-
PDF
- Split View
-
Views
-
Cite
Cite
Raheel Ahmad, Marco Baia, David N Naumann, Fahad Mahmood, Fabio Tirotta, Samuel Ford, Anant Desai, Max Almond, Emergency multivisceral resection for spontaneous haemorrhage rupture of huge solid pseudopapillary neoplasm of the pancreas during pregnancy, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac331, https://doi.org/10.1093/jscr/rjac331
Close - Share Icon Share
Abstract
Solid pseudopapillary neoplasm (SPN) of the pancreas is a rare malignancy with a low malignant potential and strong female preponderance. Diagnosis during pregnancy is extraordinary, and management must consider the risks to the mother and foetus of tumour growth and rupture. A large 35-cm SPN was identified on magnetic resonance imaging (MRI) in a 24-year-old woman at 6 weeks of gestation following presentation with an abdominal mass. Surgery was delayed to allow the foetus to reach as close to term as possible because surveillance MRIs showed incremental mass growth. Emergency c-section was undertaken at 35 weeks of gestation due to persistent tachycardia and suspected haemorrhage into the tumour. A Hb of 70 g/l post-delivery despite four units of RBCs and an albumin of 11 g/l necessitated urgent multivisceral surgery. Surgical resection is the mainstay of treatment for SPN. However, the strategy of choice during pregnancy remains undetermined, with more recent reports delaying surgery until post-partum.
INTRODUCTION
Solid pseudopapillary neoplasm (SPN) of the pancreas is a rare malignant tumour, accounting for ~2.7% of all exocrine and ~3.4% of all pancreatic cystic neoplasms [1, 2]. It typically presents in women, with an 87.8% predominance, during the second and third decades of life [3]. Most cases are discovered incidentally on radiological imaging because symptoms of SPN are generally non-specific with abdominal pain or discomfort being the most common complaint.
Surgical resection is the mainstay of treatment, with a reported curative rate >95% and 5-year survival of 95% [1, 4]. SPN is defined by a low malignant potential, with tumour recurrence or metastasis arising in only 10–15% of cases [5]. Long-term survival, even in the event of metastasis, has been described in the literature [6].
The occurrence of SPN during pregnancy is extraordinary with only a few reports in the literature. Tumour growth is heightened during pregnancy and the risk of spontaneous rupture is of great concern to both the mother and foetus [7]. There is currently no consensus regarding the optimal management of SPN during pregnancy. We report the successful surgical treatment of the largest SPN, to our knowledge, detected during pregnancy. Management was further complicated by an acute, active haemorrhage into the tumour during pregnancy.
CASE REPORT
A 24-year-old woman of 6-week gestation (gravida II, para I) was referred to her local hospital following complaint of an abdominal mass on her left side for ~1 month. A magnetic resonance imaging (MRI) demonstrated a 203 × 134 × 240 mm soft tissue mass in her left upper quadrant, sitting between her left kidney and spleen, and displacing the tail of her pancreas. The appearances were concerning for a malignant retroperitoneal sarcoma. An urgent biopsy showed a low-grade spindle cell lesion, most likely consistent with features of SPN.
The patient was referred to the regional sarcoma MDT and a further MRI was organised at a 6-week interval to determine the rate of tumour growth. There was minimal interval change in the appearance and size of the tumour, so the consensus opinion at the MDT was to continue surveillance during the pregnancy and delay surgery until the post-partum period. A further two surveillance MRIs were undertaken at 2-month intervals and demonstrated small incremental enlargements (Fig. 1). The plan was to reach 38 weeks of gestation, deliver the baby and excise the tumour a few weeks afterwards, guaranteeing the best chance of survival for both the mother and newborn.
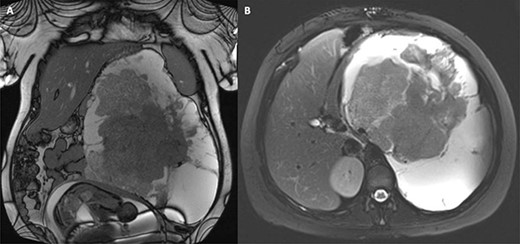
MRI surveillance scan 6 months after diagnosis at 33 weeks of gestation; the tumour and gravid uterus are evident in the coronal view (A), and the tumour occupies the whole left upper quadrant in the axial view (B).
