-
PDF
- Split View
-
Views
-
Cite
Cite
Matthew G Alben, Neil Gambhir, Mandeep S Virk, Isolated infraspinatus musculotendinous junction tear treated with open repair and dermal allograft augmentation: a case report with 5-year outcome, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac269, https://doi.org/10.1093/jscr/rjac269
Close - Share Icon Share
Abstract
We report the 5-year outcome of an isolated, atraumatic full-thickness infraspinatus myotendinous junction tear treated with open surgical repair. The index patient developed severe pain and weakness in external rotation strength following a subacromial corticosteroid injection. Magnetic resonance imaging and ultrasound of the shoulder demonstrated a full-thickness myotendinous junction tear with extensive muscle edema, mild atrophy and a spinoglenoid notch varix. Due to persistent, worsening pain and presence of ER weakness, the patient underwent primary infraspinatus muscle–tendon repair with allograft augmentation via an arthroscopic-assisted open posterior approach. The patient had an uneventful postoperative course with a resolution of pain and improvement in ER strength, which is maintained at the latest 5-year follow-up. This case report highlights a favorable long-term outcome of an isolated infraspinatus myotendinous junction tear treated with primary muscle–tendon repair and dermal allograft augmentation.
INTRODUCTION
Although rotator cuff tears (RCTs) are among the most common sources of shoulder pain, isolated infraspinatus (IS) tears are relatively uncommon [1, 2]. Such tears are typically atraumatic in etiology and have peculiar imaging findings of muscle edema, often in conjunction with considerable fatty infiltration [1, 3]. Moreover, RCTs at the myotendinous junction (MTJ) are an atypical variant that continues to be a challenge when treating.
Herein, we describe the 5-year postoperative outcome of an isolated MTJ tear of the IS following arthroscopic-assisted open muscle–tendon repair with allograft augmentation via a posterior open approach. The patient reported resolution of her shoulder pain symptoms with external rotation (ER) strength recovery that has persisted as of her latest 5-year follow-up visit. The patient provided consent for data concerning the case to be submitted for publication.
CASE REPORT
History and preoperative findings
The index patient is a 52-year-old, right-hand dominant female with a history of right shoulder pain for 1 year. Initial physical examination was remarkable for full range of motion (ROM) and 5/5 rotator cuff strength. She was initially treated with physical therapy and a subacromial steroid injection, returning for a second steroid injection for pain recurrence 5 months later. After the second injection, she reported an acute exacerbation of shoulder pain originally treated as a steroid flare reaction. However, further imaging was obtained due to persistent shoulder pain and noted weakness in her arm. MRI and ultrasound sonography demonstrated a complete tear of IS MTJ with a fluid-filled gap, edema and mild muscle atrophy (Fig. 1A and B), in addition to a venous varix in the spinoglenoid (SG) notch (Fig. 1C). Given the unremitting pain and shoulder weakness despite conservative therapy, the patient elected for surgical repair 5 months after acute worsening of symptoms (Fig. 2A).
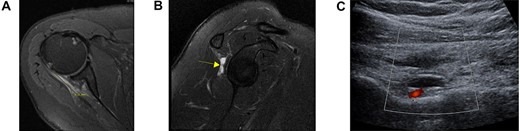
Axial (A) and sagittal (B) views of the preoperative MRI demonstrating a full-thickness tear at the level of the myotendinous junction with a fluid-filled gap (yellow arrow) and distal infraspinatus tendon stump attachment on the greater tuberosity. Ultrasound demonstrating a large, well-circumscribed hypoechoic lesion ultimately diagnosed as a venous varix adjacent to the suprascapular artery (C).

Preoperative (A) and postoperative (B) clinical photograph of the patient’s posterior right shoulder at the 5-year follow-up visit.
