-
PDF
- Split View
-
Views
-
Cite
Cite
Emilio L Robles, Killian M Pache, Joshua S Gluck, Acute compartment syndrome of the leg caused by cocaine use, creatine supplementation and vigorous exercise, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac502, https://doi.org/10.1093/jscr/rjac502
Close - Share Icon Share
Abstract
Delayed diagnosis of acute compartment syndrome (ACS) can be catastrophic. Reporting abnormal presentations to facilitate timely diagnosis and treatment is vital. We present a case of ACS in the deep posterior compartment of the leg with an unusual presentation and cause. The patient presented to the emergency department complaining of numbness on the plantar aspect of his left foot, and described a history of cocaine use, increased exercise and creatine supplementation. The patient was diagnosed with acute deep posterior compartment syndrome of the left leg and underwent a lower extremity fasciotomy. There are case reports demonstrating that strenuous activity, drug use and creatine supplementation cause increased compartment pressures and ACS. Rare in the literature is a case where these activities occur concurrently with the abnormal presentation of symptoms seen in this case. We hope this case brings awareness of atraumatic risk factors and uncommon presentations to the medical community.
INTRODUCTION
Acute compartment syndrome (ACS) is an emergency where intra-compartmental pressures are elevated resulting in hypoxia, ischemia and soft tissue necrosis [1]. Complications range from neurovascular deficits, to limb loss and even death [2]. Rapidly diagnosing compartment syndrome is vital to prevent the morbidity that comes with delayed treatment. Pain out of proportion is the most common presenting symptom [3]. Abnormal presentations and causative factors pose diagnostic difficulty. Examples include strenuous exercise, rhabdomyolysis, drug use, surgical positioning, infection and more [4–6]. We present the case of a patient who presented with inability to feel sensation on the plantar aspect of the left foot. The patient had not sustained any trauma, but reported a vigorous exercise routine, regular cocaine use and the use of creatine as a workout supplement. The patient was diagnosed with deep posterior compartment syndrome of the leg and treated with fasciotomies. We believe the combination of cocaine use, creatine supplementation and vigorous exercise led to the development ACS. We believe this report to be crucial to the medical community’s ability to respond appropriately to abnormal presentations and rare causative factors.
CASE REPORT
We present the case of a 24-year-old Caucasian male with a chief complaint of numbness to the plantar aspect of his left foot for a day. The patient’s urine toxicology was positive for cocaine. Prior to this hospitalization, the patient was healthy without any past medical history. Socially, he admitted to occasional cocaine, tobacco and alcohol use. Orthopedics was consulted early morning the next day to evaluate the patient’s numbness. The patient reported the numbness was associated with mild pain in his calf with ambulation. The patient denied any trauma, however reports increasing his daily workout routine to include running five miles and playing basketball. Furthermore, he reports taking creatine supplements to enhance his performance. The patient admitted to using cocaine regularly, with a positive drug screen suggesting recent use.
The left lower extremity demonstrated 2+ dorsalis pedis and posterior tibial pulses, and intact gross motor movement from L5 to S1. He had complete loss of sensation to the plantar aspect of his foot, with intact sensation elsewhere. His lateral and anterior compartments were soft and compressible, however his posterior compartments were tense. He had mild discomfort to palpation and passive stretch of the posterior compartments. Radiographic imaging shown in Fig. 1 ruled out trauma.
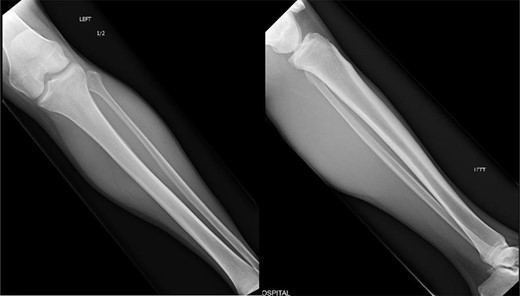
Orthogonal radiographic views of the patients left tibia and fibula. No evidence of trauma to be suspected which correlated with the patient’s history.
Although his symptoms were rather equivocal without any trauma, the combination of tense posterior compartments, insensate plantar foot and mild–moderate pain in the calf were concerning for atraumatic ACS. Given this, and the risk factors for development of compartment syndrome including recent cocaine use, vigorous exercise and creatine intake, it was elected to take the patient for urgent fasciotomy.
Intra-compartmental pressures were measured in the operating room and are demonstrated in Table 1. Criteria for deep posterior compartment syndrome of the left leg was clearly met, thus we proceeded with fasciotomies. Once within the deep posterior compartment, the flexor hallucis longus demonstrated evidence of hypoperfusion, yet still appeared viable with contractibility. The remaining muscles appeared well perfused. Intra-operatively the anterior and lateral compartments were noted to have increased tension when compared with the contralateral extremity. Given these findings, a fasciotomy of the lateral and anterior compartments was performed.
