-
PDF
- Split View
-
Views
-
Cite
Cite
Christine Li, Amanda Robertson, Umbilical epidermal inclusion cysts, an unusual cause of umbilical mass following laparoscopic surgery: case report, Journal of Surgical Case Reports, Volume 2022, Issue 3, March 2022, rjac059, https://doi.org/10.1093/jscr/rjac059
Close - Share Icon Share
Abstract
Umbilical lumps are a common presentation that can represent a diagnostic challenge as the differentials are broad. Epidermal inclusion cysts occur when epidermal cells are implanted in the dermis following trauma, or surgery. Although epidermal inclusion cysts are common, they are rarely cause of umbilical mass, with less than 10 cases described in the literature. Very few cases have been reported following abdominal surgery and none following laparoscopy. These lesions can occur with or without pain, mass, redness or spontaneous discharge and symptoms can persist for years. This paper reports a case of an umbilical epidermal inclusion cyst in a 52-year-old female presenting with a 6-week history of a painful, red umbilical lump on a background of two previous diagnostic laparoscopies. This was successfully treated with complete excision of the lesion.
INTRODUCTION
Epidermoid cysts are common benign cysts that arise from the infundibulum of a hair follicle and are encapsulated in a layer of epithelium [1]. Epidermal inclusion cysts refer specifically to when these occur as a result of the implantation of epidermal cells into the dermis following any kind of trauma, such as surgery. An epidermal inclusion cyst occurring in the umbilicus is a rare phenomenon, with very few cases previously reported and none following laparoscopy. Umbilical lumps can present diagnostic challenges as the differentials are broad, including umbilical hernia, embryologic remnant abnormalities, metastatic disease, endometriosis and suture granulomas. Epidermal inclusion cysts should also be included in this list.
We present an umbilical epidermal inclusion cyst in the context of previous laparoscopic surgery. This case report is compliant with the SCARE criteria [2].
CASE REPORT
A 52-year-old female presented to our emergency department (ED) with a 6-week history of an umbilical lump and 5 weeks of redness, swelling and pain. She had previously been seen in a general surgery clinic and was presumed to have an infected umbilical hernia. She was prescribed oral clindamycin and planned for an umbilical hernia repair once the infection had resolved. At the time of presentation to our ED, she had received 5 weeks of antibiotics with some improvement initially, but now worsening pain and haemopurulent discharge.
Her medical history consisted of endometriosis and hormone-responsive left breast cancer diagnosed 4 months prior on routine mammogram screening. This had been treated with a wide local excision, sentinel lymph node biopsy and adjuvant radiotherapy. At this point, she was awaiting a bilateral oophorectomy and hormone therapy. This had been delayed by her umbilical lump infection.
Her other surgical history included two laparoscopies performed 12 and 10 years prior for endometriosis. This had been complicated by keloid scarring in her umbilical incision site, although none was visible on presentation to us. She had no family history of medical illnesses, was a non-smoker and non-drinker. She had a body mass index of 30 kg/m2 and was allergic to penicillin, which would cause a rash.
On examination, her vital signs were within normal limits and she was afebrile. She had a 3 x 2 x 2 cm umbilical lump that was firm and tender with surrounding erythema and a small volume of haemoserous fluid discharge.
Blood tests revealed a normal white cell count of 8 x 109/L (reference range 4.0–12.0 x 109/L) and mildly elevated C-reactive protein of 8.7 mg/L (reference range < 5.0 mg/L). A computed-tomography (CT) scan revealed soft tissue thickening of the umbilicus of uncertain nature without intraperitoneal extension (Fig. 1).
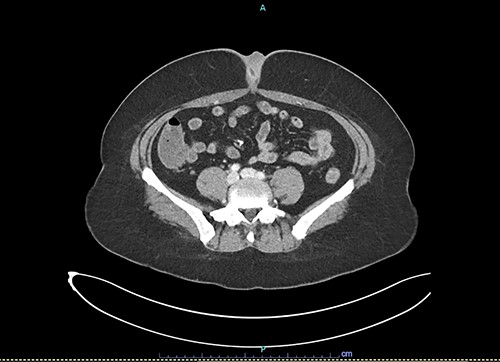
Axial slice of contrast-enhanced CT scan showing umbilical soft tissue thickening and fluid-filled structure at presentation to emergency department.
