-
PDF
- Split View
-
Views
-
Cite
Cite
Zisis Ntontis, Nikolaos Trygonis, Panagiotis Bitados, Chrysostomos Tsatsoulas, Eirini Pappa, Kosmas Samartzidis, Ioannis Stavrakakis, Well leg compartment syndrome due to the lithotomy position in orthopedic surgery: a report of two cases and a review of the literature, Journal of Surgical Case Reports, Volume 2022, Issue 11, November 2022, rjac522, https://doi.org/10.1093/jscr/rjac522
Close - Share Icon Share
Abstract
The well leg compartment syndrome (WLCS) is a complication that can occur because of the lithotomy surgical position. Although it is a very rare entity, it can lead to a permanent disability if not properly treated. Very few cases have been described in the literature as a result of orthopedic surgery. We present two cases of WLCS that developed because of the lithotomy position. The first case concerns a patient who sustained a left floating knee and developed a compartment syndrome of the right uninjured calf during surgery. A good outcome has been achieved after early fasciotomies. The second case is about a patient who developed a compartment syndrome of the right buttock after a left unicompartmental knee replacement. This patient was treated conservatively because of delayed diagnosis. A brief literature review regarding the WLCS in orthopedic surgery is also conducted.
INTRODUCTION
Well leg compartment syndrome (WLCS) is defined as the occurrence of compartment syndrome in the uninjured limb in the absence of an underlying predisposing factor. It is highly associated with operations where the patient lies in the lithotomy or a hemilithomy position for a prolonged period of time. There have been patients reported in the literature, who developed this condition during procedures of general surgery, urology, gynecology and orthopedics [1]. WLCS is commonly misdiagnosed, as high clinical suspicion is required to identify the lesion. It usually begins under the effect of anesthesia leading to a delay of the diagnosis. Even though WLCS is underreported, it is assumed to affect one of every 3.500 operations performed in the lithotomy position [2]. Apart from the lithotomy position, there have also been described orthopedic patients who developed WLCS, resulting from the lateral decubitus position [3].
Prolonged surgical procedures in the lithotomy or the hemilithomy position along with perioperative hypoperfusion lead to ischaemia and increased capillary permeability, followed by a reperfusion injury once the leg is released from the compromising position. This whole mechanism leads to an increase in the intercompartmental pressure, presenting the pathophysiology and clinical symptoms of the typical compartment syndrome [4].
Risk factors associated with WLCS include the patient’s commorbidities, such as obesity and coagulopathy, surgical time exceeding 4 h, perioperative hypotension, compression of the well uninjured leg, as well as the use of intermittent air oppression equipment [5, 6].
Two cases of WLCS are presented in this paper. A review of the literature regarding this condition is also conducted.
CASE SERIES
Case 1
A 19-year-old male patient was admitted to the orthopedic department of our institution after a motorbike accident. The patient sustained a diaphyseal fracture of the left femur and ipsilateral tibia (floating knee) (Fig. 1), along with a right acromioclavicular joint type II injury and a right minimally displaced distal radius fracture. The patient was scheduled for emergent surgery. He underwent a retrograde intramedullary nailing of the left femur and an antegrade intramedullary nailing of the left tibia, under general anesthesia (Fig. 2). The operation was performed with the patient in the lithotomy position. The right intact leg was applied in 1000 of the hip flexion and 900 of the knee flexion. The duration of the surgery was 4 h and 20 min.

Ipsilateral femoral and tibial shaft fracture of the left limb (floating knee).

Post-operative view of the left femur and tibia. Concomitant retrograde IM nailing and antegrade IM nailing were performed.
