-
PDF
- Split View
-
Views
-
Cite
Cite
Jai Chitnavis, Daniel Maghsoudi, Harshvir Grewal, Bilaterally symmetrical ganglion and subchondral cysts of the knee: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac064, https://doi.org/10.1093/jscr/rjac064
Close - Share Icon Share
Abstract
A 49-year-old patient, with a maternal history of arthritis, presented with an extra-capsular lump of the left knee. Following magnetic resonance imaging (MRI) scan and excision biopsy, the lump proved to be a benign ganglion cyst. The scan had also shown focal subchondral cyst formation and articular cartilage wear in the medial femoral condyle and patella, with no other abnormality. Four years later, she presented with identical symptoms and signs in the right knee. MRI scan confirmed a symmetrical pattern of ganglion and subchondral cyst location and size. Although both ganglion and subchondral cysts of the knee are common, their development is poorly understood and this combination of cyst formation and chondral wear has not been previously documented. Symmetry of end-stage knee osteoarthritis (OA) is recognized by clinicians. We speculate that OA of the knee begins asymptomatically with point-specific loss of articular cartilage, typically reflecting an inherent and bilateral vulnerability to degeneration.
INTRODUCTION
Most ‘cysts’ around the knee should be regarded as ‘sinuses’. Rather than being discrete and closed cavities, cysts around the knee are usually recesses directly communicating with the joint capsule or its cavity.
Cysts involving the knee joint may be classified as extra-osseous, with or without a synovial lining, or intra-osseous.
By cadaveric dissection, 19th century surgeons, including Baker (1877), noted that popliteal cysts were continuous with the knee joint [1].
The increasing use of magnetic resonance imaging (MRI) in modern clinical practice confirms that popliteal cysts are common and often asymptomatic [2]. Many such cysts are associated with degenerative meniscal tears and arthritis. Scans typically demonstrate popliteal cysts with a narrow but visible connection to the joint [3]. Histologically, most popliteal cysts are lined with synovium.
Typical ‘ganglion’ cysts of the knee are also extra-osseous in location. However, although opposed to the joint or its soft-tissues, ganglion cysts, unlike most popliteal cysts, are not synovial. Ganglion cysts contain mucoid gel, fluctuate in size and often spontaneously disappear. Without histological confirmation, it is difficult for MRI to distinguish between ganglion and synovial cysts and to decide whether the former are malignant.
Unlike extra-osseous cysts, subchondral ‘cysts’, are localized intra-osseous cavities. Commonly located just under regions of full thickness articular cartilage wear in osteoarthritis (OA), subchondral cysts also typically communicate with the joint [4].
Deformities of the knee, including varus and valgus malalignment, as well as disorders of the joint including arthritis, osteochondritis dissecans and degenerative meniscal tears commonly affect both knees in the same individual [5] (J Chitnavis, personal communication).
Despite the prevalence of extracapsular ganglion and subchondral cysts as isolated entities, their combined and bilateral presentation has not so far been described.
CASE REPORT
A 49-year-old female presented with a 6-week history of a painful lump on the medial aspect of her left knee. Growth of the lesion was associated with recreational running. The lump hurt at night. Her mother had undergone bilateral hip and unilateral knee replacement for OA.
Clinical examination revealed a firm 5 × 5-cm lump, located above the medial joint line and behind the medial collateral ligament (MCL). The left knee was otherwise normal. X-rays showed ‘mild medial and patella-femoral OA’. Due to concerns that the lump was malignant, a Gadolinium-enhanced MRI scan was performed and illustrated a septated ganglion cyst, measuring 45 × 29 × 17 mm, without solid components or malignant features. A 2-mm wide articular cartilage defect was evident in the medial femoral condyle, which was associated with adjacent subchondral cyst formation. Subchondral cyst formation was also present under the medial patella facet associated with articular degeneration.
Via a 6-cm medial incision, a multi-loculated mass was excised off the MCL and the semimembranosus tendon. Arthroscopy was not performed. Histology confirmed the lump was a benign ganglion. She made a good recovery and resumed recreational running.
Four years later, she presented with identical symptoms in her right knee. A 6 × 5-cm lump was present on the medial aspect of the joint. It was firm and trans-illuminated. The joint was otherwise normal.
