-
PDF
- Split View
-
Views
-
Cite
Cite
Jordan Thomas, Adrian Khelif, Shrine Arulanantham, Jean Lemaitre, Jean-Emmanuel Lalive d’Epinay, Discovery of primary hyperparathyroidism following an endoscopic resection of the prostate: case report, Journal of Surgical Case Reports, Volume 2022, Issue 5, May 2022, rjac247, https://doi.org/10.1093/jscr/rjac247
Close - Share Icon Share
Abstract
Urological complaints related to primary hyperparathyroidism are frequently caused by the formation of urolithiasis. We report another rare clinical manifestation of primary hyperparathyroidism associated with urological symptoms. A 68-year-old man presented with dysuria related to benign prostatic hyperplasia. After undergoing endoscopic resection of the prostate, the patient’s urinary complaints persisted for several months thereafter. Urinary ultrasound revealed numerous calcifications on the prostatic resection area, requiring a cystoscopy for excision and analysis of the calcifications. This was followed by an endocrine evaluation that revealed a primary hyperparathyroidism due to a single parathyroid adenoma, which was responsible for the prostatic calcifications and the patient’s atypical symptomatology. The clinical evolution was favorable after parathyroidectomy. Symptomatic prostatic calcifications, due to primary hyperparathyroidism, on an area of the endoscopic prostate resection are uncommon. The only treatment is endocrine surgery.
INTRODUCTION
Transurethral resection of the prostate may be associated with unexpected postoperative complications. We report the case of primary hyperparathyroidism detected following persistent urinary complaints after a prostate surgery.
Primary hyperparathyroidism is a pathology in which symptoms are often nonspecific or absent. Urological complaints are generally renal colics caused by the presence of urinary tract stones. Our case presents an atypical symptomatology leading to the diagnosis of the endocrine pathology.
No other similar cases have been described in the literature.
CASE PRESENTATION
A 68-year-old patient, with a history of anticoagulated thromboembolic disease, presented with dysuria at a urology consultation in 2019. The primary assessment showed benign prostatic hypertrophy for which treatment with α-blockers was initiated. The treatment proved to be insufficient, and, therefore, the patient had to undergo a transurethral resection of the prostate in October 2019.
Immediate postoperative symptoms, usual in such cases, included urinary irritation and urgency. However, the complaints were abnormally persistent and were accompanied, 6 months later, by alguria associated with low macroscopic hematuria. Urinary tract infection was quickly ruled out.
Ultrasound evaluation of the urinary tract did not show any renal abnormalities, with the exception of numerous calcifications identified at the resection area of the prostatic urethra.
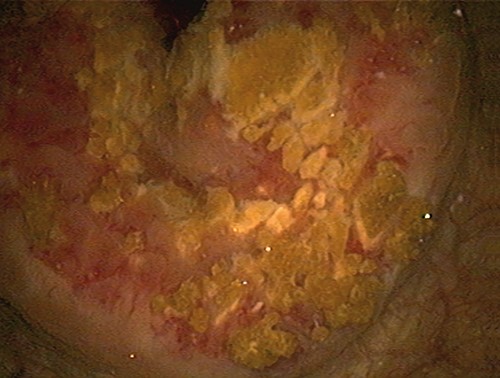
In May 2020, a cystoscopy confirmed the presence of multiple sharp yellowish crystals covering the prostatic resection area (Fig. 1). An endoscopic ablation was performed, without prostatic resection, to maintain anticoagulation treatment. The analysis of the calcifications revealed that they contained calcium phosphate and calcium oxalate. Following these results, a metabolic workup was carried out that demonstrated hypercalcemia at +2.91 mmol/L, increased parathyroid hormone at +128 ng/L and hypercalciuria at +15.55 mmol/24 h.
These biological results quickly raised the suspicion of primary hyperparathyroidism. Cervical ultrasound revealed a heterogeneous lesion behind the lower pole of the left thyroid lobe measuring 12x12x22 mm, suggesting the presence of a parathyroid adenoma.
In September 2020, the patient underwent scintigraphy with single-photon emission computed tomography, which revealed hyperfixation of the radiotracer in correlation with the lesion seen on the ultrasound (Fig. 2). He was diagnosed with primary hyperparathyroidism due to a parathyroid adenoma and underwent a lower left parathyroidectomy in December 2020. The anatomopathological results confirmed the excision of a single and benign adenoma.
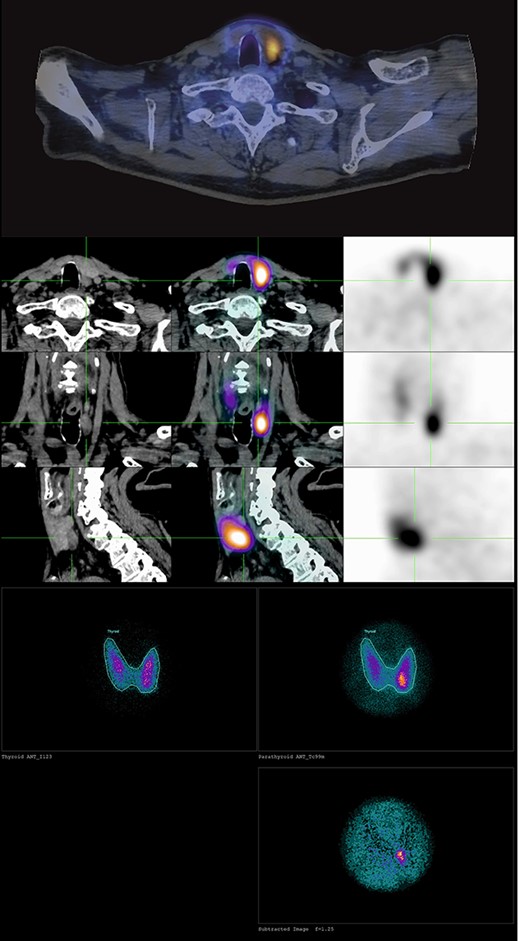
Scintigraphy with single-photon emission computed tomography images of the left inferior parathyroid adenoma.