Contrary to the initial plan, the patient was admitted to her local hospital for tachycardia after the last surveillance MRI. She required an emergency caesarean section at 35 weeks of gestation due to suspected haemorrhage into the tumour. After the delivery, she was physiologically unstable, with sinus tachycardia (155 beats/minute), low albumin (11 g/l) and low haemoglobin (70 g/l) despite four units of blood transfusion. A computed tomography (CT) TAP with contrast concluded active haemorrhage into the mass, but no haemoperitoneum, and confirmed the absence of metastatic disease. A CT angiogram was subsequently organised, but embolization was abandoned due to abnormal blood supply arising from the origin of the aorta.
She was transferred to ICU at the regional sarcoma centre and was taken to theatre as an emergency case. The tumour was resected from her left retroperitoneum en bloc with the pancreatic body and tail (site of origin), spleen, a portion of the greater curvature of the stomach, left kidney and adrenal gland, the splenic flexure of the colon and a cuff of the left diaphragm. Simple excision was attempted but was abandoned in favour of multivisceral resection to preserve the integrity of the tumour and avoid spillage of cancerous cells, allowing the best chance of curative excision. Histopathology confirmed a large (35 cm, 8 kg) SPN which had been completely excised with clear margins (Fig. 2).
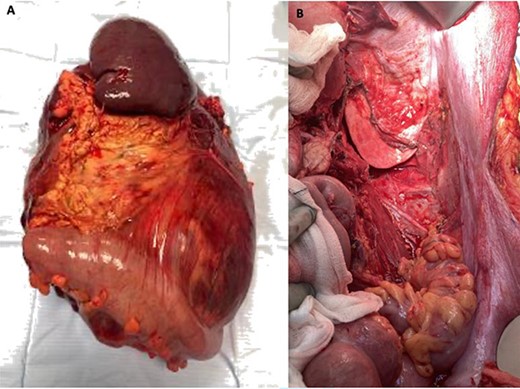
Peri-operative images showing (A) fresh specimen from multivisceral resection with spleen, pancreas and colon clearly visible, and (B) operative field after resection.
The patient made an excellent recovery and was discharged on Day 22 following surgery. The only post-operative complication was a non-occlusive thrombus with associated infection and pyrexia in the right internal jugular vein, related to her intravenous central catheter.
A baseline post-operative CT at a 3-month interval showed no evidence of tumour recurrence or residual disease. She is now on an ongoing surveillance programme for the next 5 years.
DISCUSSION
Complete surgical excision, including resection of metastases, when possible, is the established standard of care for SPN and has been shown to lead to long-term survival [5]. In a minority of cases, the tumour may recur or metastasise (usually to the liver, peritoneum or lymph nodes) [1], and there have been reports in the literature seeking to identify potential markers to predict aggressive disease behaviour. Proposed predictive factors include tumour size, perineural invasion, angioinvasion, deep infiltration of surrounding structures and Ki-67 proliferative index [8]. However, at present, there is a lack of agreement between the studies.
There are currently no guidelines on the optimal management of SPN during pregnancy. In the literature, there have been only 14 reported cases of pregnancy complicated by SPN [9]. In 10 of the reported cases, surgery was performed during pregnancy, with 1 unsuccessful case that led to spontaneous abortion [10]. All four cases where surgery was performed after delivery, or termination in one case [11], were successful. In two cases, the patients opted for a termination of pregnancy [11, 12]. Spontaneous rupture was documented in one case [13]. Metastasis with tumour recurrence was reported in another case [9], and there were no reports of intrauterine growth restriction. In 11 of the cases which resulted in delivery, all the infants made good developmental progress.
In our case, the tumour was detected relatively early as the patient was symptomatic and it had already grown to a considerable size. The benefits and risks of surgery during pregnancy were discussed in an MDT and with the patient, and a decision was made to delay surgery. However, the tumour ruptured spontaneously following emergency delivery, necessitating further emergency laparotomy and multivisceral surgery. There was no foetal impairment, and both the mother and baby are doing well.
In conclusion, surgery is the established treatment with good prognosis, but there is still some uncertainty regarding the optimal surgical strategy and timing during pregnancy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was received for this publication.
References
Author notes
This paper is not based on a previous communication to a society or meeting.
- pregnancy
- tachycardia
- magnetic resonance imaging
- abdominal mass
- hemorrhage
- albumins
- cancer
- cesarean section
- fetus
- mothers
- rupture
- surgical procedures, operative
- diagnosis
- neoplasms
- pancreas
- surgery specialty
- persistence
- tumor growth
- surveillance, medical
- solid pseudopapillary tumor of the pancreas
- excision
- retail clinics
- borderline neoplasms