As soon as the patient woke up from the general anesthesia, he reported severe pain of the right uninjured calf. After 3 h, the pain became worse and unresponsive to strong analgesic medications. On examination, extreme swelling in the right calf was noticed. The pain was exacerbated with passive movements of the right toes and ankle. A progressive weakness of the anterior tibialis and the extensor hallucis longus muscle was noticed as well. The diagnosis of the right uninjured tibia compartment syndrome owing to the lithotomy position was confirmed and the patient underwent the appropriate fasciotomies 6 h after the initial operation. The shoelace surgical technique (Fig. 3) was performed for gradual closure of the compartments. Six months post-operation, the patient has gained 5/5 motor strength of the anterior tibialis and 3/5 of the extensor hallucis longus muscle, with no sensory deficits. A left femoral and tibia nail dynamization has been performed because of the fracture delayed union.

Progressive closure of the right uninjured tibia open compartments using the shoelace technique.
Case 2
A 62-year-old patient underwent a left unicompartmental knee arthroplasty (UKA), because of a medial compartment degenerative arthritis. He reported a past medical history of type II diabetes mellitus and coronary artery disease. The operation was performed with the patient in the lithotomy position and lasted 1 h and 30 min. On the third post-operative day, the patient complained of a severe pain of his right buttock. On examination, the right buttock was found to be extremely swollen and tender on palpation. No neurovascular impairment was identified distal to the lesion. The intracompartmental pressure (IP) of the right buttock was measured 57 mmHg and the pressure difference (ΔP) between the diastolic blood pressure (DBP) and the IP was calculated 25 mmHg (ΔP = DBP − IP). The creatine phosphokinase (CPK) was 29 000. These results were compatible to a right buttock compartment syndrome.
Given the delay of the diagnosis, surgical fasciotomy was not obtained and a conservative treatment was selected. Rest, ice and intravenous (IV) fluids were applied to the patient. Significant subsidence of the pain and swelling occurred 15 days later. The 6-week post-operation follow-up did not reveal any functional deficit.
DISCUSSION
WLCS can easily be missed, because of unfamiliarity with this condition, especially by surgeons of specialties other than orthopedics. Diagnosis is based mainly on the clinical examination. The measurement of intercompartmental pressures is a useful tool in case there is doubt regarding diagnosis. However, one should keep in mind that intercompartmental pressure measurement has a 35% false positive rate [7], which can lead to unnecessary fasciotomies.
Most of the patients reported in the literature who developed WLCS sustained either a femoral shaft or a tibia fracture. The data that we extracted from the literature review showed that the median duration of surgery (mainly intramedullary nailing in the lithotomy position) was 280 min (4 h and 40 min) with a range of 300 min (minimum: 150 min, maximum: 450 min). Table 1 presents a review of the literature regarding orthopedic cases of WLCS, with the first case published by Dugdale et al. [8] in 1989.
| Study . | Fracture type-side . | Duration . | Operation . | Position . | Fasciotomy . | Outcome . |
|---|---|---|---|---|---|---|
| 1. Dugdale 1989 [8] | Comminuted femur fracture – L | 5 h 45 min | IM nailing | Supine. Right hip and knee flexion of 90°. Calf suspended in a broad well-padded sling | 2 incisions, 4 compartments | Five months postop: Moderate weakness in anterior compartment, mild contractures in deep post-compartment |
