-
PDF
- Split View
-
Views
-
Cite
Cite
Luca Domenico Bonomo, Marcello Zago, Claudia Quirico, Antonio Ottinetti, Filippo Panzera, Alessandra Galli, Luca Gattoni, Gualtiero Canova, Antonella Nicotera, Surgical rarities: case report of appendicular diverticulitis and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 7, July 2022, rjac319, https://doi.org/10.1093/jscr/rjac319
Close - Share Icon Share
Abstract
Appendicular diverticulosis is a rare condition observed in about 0.004–2% of all appendectomy specimens. Risk of perforation/bleeding is high and a relevant association with mucinous neoplasms is known. Appendectomy is indicated even in case of occasional finding. We present the case of a 22-year-old man who entered the Emergency Room for pain in right iliac fossa. Blood tests showed only a slight increase in C-reactive protein. Abdominal ultrasound (US) evidenced an appendix with thickened walls and a rounded fluid-filled hypoechoic lesion at its distal tip. Laparoscopic appendectomy confirmed the presence of mucocele. Postoperative course was uneventful and the patients discharged on postoperative day 3. Histological examination indicated diverticulitis/peridiverticulitis of the appendix and acute suppurative appendicitis. No perforation of the diverticula was detected. No neoplastic epithelium/mucous material was observed. In our case, preoperative US proved to be a useful alternative to computed tomography for the diagnosis.
INTRODUCTION
Appendicular diverticulosis is a rare entity reported only in 0.004–2% of all appendectomy specimens [1]. Patients are typically asymptomatic. In fact, the anomaly is often found intraoperatively in case of acute appendicitis or during imaging exams. Patients with appendicular diverticulitis (AD) tend to be older than patients with classic acute appendicitis (mean age of 38.8 years vs. 19.5 years, respectively) and the pain may be more discontinuous and non-specific [1, 2]. Occasional finding of this condition requires elective surgery due to the risk of bleeding, perforation and malignancy [3, 4].
CASE REPORT
We present the case of a 22-year-old man with a history of aortic coarctation previously treated with angioplasty. The patient entered the Emergency Room on February 2022 due to pain in right iliac fossa started the day before. Medical examination showed the presence of McBurney’s sign. No fever or vomit was reported. Adult Appendicitis score was 14 (intermediate risk of appendicitis). Blood tests only indicated a slight increase in C-reactive protein (0.71 mg/dL). Abdominal ultrasound (US) revealed an appendix with diameter of 10 mm, thickened walls, a rounded image filled with liquid at the distal tip and minimal periappendicular fluid collection (Fig. 1). Computed tomography (CT) scan was not necessary. In consideration of symptoms and US results, suggesting acute appendicitis, the patient underwent laparoscopic appendectomy. The diagnosis of acute appendicitis was confirmed intraoperatively. A mucocele of the distal tract of the appendix was observed, according to US report. Meckel’s diverticulum was not found. Bowel opening to stool occurred on postoperative day (POD) 3 and oral intake was resumed on POD 1. Postoperative course was uneventful and the patient discharged on POD 3. Histological examination reported a specimen of 6 cm in length, with diverticulitis/peridiverticulitis of the appendix and acute suppurative appendicitis (Fig. 2). Three diverticula were observed with the following maximum diameter: 9 mm (distal tip with abscess), 6 mm and 4 mm (distal appendix).
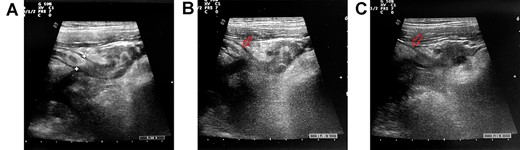
The abdominal US evidences a thickened appendix with circular protrusion at its distal tip (A). Periappendicular collection is visible (B–C, red arrow indicates the appendix).
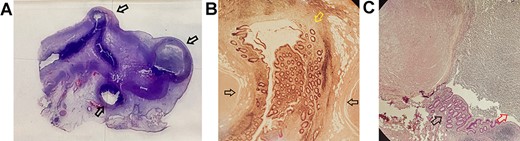
The histological section indicates the presence of three diverticula (A): the more distal one, with an abscess inside the lumen, of 9 mm and the other two (distal appendix) of 6 and 4 mm in diameter (black arrows indicate the diverticula). (B) The protrusion of the mucosa (pointed in yellow) through the muscular layer (pointed in black) in the bigger diverticulum. (C) The abscess in the largest diverticulum is pointed in red (black arrow indicates the mucosa).
DISCUSSION
AD is an uncommon condition whose clinical significance is relevant, since the risk of complications is greater than in classic acute appendicitis [5, 6]. Diverticula of the vermiform appendix were first described in 1893. They are more common in men and typically represent an acquired condition (pseudodiverticula) [1], with protrusion of mucosa/submucosa through the appendix wall. Congenital forms (full-thickness protrusion) are even more rare, reported in 1% of appendicular diverticula on a series of 50 000 appendectomies [7]. Acquired appendicular diverticula could originate from mucosa protrusion through a ‘locus minoris resistentiae’ at the level of a vascular hiatus. The pathophysiology of appendiceal diverticulitis is the same known for colonic diverticulitis: lumen obstruction induced by solid or fluid material determines inflammation of the thin diverticular walls and associates with higher perforation rate (30–66%) [8–10].
