-
PDF
- Split View
-
Views
-
Cite
Cite
Tarik Souiki, Anas Belhaj, Abderrahim Ait Abderrhim, Badreeddine Alami, Layla Tahiri, Laila Chbani, Karim Ibn Majdoub, Imane Toughrai, Khalid Mazaz, Dermatofibrosarcoma protuberans of the anterior abdominal wall: case report and literature review, Journal of Surgical Case Reports, Volume 2022, Issue 6, June 2022, rjac272, https://doi.org/10.1093/jscr/rjac272
Close - Share Icon Share
Abstract
Dermatofibrosarcoma protuberans (DFSP) is a rare and slowly growing cutaneous tumor with high risk of local invasion and recurrence. Here, we report a case of a DFSP of the anterior abdominal wall diagnosed in a 45-year-old woman. The clinical examination showed an indurated well-limited oval mass localized in the supra-umbilical level and measuring 5 cm by 3 cm. The histological finding of skin biopsy was consistent with the diagnosis of DFSP. A wide local excision was performed while respecting minimum safety margins of 3 cm. The primary closure was possible after advancing the subcutaneous adjacent tissue. The histological examination of the surgical specimen confirmed the DFSP diagnosis and determined safe microscopic margins. After 4 years of regular follow-up, no locoregional or distant recurrence was observed. We discuss through this case the diagnosis difficulties and the particularities of the abdominal wall localization.
INTRODUCTION
Dermatofibrosarcoma protuberans (DFSP) is a rare and slowly evolving cutaneous tumor with a high local propensity of invasion and recurrence. Considering the indolent, and slow-growing characteristics, the diagnosis of DFSP is often delayed. The treatment consists of an aggressive surgical approach resulting in a large parietal defect that may be challenging to repair. We report the case of a young woman presenting with a DFSP of the anterior abdominal wall (AAW) managed by wide local excision (WLE) with primary closure. We discussed through this report the difficulties of the diagnosis, the particularities of the treatment approach in the abdominal localization, and the relevant literature.
CASE PRESENTATION
A 45-year-old woman complained of the occurrence of a small cutaneous lesion on the AAW evolving over the past precedent 3 years. The swelling volume had progressively increased. The physical examination revealed an oval mass with regular borders and a polylobed surface; the lesion was localized at the supra-umbilical level of AAW, and slightly lateralized on the right with dimensions of 5 cm by 3 cm (Fig. 1). The palpation revealed a hard and fixed swelling on the skin. However, it remains freely mobile regarding the deeply musculoaponeurotic plane. The histopathological findings on the skin biopsy were consistent with DFSP. The thoracic–abdominopelvic computed tomography (CT) scan did not show any metastatic lesions. The abdominal CT sections showed a well-defined enhancing soft tissue density lobulated lesion measuring 5.8 × 1.5 cm and arising from the AAW. The lesion presented a discreetly heterogeneous enhancement. It infiltrated subcutaneous tissue without any involvement of the musculoaponeurotic plane which remained distant from the lesion (Fig. 2). The patient underwent WLE with minimal macroscopic safety margins of 3 cm from the visible and palpable limits of the tumor (Fig. 3). The resulting defect was repaired with primary closure by advancing the adjacent tissue. Indeed, the cutaneous and subcutaneous tissue under the wound caudal edge was raised off anterior abdominal aponeurosis which facilitated flapping advancement and wound-free-tension coverage (Fig. 4a). We obtained an acceptable esthetic result in the form of a transverse mid-abdominal scar (Fig. 4b). The recovery was simple. The specimen histopathology revealed a characteristic of DFSP appearance with spindle cells in a storiform arrangement (Figs 5 and 6). The immunohistochemistry confirmed the diagnosis by revealing cluster differentiation 34 (CD 34) expression (Fig. 7). The margins are microscopically safe. The final decision of the multidisciplinary meeting consisted of surveillance. After 4 years of follow-up, no locoregional or distant recurrence was observed.