A repeat MRI was performed and reported ‘very similar’ appearances to the left knee, showing a septated ganglion originating from the postero-medial aspect of the joint and subchondral cyst formation with a pattern and location mirroring that which had involved the left knee (Figs 1–3). Reassured by these findings, the patient deferred surgery.
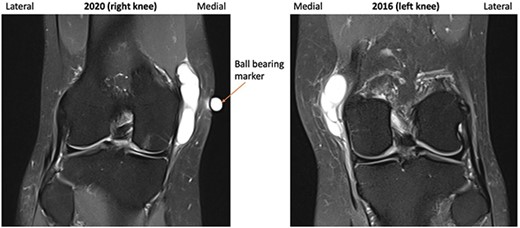
2016 and 2020 T2-weighted MRI in coronal plane with ganglion cyst visible medially.
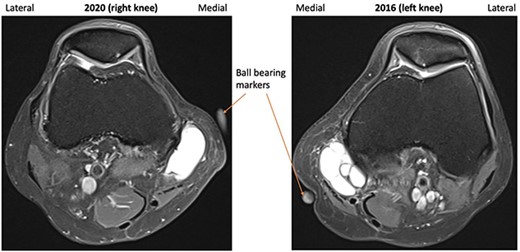
2016 and 2020 T2-weighted MRI in transverse plane with ganglion cyst visible medially.
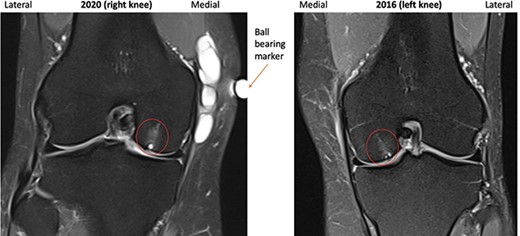
2016 and 2020 T2-weighted MRI in coronal plane with subchondral cyst circled medially.
Eighteen months later, she reported that the lump in the right knee had disappeared spontaneously and that she was still running without symptoms in either knee.
DISCUSSION
Bilateral ganglion and subchondral cyst presentation of the knees has not, to our knowledge, previously been described. The symmetrical presentation of cysts shown here is remarkable.
Repetitive micro-trauma, associated with activities such as running, is cited as a causative factor in the development of ganglion cysts [5].
Although the extra-osseous cysts in this report were related to the joint capsule, no meniscal tear or Baker’s Cyst was present in either knee to suggest, on MRI, that they were synovial.
Subchondral cyst formation associated with localized articular cartilage loss was evident in the weight-bearing portions of both medial femoral condyles and patellae, parts of the knee which are most commonly affected by articular cartilage loss in OA [6].
Population surveys using MRI have associated the presence of subchondral cysts of the knee with the progression of symptomatic OA and joint replacement [7].
More than 100 000 people undergo knee replacements annually in the UK, the vast majority for idiopathic OA [8].
A clinical study of patients with end-stage OA of the knee warranting knee replacement confirmed that 63% had bilateral disease, 97% of whom manifested a symmetrical pattern of OA on X-ray [9].
Our patient’s pain was associated with the presence of extracapsular ganglion cysts in both knees. The subchondral cysts in the weight-bearing regions of the tibio-femoral and patello-femoral joints were incidental MRI findings which did not contribute to pain nor swelling.
Until recently, the development of idiopathic OA in the appendicular skeleton was regarded as a random onset of ‘wear and tear’. Studies highlighting the prevalence of bilateral and symmetric patterns in idiopathic OA of the knee suggest otherwise [9].
The musculoskeletal system is the only system in the body which precisely exhibits ‘chirality’. The joint or part of the skeleton on one side of the body looks identical to but is a clearly distinguishable mirror image of that on the opposite side.
Point-specific breakdown of peri-capsular structures, articular cartilage and subchondral bone in identical sites in both knees, as exhibited by MRI in our case, support suspicions of an inherent susceptibility to symmetric tissue degeneration. While our patient does not clinically manifest symptomatic arthritis, full-thickness articular cartilage loss in both knees and a maternal history of knee OA suggest a future onset of symptomatic disease [10].
We believe this is the first reported example of bilaterally symmetrical ganglion and subchondral cyst formation of the knee. Findings provide insights into the patterns and development of idiopathic OA.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
LI G,
Solomon L, Warwick D, Nayagam S.
The NJR Editorial Board.