| Comminuted femur and femoral neck – L | 6 h | Locked IM nailing | Supine. Flexion abduction, external rotation of the hip Right calf in a well-padded stirrup splint | 2 incisions 4 compartments | Six months post-op: mild sensory and motor deficits in leg and foot, resolving | |
| 2. Anglen et al. 1994 [12] | Comminuted proximal femoral shaft fracture – R | 6 h | IM nailing, Distal screws breakage Exchange nailing. Injury of the femoral artery | Hip flexion and abduction Knee flexion Leg padded with towels on a holder | 2 incisions 4 compartments | Well-healed skin graft on lateral incision. Ankle stiffness. Normal sensation on the sole of the foot 2 years later |
| Femoral shaft Fracture Open tibia fracture Gustilo II | 6 h 15 min | Femoral nailing, Tibial debridement and external fixation | Hip flexion and abduction. Knee flexion. Leg held by a well-padded stirrup | 2 incisions 4 compartments | Four months later: well-healed skin grafts Complete loss of active ankle dorsiflexion, anesthesia on the dorsum of the foot Sticks and orthosis | |
| 3. Carlson et al. [13] | Femurs both | 3 h | Right, then left IM nailing | Left first. Hip flexion 90°, abduction 40°, external rotation 40° Knee flexion 90° Leg holder | Not specified | Recovery of 4/5 strength several months after |
| 4. Adler et al. [14] | Femoral shaft – L | 5 h 30 min | IM nailing, | Hemilithotomy position. Leg in a well-padded leg holder | 2 incisions 4 compartments | Unknown. 3 debridements before closure |
| Periprosthetic subtrochanteric hip fracture on a past femoral nailing – R | 4 h 30 min | Nail removal, ORIF with reconstruction nail | Hemilithotomy Leg on a well-padded leg holder | 2 incisions 4 compartments | Chronic burning pain in his left forefoot | |
| 5. Mathews et al. [15] | Open proximal femur fracture – R | 7 h 30 min | IM Nailing, Exchange nail with plate and Ilizarov | Hip flexion 80°, abduction 20°, knee flexion 70° | 2 incisions 4 compartments | Skin graft. Posterior compartment contractures (operated) 8 months post-op: Ankle stiffness Left foot diminished plantar sensation |
| Comminuted femoral shaft fracture Left sacroiliac dislocation – L | 6 h 4 h of leg rise | I.M nailing | Hip flexion 90°, abduction 30°, knee flexion 80° | 4 compartments. 12 hafter first fasciotomy: extension of anterior fasciotomy | 14 month later: Dorsiflexion and hallux extension 3/5, decreased sensation on the dorsum of the foot | |
| 6. Christodoulou et al. [16] | Gustilo II peritrochanteric and shaft femoral fracture – R | 5 h | IM nailing | Hemilithotomy position. | 2 incisions 4 compartments | Recovery of Hypoesthesia |
| Subtrochanteric femoral fracture Trimalleolar ankle fracture-L | 3 h | IM nailing. ORIFof the ankle fracture | Hemilithotomy position | 4 compartments | 1 year later: Partial loss of hallux dorsiflexion Foot and ankle edema | |
| 7. Meldrum et al. [17] | Comminuted Subtrochanteric fracture – R | 3 h 45 min | IM nailing | Leg in a padded stirrup | Not specified | 2 years later, shortening 2 cm, paraesthesia. Pain when standing for 3 h or more |
| 8. Weber et al. [18] | Comminuted subtrochanteric femoral fracture – L | 2 h 55 min | IM nailing | Hemilithotomy | Not specified | Loss of sensitivity in peroneal superficial nerve area, weakness in foot pronation |
| 9. Noordin et al. [19] | Femoral midshaft fracture – R | 4 h 15 min | IM nailing | Hip flexion 90°, 40° abduction, 40° external rotation Knee flexion 90° Leg in a well-padded calf res, ankle free Left leg height 45 cm from the heart level | 2 incisions 4 compartments | Full recovery in 24 h No mechanical or neurological sequelae 7 months after |
| 10. Meena et al. [20] | Subtrochanteric femoral fracture – R | 2 h 30 min | IM nailing, Then dynamic condylar screw within 48 h after trauma | Leg flexion 70°, abduction 40° Leg holder Blood pressure maintained low by anesthetists | 2 incisions 4 compartments | 1 year later: full recovery |