Preoperative diagnosis may be difficult during acute inflammation and CT represents the exam of choice to point out characteristic patterns. Osada et al. [8] reported preoperative multidetector CT diagnosis of appendicular diverticula in 6 out of 156 patients who underwent appendectomy. A total of 7 patients received a diagnosis of AD at histological examination. Therefore, in a single case, CT scan was not able to detect this condition. At CT investigation, appendicular diverticula appear as an out-pouching from the appendix. Inflamed diverticula present with thickened walls or enhanced solid mass [8]. Diverticular lumen may be air-filled or fluid-filled. Radiologists should also indicate the number of diverticula and their localization (distal, mid, proximal tract of the appendix). In their study, Osada et al. observed a mean diameter of 7.0 mm with the most common location in the middle segment of the appendix. Appendicular diverticula may also be classified into four morpholog-ical types [8, 11]. Our case can be referred to type 2: acute appendicitis with acute diverticulitis. The other types include diverticulitis without appendicitis (type 1), appendicitis and diverticula (type 3), appendix with diverticula (type 4).
Although CT scan represents the best radiological exam for the characterization of this condition, experiences with US are available in the literature [12, 13]. Kubota et al. [12] reported the US diagnosis of AD in a 30-year-old female. US scan revealed an enlarged appendix with multiple hypoechoic lateral small pouch-like projections. The surrounding fatty tissue appeared hyperechoic due to inflammation of the mesoappendix. Iki et al. [13] also reported the case of appendiceal diverticulitis diagnosed with US scan. In this 84-year-old man images showed an appendix of 20 mm on cross section surrounded by protruding outpouches. These rounded projections appeared as hypoechoic lesions with thin hyperechoic border in the periphery. In our case, US showed the presence of a single circular hypoechoic protrusion at the distal tip of the appendix, intraoperatively described as a mucocele. Surrounding hyperechogenic fatty tissue and fluid collection were also present, confirming the characteristics indicated by the aforementioned authors.
The clinical relevance of appendicular diverticula lies in the risk of bleeding, perforation and neoplastic transformation. Need for transfusion is reported in the literature [14]. Furthermore, an association with adenocarcinoma, mucinous neoplasms, benign neural lesions and even cystic fibrosis has been observed [15]. In particular, low-grade mucin-producing tumors may lead to pseudomyxoma peritonei, a condition characterized by intraperitoneal mucin with or without the presence of secreting epithelium and often fibrous tissue. Lamps et al. [15] reported 8 low-grade mucinous neoplasms out of 19 cases (42%) with appendicular diverticulum. Neoplastic epithelium was present within diverticular layer in all cases. In a single case, pseudomyxoma peritonei was described during appendectomy. In this specimen, a rupture of the diverticulum occurred. In our case, intraoperative abdominal exploration did not evidence mucin outside the appendix. Histological examination did not show any neoplastic epithelium nor the presence of mucinous material. No signs of perforation were found.
In conclusion, AD is a rare condition with relevant risk of concomitant mucinous neoplasm. In case of accidental finding of appendicular diverticula, elective appendectomy is mandatory due to high risk of perforation and bleeding. CT scan is the ‘gold standard’ for the diagnosis and typing of these lesions. US scan in favorable circumstances may lead to diagnosis, even if smaller diverticula may be difficult to detect.
AUTHOR CONTRIBUTIONS
Data acquisition: Bonomo, Nicotera, Quirico, Ottinetti, Canova, Zago, Panzera, Galli, Gattoni
Drafting of manuscript: Bonomo, Nicotera
Critical revision of manuscript: Bonomo, Nicotera, Zago, Canova, Panzera, Ottinetti
RESEARCH INVOLVING HUMAN PARTICIPANTS AND/OR ANIMALS
The study has been performed in accordance with the ethical standards of the Declaration of Helsinki and its later amendments.
FUNDING/SUPPORT
None.
FINANCIAL DISCLOSURES
We have no financial disclosures.
DECLARATION OF COMPETING INTEREST
Authors have no competing interests.
ETHICAL APPROVAL
The study is not a clinical trial. Ethical Committee approval and registration were not required.
INFORMED CONSENT
The patient has given informed consent to the processing of personal data, including consent to the use of health data and images for scientific purposes.
References
- appendicitis
- computed tomography
- hemorrhage
- blood tests
- appendectomy
- epithelium
- diverticulitis
- diverticulum
- emergency service, hospital
- ilium
- mucocele
- mucus
- pain
- preoperative care
- suppuration
- surgical procedures, operative
- c-reactive protein
- diagnosis
- neoplasms
- diverticulosis
- abdominal ultrasonography
- appendectomy, laparoscopic