The following month, the patient underwent another excision of urethral calcium deposits, which had reappeared during the check-up period, before the endocrine surgery. Biological controls illustrated the normalization of calcemia and parathyroid hormone (Table 1).
The postoperative course was uncomplicated with complete disappearance of symptoms. Clinical, biological and radiological postoperative assessments showed no recurrence after 1 year.
DISCUSSION
This atypical clinical case illustrates the need for multidisciplinary management when clinical and therapeutic results do not correspond to the usual postoperative outcomes.
In our case, the persistence of urological complaints, unusual 6 months after a standard transurethral resection of the prostate, required further investigation. The analysis of the calcifications and the metabolic workup, carried out in collaboration with endocrinologists, made it possible to quickly move toward a diagnosis of primary hyperparathyroidism with the discovery of a single secreting parathyroid adenoma. The large extent of the calcifications covering the resection surface, and their razor-blade appearance were the basis for the analysis and the diagnosis.
Primary hyperparathyroidism is a common endocrine pathology affecting 1% of the population, with a female predominance [1, 2]. The pathology is due to a singular and benign parathyroid adenoma in 80% of cases. It is rarely malignant. Diagnosis is based on abnormally high blood levels of calcium and parathyroid hormone. Excess parathyroid hormone leads to an increased release of bone calcium and intestinal calcium absorption. It also acts on the kidney by reducing urinary secretion of calcium. However, primary hyperparathyroidism predisposes to the formation of urolithiasis, due to the presence of abnormal calciuria [3, 4].
| . | Preoperative values . | Postoperative values . |
|---|---|---|
| Calcemia | 2.91 mmol/L | 2.33 mmol/L |
| PTH | 128 ng/L | 11 ng/L |
| Calciuria /24 h | 15.55 mmol/24 h | Unknown |
| . | Preoperative values . | Postoperative values . |
|---|---|---|
| Calcemia | 2.91 mmol/L | 2.33 mmol/L |
| PTH | 128 ng/L | 11 ng/L |
| Calciuria /24 h | 15.55 mmol/24 h | Unknown |
| . | Preoperative values . | Postoperative values . |
|---|---|---|
| Calcemia | 2.91 mmol/L | 2.33 mmol/L |
| PTH | 128 ng/L | 11 ng/L |
| Calciuria /24 h | 15.55 mmol/24 h | Unknown |
| . | Preoperative values . | Postoperative values . |
|---|---|---|
| Calcemia | 2.91 mmol/L | 2.33 mmol/L |
| PTH | 128 ng/L | 11 ng/L |
| Calciuria /24 h | 15.55 mmol/24 h | Unknown |
Generally asymptomatic, the symptomatology of primary hyperparathyroidism can vary according to the degree of hypercalcemia. Complaints are generally nonspecific and diverse: fatigue, muscle weakness, bone disease, nausea, vomiting or even renal colic due to the migration of urinary lithiasis present in 7–20% of patients with primary hyperparathyroidism [5]. In our case, the patient had no history of urolithiasis and presented with alguria and macrohematuria, very unspecific for an endocrine pathology. No other symptoms of hypercalcemia were present.
This unusual clinical case highlights the physiopathology of calcium deposits present at the surgical site. Tissue damage would lead to the increase of calcium exiting the damaged cell membranes responsible for the formation of localized calcifications on the prostatic resection area. Moreover, the acidic environment of the damaged tissue would support the process of saturation and crystallization [6]. The abnormally high renal excretion of calcium seemingly amplifies the phenomenon.
Curative treatment for primary hyperparathyroidism due to a parathyroid adenoma is based on the surgical excision of the adenoma [7–10]. According to Bilezikian et al. [1], there is no controversy about surgical treatment for symptomatic cases. The patient underwent removal of the parathyroid adenoma in December 2020, allowing for rapid normalization of calcemia and parathyroid hormone (Table 1). Various studies [11, 12] report a significant decrease in urinary calcium after parathyroid surgery. We did not repeat the urinary examination but noted that no new calcifications reappeared after the last excision, indicating a probable normalization of urinary calcium.
Atypical calcifications related to primary hyperparathyroidism, as a result of parathyroid adenoma, have been reported in other organs, including the lungs [13, 14]. Similar to our case report, parathyroid surgery was the therapeutic solution, allowing for the regression of calcium deposits. However, no similarity was found in the literature regarding prostatic calcifications on a resection area, making our case unique.
CONCLUSION
The appearance of symptomatic calcifications on a prostate resection area is a rare complication that may be related to primary hyperparathyroidism, with physiopathological mechanisms that are not yet fully understood. The only curative treatment is based on the surgical management of the endocrine pathology. This case report describes an unusual postoperative urological complication associated with an unprecedented symptomatology of primary hyperparathyroidism and reminds us of the importance of multidisciplinary care.
ACKNOWLEDGEMENT
The authors thank Audrey Lallemant for the translation and Céline Rasmont for iconographic improvement.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
FUNDING
No funding received.
The current address of the corresponding author is: Centre Hospitalier Universitaire Ambroise Paré, Bd John Fitzgerald Kennedy 2, 7000 Mons, Belgium. The work was carried out at Hôpital Du Jura Bernois, Les Fontenayes, 17, Saint-Imier 2610 Switzerland.



