, the lymphocytes are all immature (positive CD1a, TdT, and CD99). Furthermore, depending on the site of metastasis, diagnosing metastatic type B3 thymoma is particularly difficult compared with other subgroup thymomas because of the poor lymphocyte content and the presence of focal CD5 [8]. The histological results of our patient revealed a lesion with negative CD5 staining. Only P40 and TdT displayed positive staining, confirming the squamous cell carcinoma cell origin [4].
According to the guidelines of the National Comprehensive Cancer Network [7] (revised in 2014), complete tumour removal is recommended for resectable thymomas. In addition, radiation therapy, chemotherapy and/or postoperative adjuvant therapy may be appropriate depending on the stage. In a review study, Paolo [9] included the following stages of thymoma as resectable thymomas: Masaoka I, II and III and IASLC/ITMIG TNM I, II and IIIA/T3. Patients with stage IV mainly receive radiotherapy or chemotherapy.
Although chemotherapy is the primary therapeutic approach in the case of metastasis, no standard regimen had been developed. For patients with metastatic thymoma. Currently, platinum-based chemotherapy with anthracyclines is regarded as the regimen of choice. However, in a retrospective study, Ströbel et al. [10] indicated that adjuvant chemotherapy does not improve the prognosis of malignant thymoma. In addition, no compelling evidence supports the benefit of targeted therapy [9]. Our patient received further adjuvant chemotherapy and targeted therapy after surgery for disease control.
CONCLUSION
Splenic metastasis of a type B3 malignant thymoma is extremely rare. The treatment plan depends mainly on the stage. The main approach is to surgically remove resectable tumours first and then to use a combination of platinum-based chemotherapy and radiotherapy. Systemic treatment is the main goal for patients with stage IV disease, although the weight of evidence concerning efficacy remains relatively weak.
CONFLICT OF INTEREST STATEMENT
None declared.