Surgical treatment and postoperative care
Diagnostic arthroscopy demonstrated a retracted IS tear at the MTJ region (Fig. 3A). The tear site was tagged with a suture arthroscopically for the ease of identification via a posterior open approach (Fig. 3B). After arthroscopy, a 6-cm skin incision starting from the posterolateral corner of the acromion towards the axilla was made. Deltoid split was performed along the posterior raphe to expose the underlying IS muscle and tendon. The MTJ tear was easily identified by the marking sutures placed arthroscopically. High strength, nonresorbable sutures (#2 Fiberwire; Arthrex Inc, Naples, FL) were passed through the tendon and muscle stump in a Mason–Allen configuration across the tear. A patch of dermal allograft matrix (Arthrex Inc, Naples, FL) was placed over the repair, anchored to the tendon and muscle side with interrupted sutures (Fig. 3C). Passive intraoperative shoulder motion demonstrated the IS muscle–tendon unit to move as a single unit.
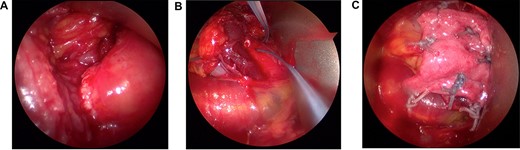
The infraspinatus tear at the myotendinous junction was identified arthroscopically (A) and tagged with a suture to ease identification during open repair (B). Following muscle to tendon repair across the tear in a Mason–Allen configuration, the repair was reinforced with a dermal allograft patch incorporated over the tear (C).
The arm was placed in a sling with an abduction pillow in neutral rotation for 6 weeks postoperatively. Passive ROM was started at 2 weeks followed by active-assisted ROM after 6 weeks. At 3 months, rotator cuff strengthening exercises (isometric followed by isokinetic) were initiated.
| . | Postoperative score at 5-year follow-up . |
|---|---|
| PROMIS Upper Extremity | 44.8 ± 2.8 |
| PROMIS Pain Interference | 38.7 ± 5.6 |
| PROMIS Pain Intensity | 30.7 ± 4.5 |
| American Shoulder and Elbow Surgeon Score | 98.33 |
| Subjective Shoulder Value | 90 |
| . | Postoperative score at 5-year follow-up . |
|---|---|
| PROMIS Upper Extremity | 44.8 ± 2.8 |
| PROMIS Pain Interference | 38.7 ± 5.6 |
| PROMIS Pain Intensity | 30.7 ± 4.5 |
| American Shoulder and Elbow Surgeon Score | 98.33 |
| Subjective Shoulder Value | 90 |
PROMIS, Patient-Reported Outcomes Measurement Information System.
| . | Postoperative score at 5-year follow-up . |
|---|---|
| PROMIS Upper Extremity | 44.8 ± 2.8 |
| PROMIS Pain Interference | 38.7 ± 5.6 |
| PROMIS Pain Intensity | 30.7 ± 4.5 |
| American Shoulder and Elbow Surgeon Score | 98.33 |
| Subjective Shoulder Value | 90 |
| . | Postoperative score at 5-year follow-up . |
|---|---|
| PROMIS Upper Extremity | 44.8 ± 2.8 |
| PROMIS Pain Interference | 38.7 ± 5.6 |
| PROMIS Pain Intensity | 30.7 ± 4.5 |
| American Shoulder and Elbow Surgeon Score | 98.33 |
| Subjective Shoulder Value | 90 |
PROMIS, Patient-Reported Outcomes Measurement Information System.