| 11. Clarke et al. [1] | Peritrochanteric fracture of the right femur with ipsilateral femoral and tibial shaft fractures | 6 h 30 min | Interlocking tibia nailing. Retrograde femoral nail | Hemilithotomy | 2 incisions 4 compartments | Complete recovery |
| 12. Anwer et al. [21] | Femoral Midshaft fracture – L | 2 h 30 min | ORIF. | Lithotomy | 2 incisions 4 compartments | Right foot motor function and sensation improvement |
| Study . | Fracture type-side . | Duration . | Operation . | Position . | Fasciotomy . | Outcome . |
|---|---|---|---|---|---|---|
| 1. Dugdale 1989 [8] | Comminuted femur fracture – L | 5 h 45 min | IM nailing | Supine. Right hip and knee flexion of 90°. Calf suspended in a broad well-padded sling | 2 incisions, 4 compartments | Five months postop: Moderate weakness in anterior compartment, mild contractures in deep post-compartment |
| Comminuted femur and femoral neck – L | 6 h | Locked IM nailing | Supine. Flexion abduction, external rotation of the hip Right calf in a well-padded stirrup splint | 2 incisions 4 compartments | Six months post-op: mild sensory and motor deficits in leg and foot, resolving | |
| 2. Anglen et al. 1994 [12] | Comminuted proximal femoral shaft fracture – R | 6 h | IM nailing, Distal screws breakage Exchange nailing. Injury of the femoral artery | Hip flexion and abduction Knee flexion Leg padded with towels on a holder | 2 incisions 4 compartments | Well-healed skin graft on lateral incision. Ankle stiffness. Normal sensation on the sole of the foot 2 years later |
| Femoral shaft Fracture Open tibia fracture Gustilo II | 6 h 15 min | Femoral nailing, Tibial debridement and external fixation | Hip flexion and abduction. Knee flexion. Leg held by a well-padded stirrup | 2 incisions 4 compartments | Four months later: well-healed skin grafts Complete loss of active ankle dorsiflexion, anesthesia on the dorsum of the foot Sticks and orthosis | |
| 3. Carlson et al. [13] | Femurs both | 3 h | Right, then left IM nailing | Left first. Hip flexion 90°, abduction 40°, external rotation 40° Knee flexion 90° Leg holder | Not specified | Recovery of 4/5 strength several months after |
| 4. Adler et al. [14] | Femoral shaft – L | 5 h 30 min | IM nailing, | Hemilithotomy position. Leg in a well-padded leg holder | 2 incisions 4 compartments | Unknown. 3 debridements before closure |
| Periprosthetic subtrochanteric hip fracture on a past femoral nailing – R | 4 h 30 min | Nail removal, ORIF with reconstruction nail | Hemilithotomy Leg on a well-padded leg holder | 2 incisions 4 compartments | Chronic burning pain in his left forefoot | |
| 5. Mathews et al. [15] | Open proximal femur fracture – R | 7 h 30 min | IM Nailing, Exchange nail with plate and Ilizarov | Hip flexion 80°, abduction 20°, knee flexion 70° | 2 incisions 4 compartments | Skin graft. Posterior compartment contractures (operated) 8 months post-op: Ankle stiffness Left foot diminished plantar sensation |
| Comminuted femoral shaft fracture Left sacroiliac dislocation – L | 6 h 4 h of leg rise | I.M nailing | Hip flexion 90°, abduction 30°, knee flexion 80° | 4 compartments. 12 hafter first fasciotomy: extension of anterior fasciotomy | 14 month later: Dorsiflexion and hallux extension 3/5, decreased sensation on the dorsum of the foot | |
| 6. Christodoulou et al. [16] | Gustilo II peritrochanteric and shaft femoral fracture – R | 5 h | IM nailing | Hemilithotomy position. | 2 incisions 4 compartments | Recovery of Hypoesthesia |
| Subtrochanteric femoral fracture Trimalleolar ankle fracture-L | 3 h | IM nailing. ORIFof the ankle fracture | Hemilithotomy position | 4 compartments | 1 year later: Partial loss of hallux dorsiflexion Foot and ankle edema | |