Preoperative compartment measurements and ΔP. The patient’s preoperative diastolic blood pressure was 69 mmHg
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 15 | 54 |
| Superficial posterior | 22 | 47 |
| Deep posterior | 67 | 2 |
| Lateral | 22 | 47 |
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 15 | 54 |
| Superficial posterior | 22 | 47 |
| Deep posterior | 67 | 2 |
| Lateral | 22 | 47 |
Preoperative compartment measurements and ΔP. The patient’s preoperative diastolic blood pressure was 69 mmHg
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 15 | 54 |
| Superficial posterior | 22 | 47 |
| Deep posterior | 67 | 2 |
| Lateral | 22 | 47 |
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 15 | 54 |
| Superficial posterior | 22 | 47 |
| Deep posterior | 67 | 2 |
| Lateral | 22 | 47 |
All of the compartments were noted to be softer and more compressible after fasciotomies. The compartment pressures were reassessed and demonstrated in Table 2. The compartment syndrome was resolved, particularly in the deep posterior compartment. The patient was noted to have 2+ pulses distally.
Post-operative compartment measurements and ΔP after wound closure. The patient’s preoperative diastolic blood pressure was 69 mmHg
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 19 | 50 |
| Superficial posterior | 17 | 52 |
| Deep posterior | 24 | 45 |
| Lateral | 29 | 40 |
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 19 | 50 |
| Superficial posterior | 17 | 52 |
| Deep posterior | 24 | 45 |
| Lateral | 29 | 40 |
Post-operative compartment measurements and ΔP after wound closure. The patient’s preoperative diastolic blood pressure was 69 mmHg
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 19 | 50 |
| Superficial posterior | 17 | 52 |
| Deep posterior | 24 | 45 |
| Lateral | 29 | 40 |
| Compartment . | Compartment pressure (mmHg) . | ΔP . |
|---|---|---|
| Anterior | 19 | 50 |
| Superficial posterior | 17 | 52 |
| Deep posterior | 24 | 45 |
| Lateral | 29 | 40 |
Post-operatively the patient remained without any gross motor or vascular deficits and the compartments remained soft and compressible. Most significantly by post-op day three the patient reported full resolution of the blunted sensation to the plantar aspect of his foot. The patient was discharged home after stabilization of his acute medical conditions. Unfortunately the patient never returned to clinic as instructed and was lost to follow up upon hospital discharge.
DISCUSSION
Corticosteroid is most commonly associated with a traumatic event, and the most common presenting symptom is pain out of proportion on examination [7]. Unusual causes include surgical positioning, thermal injuries, infections, rhabdomyolysis and iatrogenic causes [7–9]. Vasoconstrictive substances such as cocaine have been proposed as a cause of increasing compartment pressures, as have creatine supplementation and vigorous exercise [10–12].
As a potent vasoconstrictor cocaine decreases tissue perfusion, leading to skeletal tissue ischemia and direct myocyte toxicity [13]. The ischemia is proposed to cause a cascade beginning with cellular edema, which increases the compartment pressures, altering the venous–arterial gradient, causing more tissue ischemia and edema that continues the cycle of increased compartment pressures [1, 10]. This cascade will likely continue if there is a continued insult from ongoing cocaine use until the compartments are decompressed.
When creatine is transported from the blood into the skeletal muscle, it requires cotransport with sodium, which increases fluid transport into the muscle causing the fibers to swell [12]. In addition, creatine causes increased skeletal muscle synthesis [12]. Both factors contribute to an increase in tissue volume within the muscle compartments at rest and during exercise [12].
Muscle volume can increase ~20% during exercise, which causes an increase in interstitial compartment pressures [14]. This increased pressure impairs tissue perfusion, leading to skeletal muscle ischemia and increased cellular permeability causing fluid to shift into the interstitial space [14].
We believe the cumulative effects of cocaine use, creatine supplementation and a vigorous exercise routing led to acute deep posterior compartment syndrome. With the pathophysiology described above, it is reasonable to believe that each of these factors played a role in the manifestation of ACS. In addition, this patient had an unusual presentation in that his presenting symptom was plantar paresthesias. This correlates with the deep posterior compartment involvement. This case details two important aspects with the reporting of an unusual presentation and describing rare atraumatic causes. We hope this case helps to improve the clinical suspicion of atraumatic ACS to prevent delayed diagnosis and the negative consequences that will likely follow.
CONSENT
Written and verbal consent were obtained from the patient for publication of this case, clinical findings and related images. Written consent is available to the Editor-In-Chief upon request.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



