-
PDF
- Split View
-
Views
-
Cite
Cite
Daisuke Watabe, Tomofumi Nishino, Hajime Mishima, Masashi Yamazaki, Gluteal compartment syndrome after laparoscopic surgery in lateral jackknife position: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 10, October 2022, rjac477, https://doi.org/10.1093/jscr/rjac477
Close - Share Icon Share
Abstract
We present a case of a 42-year-old obese female with a body mass index of 38.4 kg/m2. Laparoscopic tumor resection of a left nonfunctioning adrenal tumor was performed in the lateral jackknife position, and the operative time was over 5 h. After awakening, she complained right buttock pain, and we suspected bursitis due to the surgical position and decided to follow up the patient. On the second postoperative day, spontaneous pain worsened, and the computed tomography scan of the hip showed significant swelling of the gluteal muscles, which led us to suspect a gluteal compartment syndrome. Intramuscular compartment pressure was measured under general anesthesia at 72 mmHg, and a fasciotomy was performed. The symptoms improved promptly after surgery and completely disappeared 2 months after surgery. Although the gluteal compartment syndrome is a rare condition in which circulation is impaired by compression of the gluteal muscles, treatment should be initiated promptly before serious complications arise.
INTRODUCTION
Gluteal compartment syndrome (GCS) is a very rare condition in which circulation is impaired by compression of the gluteal muscles, causing the gluteal muscles to swell and the intramuscular compartment pressure to rise. This causes further deterioration of circulatory disturbance, resulting in progressive melting and necrosis of muscle tissue, and is a very rare condition.
CASE PRESENTATION
A 42-year-old woman with a body mass index of 38.4 kg/m2 was consulted by an endocrine surgeon with a chief complaint of right buttock pain after awakening from anesthesia. The patient underwent laparoscopic tumor resection for a left nonfunctioning adrenal tumor under general anesthesia by endocrine surgeons. The patient was placed in the right lateral jackknife position (Fig. 1). The operative time was 5 h 37 min, and the anesthesia time was 8 h 15 min. After awakening, the patient complained of right buttock pain. A 12 cm long erythema centered on the right greater trochanter was observed. There was no paralysis, sensory disturbance and circulatory disturbance of the lower extremities. The patient was diagnosed with bursitis at the greater trochanter and was followed up for observation. Postoperative pain management was performed using transvenous self-regulated analgesia.

Lateral jackknife position. The right buttock is at the apex, supporting the patient’s weight. However, this is an intraoperative photograph of a patient different from the one shown here.
On X + 1, the day after surgery, the pain in the greater trochanter was less than that immediately after surgery, and the patient was able to hold on and walk. The patient’s resting pain was 78 mm on a visual analog scale (VAS), with an immediate postoperative pain of 100 mm. The pain on the extension of the buttock (hip adduction added to the straight leg rising position) was mild. Blood tests revealed markedly elevated creatine kinase (CK) of 67 871 IU/l. No myoglobinuria was observed. We suspected GCS; however, since the patient’s clinical symptoms improved, we decided to follow up by administering adequate hydration with supplemental fluids. At X + 2 days postoperatively, her pain at rest increased to 95 mm on the VAS, making it difficult for the patient to walk. Pain on the extension of the buttock also increased, but there was no evidence of nerve palsy and circulatory disturbance. CK levels1 in blood tests decreased to 26 357 IU/l. Computed tomography (CT) imaging showed a marked increase in gluteal muscle thickness in the axial view. The gluteus minimus was 26 mm and the gluteus medius was 35 mm, which was approximately three times thicker than that of the healthy side (Fig. 2). Based on the above, we made a diagnosis of GCS and decided to perform urgent fasciotomy. Under general anesthesia, the intramuscular compartment pressure was 72 mmHg on the affected side (healthy side, 26 mmHg; diastolic pressure, 50 mmHg). In the left lateral position, the patient was deployed using posterior approach. The fascia was incised with a shear knife, and the internal tension of the muscles was very high. The musculature of the medius and minimus fasciae was grossly dark red. The patient’s postoperative pain improved, and on X + 3 days, the pain on the buttock extension was relieved. A history of VAS and CK until the discharge is shown in Fig. 3. The symptoms disappeared 2 months after surgery.