| 7. Meldrum et al. [17] | Comminuted Subtrochanteric fracture – R | 3 h 45 min | IM nailing | Leg in a padded stirrup | Not specified | 2 years later, shortening 2 cm, paraesthesia. Pain when standing for 3 h or more |
| 8. Weber et al. [18] | Comminuted subtrochanteric femoral fracture – L | 2 h 55 min | IM nailing | Hemilithotomy | Not specified | Loss of sensitivity in peroneal superficial nerve area, weakness in foot pronation |
| 9. Noordin et al. [19] | Femoral midshaft fracture – R | 4 h 15 min | IM nailing | Hip flexion 90°, 40° abduction, 40° external rotation Knee flexion 90° Leg in a well-padded calf res, ankle free Left leg height 45 cm from the heart level | 2 incisions 4 compartments | Full recovery in 24 h No mechanical or neurological sequelae 7 months after |
| 10. Meena et al. [20] | Subtrochanteric femoral fracture – R | 2 h 30 min | IM nailing, Then dynamic condylar screw within 48 h after trauma | Leg flexion 70°, abduction 40° Leg holder Blood pressure maintained low by anesthetists | 2 incisions 4 compartments | 1 year later: full recovery |
| 11. Clarke et al. [1] | Peritrochanteric fracture of the right femur with ipsilateral femoral and tibial shaft fractures | 6 h 30 min | Interlocking tibia nailing. Retrograde femoral nail | Hemilithotomy | 2 incisions 4 compartments | Complete recovery |
| 12. Anwer et al. [21] | Femoral Midshaft fracture – L | 2 h 30 min | ORIF. | Lithotomy | 2 incisions 4 compartments | Right foot motor function and sensation improvement |
Abbreviations. R: Right. L: Left. IM: Intramedullary. ORIF: Open reduction internal fixation.
| Study . | Fracture type-side . | Duration . | Operation . | Position . | Fasciotomy . | Outcome . |
|---|---|---|---|---|---|---|
| 1. Dugdale 1989 [8] | Comminuted femur fracture – L | 5 h 45 min | IM nailing | Supine. Right hip and knee flexion of 90°. Calf suspended in a broad well-padded sling | 2 incisions, 4 compartments | Five months postop: Moderate weakness in anterior compartment, mild contractures in deep post-compartment |
| Comminuted femur and femoral neck – L | 6 h | Locked IM nailing | Supine. Flexion abduction, external rotation of the hip Right calf in a well-padded stirrup splint | 2 incisions 4 compartments | Six months post-op: mild sensory and motor deficits in leg and foot, resolving | |
| 2. Anglen et al. 1994 [12] | Comminuted proximal femoral shaft fracture – R | 6 h | IM nailing, Distal screws breakage Exchange nailing. Injury of the femoral artery | Hip flexion and abduction Knee flexion Leg padded with towels on a holder | 2 incisions 4 compartments | Well-healed skin graft on lateral incision. Ankle stiffness. Normal sensation on the sole of the foot 2 years later |
| Femoral shaft Fracture Open tibia fracture Gustilo II | 6 h 15 min | Femoral nailing, Tibial debridement and external fixation | Hip flexion and abduction. Knee flexion. Leg held by a well-padded stirrup | 2 incisions 4 compartments | Four months later: well-healed skin grafts Complete loss of active ankle dorsiflexion, anesthesia on the dorsum of the foot Sticks and orthosis | |
| 3. Carlson et al. [13] | Femurs both | 3 h | Right, then left IM nailing | Left first. Hip flexion 90°, abduction 40°, external rotation 40° Knee flexion 90° Leg holder | Not specified | Recovery of 4/5 strength several months after |
| 4. Adler et al. [14] | Femoral shaft – L | 5 h 30 min | IM nailing, | Hemilithotomy position. Leg in a well-padded leg holder | 2 incisions 4 compartments | Unknown. 3 debridements before closure |
| Periprosthetic subtrochanteric hip fracture on a past femoral nailing – R | 4 h 30 min | Nail removal, ORIF with reconstruction nail | Hemilithotomy Leg on a well-padded leg holder | 2 incisions 4 compartments | Chronic burning pain in his left forefoot | |
