-
PDF
- Split View
-
Views
-
Cite
Cite
Wenlin Wang, Weiguang Long, Yang Liu, Bin Cai, Juan Luo, Surgical treatment of an overgrown asphyxiating thoracic dystrophy patient, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac530, https://doi.org/10.1093/jscr/rjac530
Close - Share Icon Share
Abstract
Asphyxiating thoracic dystrophy may affect the development of multiple organs of the body, so these kinds of patients are usually short and thin. We met a 16-year-old female patient whose development exceeded the normal level. Although she was only 16 years old, her height was 167 cm and her weight was 71 Kg. Such development is extremely rare for this kind of patient, and there is no similar report in the previous literature. Comparatively, her thorax was narrow and small, and the ratio of thorax to trunk was uncoordinated, which made her situation particularly serious. We adopted Wenlin procedure combined with Wang procedure for correction. Since these two procedures were ideal orthopaedic operations, and could correct the depression effectively, we finally achieved satisfactory results.
INTRODUCTION
Asphyxiating thoracic dystrophy (ATD) is an autosomal recessive disease first reported by Jeune in 1955 [1, 2]. The disease is extremely rare and fatal. Since most patients die in the first year of life, patients surviving to adolescence are more rarer [1]. ATD has serious impacts on physical development, and most patients are thin and short. However, we received a 16-year-old female ATD patient, whose physical development exceeded the normal level (Fig. 1A). Because her chest was narrow and small, her condition was serious, and operation was the only choice to save her life. We performed surgery for her and achieved satisfactory results.
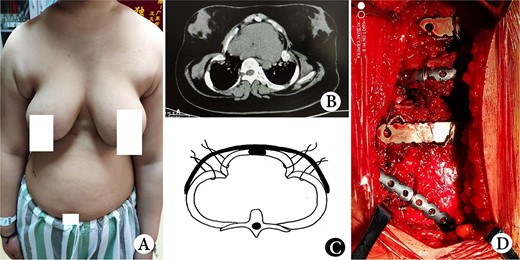
(A) Thorax appearance before operation; (B) CT scan image before operation; (C) schematic diagram of operation and (D) operation Picture.
CASE REPORT
The female patient had a full-term natural birth, and was the only child of an unrelated couple. She had dyspnea after birth and was treated with ventilation for one week. ATD was diagnosed at that time. Since then, she suffered from hypoxia for many times and gradually relieved after oxygen administration. Her condition improved after the age of five. Her activities were slightly limited, but physical development was not significantly different from that of children of the same age. At the age of 12, her body began to grow rapidly, and dyspnea gradually appeared. Her symptoms worsened a year before admission. Finally, at the age of 16, she was admitted to our hospital for surgery. Physical examination showed that her height was 167 cm, and weight 71 Kg; her thorax was narrow and small, and the ratio of thorax to trunk was uncoordinated (Fig. 1A). Computed tomography scan showed that the thorax was narrow, the lateral chest walls were sunken, and both lungs were compressed obviously (Fig. 1B). The operation was performed on both sides of the chest walls simultaneously. We used Wenlin procedure [3] and Wang procedure [4] to perform the operation. A longitudinal incision was made at the axillary midline to expose all ribs and costal cartilages. Two arc-shaped steel bars were inserted through the front of the sternum, with both sides of the bar located in front of the concave part of chest wall. The main concave parts were lifted and fixed on the steel bars with steel wires, and the other small concave parts were lifted and fixed on two additional short steel bars (Fig. 1C and D). After the concave parts were eliminated, the incisions were closed, and the operation was completed (Fig. 2A). Ventilator was used continuously for 1 week after operation. After the condition was stable, she weaned and changed to nasal catheter for oxygen. The oxygen saturation was maintained above 91%. Her chest circumference increased from 71 to 81 cm, and examination showed her thorax improved significantly after operation (Fig. 2B). She was discharged 25 days after operation, and recovered satisfactorily without symptoms. The bars were removed 2 years later, and there was no recurrence postoperatively.
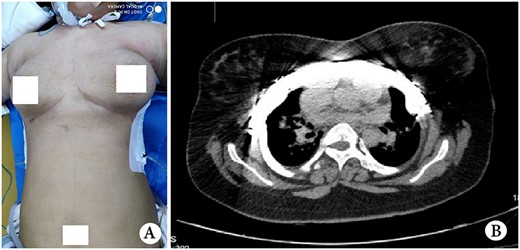
(A) Postoperative thorax appearance and (B) postoperative CT scan image.
DISCUSSION
Although lesions of ATD can exist in multiple parts of the body, the most dangerous lesions are located in the thorax [1–4]. Due to the narrow thorax and severe compression of the lungs, patients will have serious symptoms. Such lesions will not only affect respiratory function, but also the development of the whole body. Therefore, patients with ATD generally have two important characteristics: first, most patients die early; second, the surviving patients are generally thin and short.
By July 2022, 34 patients with ATD had received operations in our department. Of all these patients, this patient is the only one whose development is beyond the normal range. This case is particularly rare, and we have not found such a case in literature. The reason may be related to her eating habits. She is from northern China, and her diet is mainly meat food. Such eating habits may make her development beyond ordinary people. However, due to the lack of synchronous development of thorax, her symptoms are particularly serious.
Through the observation of our patients, we found that ATD could be roughly divided into two types [3–7]: Type I, the appearance of the thorax is cylindrical, and there are slight depressions on both sides of the chest wall; Type II, the appearance of the thorax is non-cylindrical, and there are obvious and deep depressions on both sides of the chest wall. According to the different types, the previous surgical methods of ATD can be divided into three categories, namely median thoracic expansion [2, 5–7], lateral thoracic expansion [8] and orthopaedic surgery [3, 4, 9, 10]. For Type I ATD, since there is no obvious lateral chest wall depression, only the median and lateral thoracic expansion can be used for the treatment. For Type II ATD, because the depression is obvious, only orthopaedic surgery is suitable.
Our patient is a typical Type II ATD patient. Due to overgrown of the body, her condition is very serious. In order to ensure the success of the operation, we adopted Wenlin procedure [3] combined with Wang procedure [4] for correction. Since these two procedures are very ideal orthopaedic operations, and both can correct the depression effectively, we finally achieved satisfactory results.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