The clinical observation is showing the indurated plaque with multiple protuberant nodules, the limits of the resection are marked out with a 3 cm carcinologic margins (white arrow)
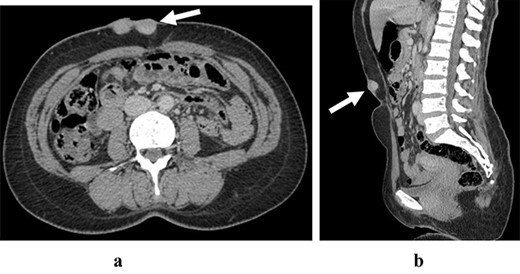
The abdominal CT scan in axial section (a) and sagittal section (b) are showing an heterogeneous enhanced lesion of the anterior abdominal wall respecting aponeurotic facia
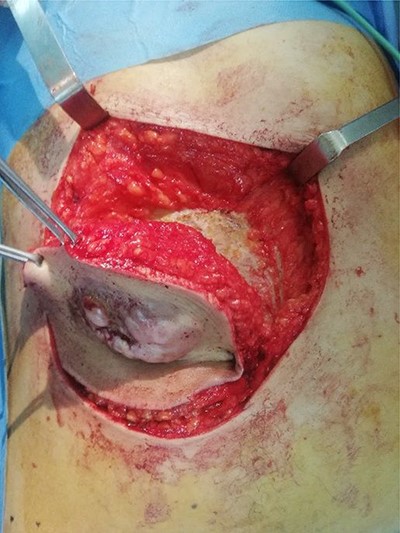

Per-operative view showing the resulting wound defect (a) repaired by primary closure (b)
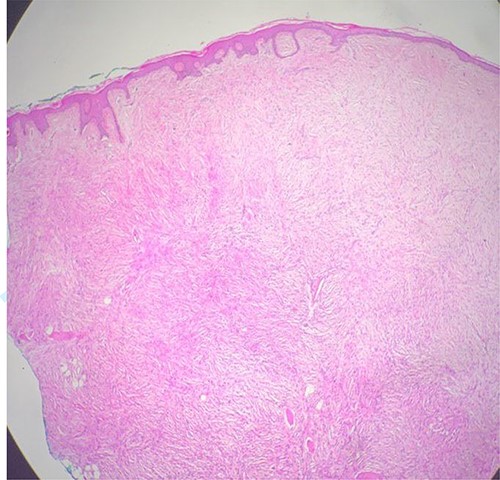
The histological findings are showing dermal proliferation of uniform spindle cells with a storiform pattern, it infiltrates subcutaneous adipose tissue (red circle) (hematoxylin–eosin staining; Original magnification ×40)
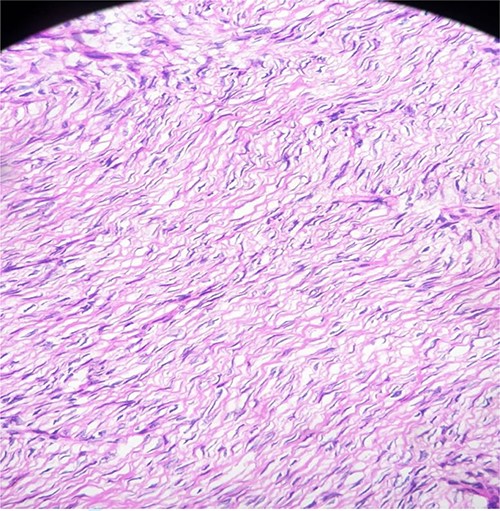
The histological findings showed storiform spindle cells proliferation with minimal atypia (hematoxylin–eosin staining; original magnification ×200)
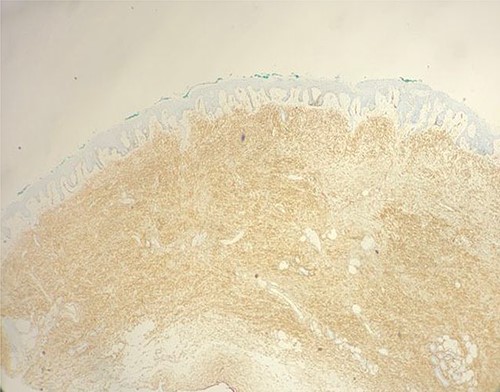
Immunohistochemistry study showing intense and diffuse elements that are positive for CD34 (original magnification ×100).