| 5. Mathews et al. [15] | Open proximal femur fracture – R | 7 h 30 min | IM Nailing, Exchange nail with plate and Ilizarov | Hip flexion 80°, abduction 20°, knee flexion 70° | 2 incisions 4 compartments | Skin graft. Posterior compartment contractures (operated) 8 months post-op: Ankle stiffness Left foot diminished plantar sensation |
| Comminuted femoral shaft fracture Left sacroiliac dislocation – L | 6 h 4 h of leg rise | I.M nailing | Hip flexion 90°, abduction 30°, knee flexion 80° | 4 compartments. 12 hafter first fasciotomy: extension of anterior fasciotomy | 14 month later: Dorsiflexion and hallux extension 3/5, decreased sensation on the dorsum of the foot | |
| 6. Christodoulou et al. [16] | Gustilo II peritrochanteric and shaft femoral fracture – R | 5 h | IM nailing | Hemilithotomy position. | 2 incisions 4 compartments | Recovery of Hypoesthesia |
| Subtrochanteric femoral fracture Trimalleolar ankle fracture-L | 3 h | IM nailing. ORIFof the ankle fracture | Hemilithotomy position | 4 compartments | 1 year later: Partial loss of hallux dorsiflexion Foot and ankle edema | |
| 7. Meldrum et al. [17] | Comminuted Subtrochanteric fracture – R | 3 h 45 min | IM nailing | Leg in a padded stirrup | Not specified | 2 years later, shortening 2 cm, paraesthesia. Pain when standing for 3 h or more |
| 8. Weber et al. [18] | Comminuted subtrochanteric femoral fracture – L | 2 h 55 min | IM nailing | Hemilithotomy | Not specified | Loss of sensitivity in peroneal superficial nerve area, weakness in foot pronation |
| 9. Noordin et al. [19] | Femoral midshaft fracture – R | 4 h 15 min | IM nailing | Hip flexion 90°, 40° abduction, 40° external rotation Knee flexion 90° Leg in a well-padded calf res, ankle free Left leg height 45 cm from the heart level | 2 incisions 4 compartments | Full recovery in 24 h No mechanical or neurological sequelae 7 months after |
| 10. Meena et al. [20] | Subtrochanteric femoral fracture – R | 2 h 30 min | IM nailing, Then dynamic condylar screw within 48 h after trauma | Leg flexion 70°, abduction 40° Leg holder Blood pressure maintained low by anesthetists | 2 incisions 4 compartments | 1 year later: full recovery |
| 11. Clarke et al. [1] | Peritrochanteric fracture of the right femur with ipsilateral femoral and tibial shaft fractures | 6 h 30 min | Interlocking tibia nailing. Retrograde femoral nail | Hemilithotomy | 2 incisions 4 compartments | Complete recovery |
| 12. Anwer et al. [21] | Femoral Midshaft fracture – L | 2 h 30 min | ORIF. | Lithotomy | 2 incisions 4 compartments | Right foot motor function and sensation improvement |
| Study . | Fracture type-side . | Duration . | Operation . | Position . | Fasciotomy . | Outcome . |
|---|---|---|---|---|---|---|
| 1. Dugdale 1989 [8] | Comminuted femur fracture – L | 5 h 45 min | IM nailing | Supine. Right hip and knee flexion of 90°. Calf suspended in a broad well-padded sling | 2 incisions, 4 compartments | Five months postop: Moderate weakness in anterior compartment, mild contractures in deep post-compartment |
| Comminuted femur and femoral neck – L | 6 h | Locked IM nailing | Supine. Flexion abduction, external rotation of the hip Right calf in a well-padded stirrup splint | 2 incisions 4 compartments | Six months post-op: mild sensory and motor deficits in leg and foot, resolving | |
| 2. Anglen et al. 1994 [12] | Comminuted proximal femoral shaft fracture – R | 6 h | IM nailing, Distal screws breakage Exchange nailing. Injury of the femoral artery | Hip flexion and abduction Knee flexion Leg padded with towels on a holder | 2 incisions 4 compartments | Well-healed skin graft on lateral incision. Ankle stiffness. Normal sensation on the sole of the foot 2 years later |