| Author . | Age . | Sex . | Previous surgery . | Duration of symptoms . | Pain . | Mass . | Redness . | Discharge . | Location . | Treatment . |
|---|---|---|---|---|---|---|---|---|---|---|
| McClenathan | 30 | M | N/A | N/A | Yes | No | Yes | N/A | Below fascia | Excision |
| 52 | F | N/A | Years | No | Yes | No | No | Above fascia | Excision | |
| 39 | F | N/A | 1 day | Yes | Yes | Yes | No | Above fascia | Excision | |
| 30 | F | N/A | Months | Yes | Yes | Yes | Yes | Below fascia | Excision | |
| 57 | F | N/A | Weeks | Yes | No | No | Yes | Above fascia | Antibiotics | |
| 51 | M | N/A | 2 weeks | Yes | No | Yes | No | Above fascia | Excision | |
| 9 | F | N/A | 1 year | No | Yes | No | No | Above fascia | Excision | |
| Andreadis | 39 | F | Abdominoplasty – 1 year prior | 6 months | No | Yes | No | No | Above fascia | Excision |
| Camenisch | 61 | F | Umbilical hernia repair + abdominoplasty – 7 years prior Laparotomy + wound revision – 6.5 years prior | 6 years | Yes | Yes | No | Yes | Above fascia | Excision |
| This case | 52 | F | Diagnostic laparoscopy x 2–10 and 12 years prior | 6 weeks | Yes | Yes | Yes | Yes | Above fascia | Excision |
| Author . | Age . | Sex . | Previous surgery . | Duration of symptoms . | Pain . | Mass . | Redness . | Discharge . | Location . | Treatment . |
|---|---|---|---|---|---|---|---|---|---|---|
| McClenathan | 30 | M | N/A | N/A | Yes | No | Yes | N/A | Below fascia | Excision |
| 52 | F | N/A | Years | No | Yes | No | No | Above fascia | Excision | |
| 39 | F | N/A | 1 day | Yes | Yes | Yes | No | Above fascia | Excision | |
| 30 | F | N/A | Months | Yes | Yes | Yes | Yes | Below fascia | Excision | |
| 57 | F | N/A | Weeks | Yes | No | No | Yes | Above fascia | Antibiotics | |
| 51 | M | N/A | 2 weeks | Yes | No | Yes | No | Above fascia | Excision | |
| 9 | F | N/A | 1 year | No | Yes | No | No | Above fascia | Excision | |
| Andreadis | 39 | F | Abdominoplasty – 1 year prior | 6 months | No | Yes | No | No | Above fascia | Excision |
| Camenisch | 61 | F | Umbilical hernia repair + abdominoplasty – 7 years prior Laparotomy + wound revision – 6.5 years prior | 6 years | Yes | Yes | No | Yes | Above fascia | Excision |
| This case | 52 | F | Diagnostic laparoscopy x 2–10 and 12 years prior | 6 weeks | Yes | Yes | Yes | Yes | Above fascia | Excision |
| Author . | Age . | Sex . | Previous surgery . | Duration of symptoms . | Pain . | Mass . | Redness . | Discharge . | Location . | Treatment . |
|---|---|---|---|---|---|---|---|---|---|---|
| McClenathan | 30 | M | N/A | N/A | Yes | No | Yes | N/A | Below fascia | Excision |
| 52 | F | N/A | Years | No | Yes | No | No | Above fascia | Excision | |
| 39 | F | N/A | 1 day | Yes | Yes | Yes | No | Above fascia | Excision | |
| 30 | F | N/A | Months | Yes | Yes | Yes | Yes | Below fascia | Excision | |
| 57 | F | N/A | Weeks | Yes | No | No | Yes | Above fascia | Antibiotics | |
| 51 | M | N/A | 2 weeks | Yes | No | Yes | No | Above fascia | Excision | |
| 9 | F | N/A | 1 year | No | Yes | No | No | Above fascia | Excision | |
| Andreadis | 39 | F | Abdominoplasty – 1 year prior | 6 months | No | Yes | No | No | Above fascia | Excision |
| Camenisch | 61 | F | Umbilical hernia repair + abdominoplasty – 7 years prior Laparotomy + wound revision – 6.5 years prior | 6 years | Yes | Yes | No | Yes | Above fascia | Excision |
| This case | 52 | F | Diagnostic laparoscopy x 2–10 and 12 years prior | 6 weeks | Yes | Yes | Yes | Yes | Above fascia | Excision |
| Author . | Age . | Sex . | Previous surgery . | Duration of symptoms . | Pain . | Mass . | Redness . | Discharge . | Location . | Treatment . |
|---|---|---|---|---|---|---|---|---|---|---|
| McClenathan | 30 | M | N/A | N/A | Yes | No | Yes | N/A | Below fascia | Excision |
| 52 | F | N/A | Years | No | Yes | No | No | Above fascia | Excision | |
| 39 | F | N/A | 1 day | Yes | Yes | Yes | No | Above fascia | Excision | |
| 30 | F | N/A | Months | Yes | Yes | Yes | Yes | Below fascia | Excision | |