DISCUSSION
DFSP is a rare mesenchymal tumor arising in the dermis, it represents less than 2% of all soft tissue sarcomas [1]. DFSP occurs mostly in young adults between 20 and 50 years of age such was the case of our patient. [2]. It is commonly known that DFSP is mostly affecting the trunk and extremities [3]. The abdominal localization of DFSP remains among the rare malignant tumors of the soft tissues of the abdominal wall, which are dominated by the desmoid tumors [4].
DFSP most commonly presents as an asymptomatic indurated plaque that slowly enlarges over months to years. The tumors are covered by skin-colored, sclerodermiform or telangiectatic atrophic skin [5]. If untreated, it becomes upraised, firm and nodular. The nodule is often fixed to the dermis but can locally invade deeply into the fascia, the muscle and other underlying structures [6]. However, despite the delayed diagnosis, most tumors are generally superficial and <5 cm [7]. The diagnosis is suggested based on several arguments mainly including the evolving history of the lesion and its localization in the dermis. Indeed, indolent growth coupled with the rarity of DFSP and the variability in clinical appearance is contributing to the diagnostic delay [5]. Therefore, to minimize diagnosis delay and subsequent mismanagement, DFSP should be suggested in any long-standing, painless, asymptomatic parietal swelling. The final diagnosis is based on histological findings. Thus, DFSP is easily recognized by the proliferation of fibrohistocytic cells expressing CD34.
The tumor staging depends on the size and the tumor history. Indeed, in the case of small and superficial DFSP, the tumor extent and mobility, as well as a regional node can be easily assessed by physical examination [5]. Nevertheless, in routine clinical work, the imaging tools such as ultrasound and CT scan are often used and allowing to confirm the extension and provide objective lesion documentation for the surgical planning. CT reveals a solitary, subcutaneous lobular–nodular architecture and soft tissue attenuation and post-contrast agent enhancement. Besides, a CT scan is useful to evaluate distant metastatic patterns [6]. However, in the case of a large tumor or recurrent primary tumor, magnetic resonance imaging (MRI) is crucial in delineating the size and extent of the tumor, as well as its connection to adjacent neuromuscular and bone structures. [5].
Surgical resection is the main treatment for DFSP. It should take into account the potential infra-clinical extensions of the tumor, which might originate the local recurrence. The standard treatment consists of a WLE. The optimal width of the resection margin is controversial. However, the majority of authorities recommend margins of 2–4 cm [8, 9]. The management of defects resulting from tumor excision is a major concern, its’ reparation depends on the size and thickness of the resulting wound. Indeed, in the case of a small and superficial lesion accounting for the majority of DFSP in abdominal location [4], the lesions are often treated by WLE and primary closure without the required resect of the full abdominal wall thickness. In our patient, the primary closure was feasible for two main factors. First, the defect was partial thickness and spreading aponeurosis. Second, the laxity of the abdominal wall allows free-tension closure. However, in the case of a large tumor with deep invasion or recurrent tumor, a large full-thickness excision is recommended and reconstruction is required [4].
The post-treatment follow-up strategy has not well been established. The majority of local recurrences are evidenced within 3 years while 30% are developing after 5 years. Hence, it has been suggested that patients should be examined every 6 months for the first 3 years, then annually lifelong [10].
CONCLUSION
DFSP is a rare soft-tissue malignant tumor, characterized by a low risk of metastasis with a high potential for local invasion and recurrence. The clinical awareness of this entity is crucial allowing an early diagnosis and suitable management. Wide local excision (WLE) ensuring microscopically disease-free margins constitutes the treatment of choice. An adequate repair of the resulting defect of the anterior abdominal wall (AAW) should be highly considered in surgical management. Long-term follow-up is recommended to assess any potential risk of recurrence that might occur over many years.
AUTHORS’ CONTRIBUTIONS
All of the authors were involved in the preparation of this manuscript. T.S. was the surgeon and has made substantial contributions to the conception, bibliography and drafting of the manuscript. A.B. was the surgeon’s assistant and is involved in the drafting of the manuscript. B.A. provided and described radiological findings and is involved in the drafting of the manuscript. L.T. provided and described histological findings and is involved in the drafting of the manuscript. All co-authors read and approved the final manuscript. While further edits of the manuscript and comments were done by T.S.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest regarding the publication of this paper.
FUNDING
None.
CONSENT
Consent was obtained from the patient for publication of this case report and any accompanying images.