| Femoral shaft Fracture Open tibia fracture Gustilo II | 6 h 15 min | Femoral nailing, Tibial debridement and external fixation | Hip flexion and abduction. Knee flexion. Leg held by a well-padded stirrup | 2 incisions 4 compartments | Four months later: well-healed skin grafts Complete loss of active ankle dorsiflexion, anesthesia on the dorsum of the foot Sticks and orthosis | |
| 3. Carlson et al. [13] | Femurs both | 3 h | Right, then left IM nailing | Left first. Hip flexion 90°, abduction 40°, external rotation 40° Knee flexion 90° Leg holder | Not specified | Recovery of 4/5 strength several months after |
| 4. Adler et al. [14] | Femoral shaft – L | 5 h 30 min | IM nailing, | Hemilithotomy position. Leg in a well-padded leg holder | 2 incisions 4 compartments | Unknown. 3 debridements before closure |
| Periprosthetic subtrochanteric hip fracture on a past femoral nailing – R | 4 h 30 min | Nail removal, ORIF with reconstruction nail | Hemilithotomy Leg on a well-padded leg holder | 2 incisions 4 compartments | Chronic burning pain in his left forefoot | |
| 5. Mathews et al. [15] | Open proximal femur fracture – R | 7 h 30 min | IM Nailing, Exchange nail with plate and Ilizarov | Hip flexion 80°, abduction 20°, knee flexion 70° | 2 incisions 4 compartments | Skin graft. Posterior compartment contractures (operated) 8 months post-op: Ankle stiffness Left foot diminished plantar sensation |
| Comminuted femoral shaft fracture Left sacroiliac dislocation – L | 6 h 4 h of leg rise | I.M nailing | Hip flexion 90°, abduction 30°, knee flexion 80° | 4 compartments. 12 hafter first fasciotomy: extension of anterior fasciotomy | 14 month later: Dorsiflexion and hallux extension 3/5, decreased sensation on the dorsum of the foot | |
| 6. Christodoulou et al. [16] | Gustilo II peritrochanteric and shaft femoral fracture – R | 5 h | IM nailing | Hemilithotomy position. | 2 incisions 4 compartments | Recovery of Hypoesthesia |
| Subtrochanteric femoral fracture Trimalleolar ankle fracture-L | 3 h | IM nailing. ORIFof the ankle fracture | Hemilithotomy position | 4 compartments | 1 year later: Partial loss of hallux dorsiflexion Foot and ankle edema | |
| 7. Meldrum et al. [17] | Comminuted Subtrochanteric fracture – R | 3 h 45 min | IM nailing | Leg in a padded stirrup | Not specified | 2 years later, shortening 2 cm, paraesthesia. Pain when standing for 3 h or more |
| 8. Weber et al. [18] | Comminuted subtrochanteric femoral fracture – L | 2 h 55 min | IM nailing | Hemilithotomy | Not specified | Loss of sensitivity in peroneal superficial nerve area, weakness in foot pronation |
| 9. Noordin et al. [19] | Femoral midshaft fracture – R | 4 h 15 min | IM nailing | Hip flexion 90°, 40° abduction, 40° external rotation Knee flexion 90° Leg in a well-padded calf res, ankle free Left leg height 45 cm from the heart level | 2 incisions 4 compartments | Full recovery in 24 h No mechanical or neurological sequelae 7 months after |
| 10. Meena et al. [20] | Subtrochanteric femoral fracture – R | 2 h 30 min | IM nailing, Then dynamic condylar screw within 48 h after trauma | Leg flexion 70°, abduction 40° Leg holder Blood pressure maintained low by anesthetists | 2 incisions 4 compartments | 1 year later: full recovery |
| 11. Clarke et al. [1] | Peritrochanteric fracture of the right femur with ipsilateral femoral and tibial shaft fractures | 6 h 30 min | Interlocking tibia nailing. Retrograde femoral nail | Hemilithotomy | 2 incisions 4 compartments | Complete recovery |
| 12. Anwer et al. [21] | Femoral Midshaft fracture – L | 2 h 30 min | ORIF. | Lithotomy | 2 incisions 4 compartments | Right foot motor function and sensation improvement |
Abbreviations. R: Right. L: Left. IM: Intramedullary. ORIF: Open reduction internal fixation.