Axial view of the maximum thickness of the left gluteus minimus and medius muscles on CT. The right side is about three times thicker than the left side with respect to the gluteus minimus (*) and the gluteus medius (#).
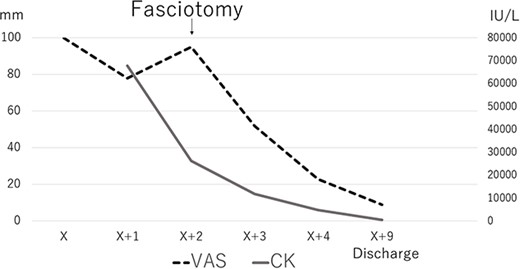
The course of VAS and CK. After fasciotomy, both are rapidly decreasing.
DISCUSSION
GCS is a rare condition first described by Owen et al. [1]. Early diagnosis and treatment are necessary because the disease progresses rapidly and misdiagnosis can result in serious sequelae, including death. Typical symptoms include pain in the buttocks, edema, tenderness, erythema and/or mottled bleeding. Eventually, the condition progresses to paresthesia and paralysis of the lower extremities. Pallors, pulselessness and loss of temperature are often late findings [2].
Recently, Adib et al. conducted a systematic review and meta-analysis of 139 cases, including those from their institution [3]. The most common etiology was postoperative, although the etiologies included heavy drinking, prolonged use of the same position owing to drug use, traumatic injury and medical etiology. The surgical position is another known risk factor for GCS. The lateral position was the most reported, followed by the supine and prone positions. In the lateral position, the dependent buttock region is subjected to greater direct pressure, which is a known risk factor [4, 5]. In this case, the patient was in a lateral jackknife position (Fig. 1), which places pressure on the buttocks and is considered a significant risk factor.
Obese patients not only have a greater degree of compression, but also a relatively longer perioperative immobility time, including increased anesthesia induction time and operative time when undergoing the same surgery [6, 7]. In our case, the patient required long time than 3 h for changing positions and setting up after anesthesia induction.
The diagnosis of GCS is made clinically based on the typical symptoms and other factors first described, but the diagnosis can be confirmed by measuring intracompartmental pressure [2]. Many authors use a threshold >30 mmHg as an indication for fasciotomy, but a diastolic pressure difference of <30 mmHg has been reported as a diagnostic criterion, in accordance with the muscle compartment syndrome more commonly seen in the lower legs [8]. When clinical suspicion is high, prompt treatment is recommended regardless of confirmatory pressure measurements [8–10]. The intramuscular compartment pressure was not measured in the awake state in this case, considering the long distance to the fascia. In our case, the preoperative pressure; 72 mm Hg, was >30 mmHg, and the difference from the diastolic pressure was <30 mmHg in our case. CK is also useful as a quantitative marker of muscle damage [11, 12]; however, the invasiveness of the surgery itself must also be considered.
The classic management of acute compartment syndrome is emergency fasciotomy. The goal of the surgery is to release the three anatomic gluteal compartments consisting of the gluteus maximus, gluteus medius, gluteus minimus and fascia lata [1, 11]. Although not surrounded by these compartments, the sciatic nerve is susceptible to compression owing to its proximity [1]. For patients with GCS, a neurological deficit at presentation is a clear indication of fasciotomy. In our case, fasciotomy was performed before the appearance of neurological abnormalities, and the patient consequently passed without neurological sequelae.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- obesity
- body mass index procedure
- edema
- computed tomography
- bursitis
- adrenal mass
- adrenal gland neoplasms
- anesthesia, general
- follow-up
- hip region
- hip joint
- intramuscular injections
- laparoscopy
- pain
- surgical procedures, operative
- fasciotomy
- laparoscopic surgery
- compartment syndrome, buttock
- awakening
- buttock pain
- compression
- tumor excision
- gluteal muscles