| 57 | F | N/A | Weeks | Yes | No | No | Yes | Above fascia | Antibiotics | |
| 51 | M | N/A | 2 weeks | Yes | No | Yes | No | Above fascia | Excision | |
| 9 | F | N/A | 1 year | No | Yes | No | No | Above fascia | Excision | |
| Andreadis | 39 | F | Abdominoplasty – 1 year prior | 6 months | No | Yes | No | No | Above fascia | Excision |
| Camenisch | 61 | F | Umbilical hernia repair + abdominoplasty – 7 years prior Laparotomy + wound revision – 6.5 years prior | 6 years | Yes | Yes | No | Yes | Above fascia | Excision |
| This case | 52 | F | Diagnostic laparoscopy x 2–10 and 12 years prior | 6 weeks | Yes | Yes | Yes | Yes | Above fascia | Excision |
The patient was admitted and commenced on intravenous clindamycin. The following day an incision and drainage was performed on the ward under local anaesthetic and sterile conditions. Only minimal purulent fluid was expressed. At this point, our top differential diagnoses included endometriosis or fat necrosis within an umbilical hernia.
After 72 h of intravenous antibiotics with minimal improvement, a decision was made between the patient and surgical team to excise the lump. We performed an excision with the patient in a supine position under general anaesthetic. This revealed a 2 x 2 x 2 cm firm mass within the umbilical stalk. A small 1-cm fascial defect was found on excision of this lump and was repaired with loop polydioxanone (PDS) suture. The wound was closed with continuous monofilament absorbable sutures. The patient was discharged home 1 day post-operatively with oral clindamycin for a further 5 days. Histopathology revealed an umbilical epidermal inclusion cyst with mixed inflammation and abscess formation and surrounding fibrosis. There was no evidence of keloid and the cyst had been completely excised.
The patient’s post-operative course was complicated by a superficial wound infection and dehiscence, requiring surgical debridement 20 days following her initial surgery. Her wound was managed with dressings and healed by secondary intention. On follow-up, the patient was pleased to have had her umbilical lump excised as the pain had been burdensome and had delayed her breast cancer treatment.
DISCUSSION
Umbilical epidermal inclusion cysts are rarely described in the literature. In a retrospective study by Yan [3], epidermal inclusion cysts were a less common cause of umbilical mass than metastatic tumours. A review of seven patients by McClenathan [4] demonstrated that these lesions can occur with or without pain, palpable mass, redness or spontaneous discharge (Table 1). In two of these studies, the majority of the epidermal cyst extended below the abdominal fascia and communicated through a small fascial opening. As in our case, six were treated with complete surgical excision and none recurred.
Two cases of umbilical epidermal inclusion cyst have been reported by Andreadis [5] and Camenisch [6], both following abdominoplasties and presenting with an umbilical mass and intermittent pain and discharge. Table 1 presents a summary of the characteristics of umbilical epidermal inclusion cysts reported to date.
Several cases have been described of epidermal inclusion cysts arising from scars [7, 8]. In a case series of six patients, Lee et al. [7] proposed the mechanism behind this being due to itching of the scar leading to breakdown of the epidermis and implantation of epidermal elements into the dermis. There is little information in the literature, however, regarding the time to presentation of an epidermal inclusion cyst following scar formation. In our case, the patient presented 10 years after her diagnostic laparoscopy.
CONCLUSION
Despite the widespread use of laparoscopy across multiple surgical specialties, epidermal inclusion cysts following these surgeries have not been well-documented. They should be included in the differential diagnosis of patients presenting with a lump in a previous incision site and can be successfully treated with complete excision.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