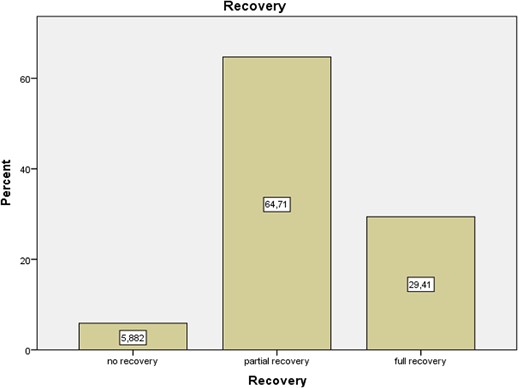
Upon suspicion, the patient should be transferred to the operating room, where either selected or extended fasciotomies should be performed. Upon early diagnosis and emergent reaction, the prognosis of WLCS is excellent with 95% of patients reporting no significant deficit [7,9]. On the other hand. Fitzgerald et al. [10] reported that 81% of patients undergoing fasciotomies develop long-term complications, but this should not deter surgeons from performing fasciotomies when deemed necessary. In the setting though of a delayed diagnosis, like our second case, surgical fasciotomy is no longer effective and might lead to serious complications, such as infection and limb amputation [11]. Our review suggests that the 29.4% of the patients who develop WLCS post-surgery achieved full recovery. 5.9 and 64.7% of the patients achieved no and partial recovery, respectively (Fig. 4).
Based on the existing literature, there are recommendations aiming at reducing the risk of post-operative WLCS as well as prompting early recognition of the syndrome. There are pre- and perioperative interventions that have shown to reduce the risk of WLCS [22]. These recommendations focus initially on the positioning of the patient by reducing the hemilithotomy position to a minimum or by changing to an open-leg position. Flexion of the hip and the knee should be limited in order to place the limb as close as possible to the level of the right atrium. Maintaining normovolaemia and avoiding vasoconstrictors further optimises the perioperative approach of the patient. The surgical team needs to maintain a high level of suspicion for patients who are at a risk of developing WLCS. This is further optimised with the use of general anesthesia versus epidural anesthesia, which allows an earlier recognition of the syndrome [23, 24].
To the best of our knowledge, there have been very few reports of WLCS in the literature, as a complication in orthopedic surgery. The UKA case may be the only one reported after a procedure that lasted < 2 h.
All the above information highlighta the need for better monitoring of the patients who are at risk of developing WLCS. According to McQueen et al. [25], continuous compartment monitoring may be the best option in confirming the diagnosis. However, compartment pressure measurements should never obviate a thorough physical exam and assessment of pain.
CONCLUSION
Our cases highlight that high index of suspicion for diagnosis of WLCS is required as a lack of awareness can lead to devastating complications. This condition remains widely unrecognized and increased awareness from the surgical team is required. A multidisciplinary approach from the surgeons as well as from the anesthetists is of paramount importance, in order to identify high-risk patients. Furthermore, all the available precautions to diminish the probability of developing WLCS during surgery should be taken.
AUTHORS CONTRIBUTION
1. Zisis Ntontis. Literature review, writing of introduction, discussion and conclusion.
2. Nikolaos Trygonis. Literature review, writing of Table 1 and abstract.
3. Panagiotis Bitados. Data processing using SPSS.
4. Chrysostomos Tsatsoulas. Figure formatting, writing of Figure 4.
5. Eirini Pappa. Figures’ editing and legends.
6. Kosmas Samartzidis. Literature review.
7. Ioannis Stavrakakis. Article review, writing of case series.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