| . | Right arm . | Left arm . |
|---|---|---|
| Forward flexion | 160° | 160° |
| Extension | 65° | 65° |
| Abduction | 170° | 160° |
| ER (arm at side) | 30° | 55° |
| Internal rotation (arm at side) | T2 | T3 |
| . | Right arm . | Left arm . |
|---|---|---|
| Forward flexion | 160° | 160° |
| Extension | 65° | 65° |
| Abduction | 170° | 160° |
| ER (arm at side) | 30° | 55° |
| Internal rotation (arm at side) | T2 | T3 |
| . | Right arm . | Left arm . |
|---|---|---|
| Forward flexion | 160° | 160° |
| Extension | 65° | 65° |
| Abduction | 170° | 160° |
| ER (arm at side) | 30° | 55° |
| Internal rotation (arm at side) | T2 | T3 |
| . | Right arm . | Left arm . |
|---|---|---|
| Forward flexion | 160° | 160° |
| Extension | 65° | 65° |
| Abduction | 170° | 160° |
| ER (arm at side) | 30° | 55° |
| Internal rotation (arm at side) | T2 | T3 |
Outcome
The patient did well after surgery with considerable pain relief (9/10 to 1/10) by the 2-week time point. At the 6-month follow-up, she was pain free and recovered her preoperative ROM with 5-/5 strength in ER. At the latest 5-year follow-up visit, the patient reports no pain, 5-/5 strength in ER and no other limitations (Fig. 2B; Tables 1 and 2).
DISCUSSION
In respect to the etiology and surgical outcomes of isolated IS tears, there are several important points that make this case report unique and worthy of discussion. Though previous studies have reported on isolated MTJ lesions of the IS muscle, they are often described as a strain or partial tears with full-thickness tears only reported at the insertional footprint [1, 4–8]. As such, Walch et al. [1], Lunn et al. [6] and Taneja et al. [7] have evaluated the unique findings of IS tears at the MTJ. They reported a primarily atraumatic etiology and an association with calcific tendinitis; on magnetic resonance imaging (MRI), muscle edema is seen acutely with fatty infiltration progression during the chronic stages of injury [1, 6, 7]. The index patient in this report had an atraumatic onset with a full-thickness IS tear at the MTJ with symptom worsening in the immediate period after a steroid injection, which has not been reported previously.
Though nonoperative and primary surgical repairs have been described for isolated IS tears, there is no consensus on ideal treatment. Lunn et al. [6] reported no improvement with surgical repair in their series and recommended against surgical repairs. Walch et al. [1] reported surgical repairs of lateral repair (supraspinatus to teres minor), medialized repair of the stump or direct repair with outcomes non-superior to nonoperative treatment. Surgical treatment with graft augmentation has not been described for this condition as this is the first report of long-term pain relief and good functional outcomes following open repair of an IS MTJ tear with dermal allograft augmentation.
The other interesting aspect of this case report is related to the etiology of the RCT. Steroid injections have been associated with collagen degeneration, as well as tendon rupture in preclinical and clinical studies [9–14]. Interestingly, our patient noted an acute worsening of shoulder symptoms after steroid injection. Although we did not have an MRI prior to worsening of symptoms, we believe her tear was acute based on the presence of muscle edema. However, the etiologic association between MTJ tears and steroid injection cannot be established based on one case. Previous studies by Walch et al. [1] and Lunn et al. [6] have reported on a history of steroid injections prior to isolated IS lesion diagnosis, but these case series also report their treatment using steroids. The index patient also had a venous varix in the SG notch, which was considered in the etiology but aspiration of the varix did not relieve the patient’s pain. Carroll et al. [15] have reported on venous varix malformation in the SG notch as a cause of shoulder pain and IS muscle atrophy.
CONFLICT OF INTEREST STATEMENT
The authors of this paper certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interests in the subject matter or materials discussed in this manuscript.
FUNDING
This study was funded by NYU Langone Health. No external funding was received.
References
- magnetic resonance imaging
- edema
- ultrasonography
- adrenal corticosteroids
- arthroscopy
- glucocorticoids
- asthenia
- atrophy
- follow-up
- pain
- surgical procedures, operative
- varicosity
- mineralocorticoids
- shoulder region
- persistence
- rotator cuff injuries
- tendon repair
- shoulder injuries
- allografting
- rotator cuff repair
- infraspinatous muscle
- musculotendinous junction



