-
PDF
- Split View
-
Views
-
Cite
Cite
Ralph Victor Yap, Manuel Villamor Jr, Scarless total thyroidectomy via transoral endoscopic vestibular approach: initial case series in a developing Asian country, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab623, https://doi.org/10.1093/jscr/rjab623
Close - Share Icon Share
Abstract
Conventional open thyroidectomy may leave a visible scar postoperatively and can lead to impaired quality of life. Since 2016, the transoral endoscopic thyroidectomy via vestibular approach (TOETVA) has gained popularity due to being a true ‘scarless’ procedure. However, minimally invasive thyroidectomy has not been widely adopted in the Philippines yet. From August 2019 to December 2019, nine patients (mean thyroid nodule size of 3.1 cm) underwent TOETVA with one open conversion due to adherent papillary cancer. Majority had a blood loss of <100 ml, whereas mean operative time was 149.8 ± 20.5 minutes. Five patients developed hypocalcemia (three transient), whereas two patients reported transient lower lip numbness. TOETVA is a safe and feasible novel procedure for both benign and malignant thyroid diseases. Care must be taken in selecting patients who opt for TOETVA, and that surgeons should reassess their limitations before implementing this technique in their surgical practice.
INTRODUCTION
Thyroidectomy, which was pioneered and advanced by Theodor Kocher has greatly evolved over the decades with further improved outcomes [1]. It remains a standard treatment for a variety of benign and malignant thyroid diseases. The conventional open thyroidectomy (COT) is performed via an anterior cervical neck incision that may leave a visible scar postoperatively. About 10% of patients who underwent COT are likely to pursue a revision of their scars at a later time. Regardless of scar type, the quality of life in these patients after surgery is impaired as well [2]. In an attempt to improve cosmesis/aesthetic outcomes by avoiding incisions on the cervical neck area, a variety of endoscopic techniques have been developed. Namely, these include endoscopic anterior/breast, axillary, postauricular and transoral approaches. These can be done in combination with the other techniques using conventional laparoscopic instruments or robotic systems.
The transoral approach has gained more popularity since the publication of the first 60 human cases that successfully underwent transoral endoscopic thyroidectomy via vestibular approach (TOETVA) by Anuwong in 2016 [3]. The procedure requires a 10-mm incision in the center of the oral vestibule and two stab incisions laterally to accommodate 5-mm trocars. It perfectly hides the mucosal wounds and heals without scarring. Multiple studies that followed have shown this approach to be safe, feasible, reproducible and can be an alternative to COT for benign and select malignant thyroid nodule(s) [4–6].
Minimally invasive and endoscopic thyroidectomies may have been performed in the Philippines, a developing country with a substantial incidence of benign and malignant thyroid diseases. However, local data are lacking as these techniques are currently not widely adopted among our local head and neck and general/laparoscopic surgeons. Thus, this study aims to share our initial single-institution case series of TOETVA in the Philippines in terms of safety and feasibility.
CASE SERIES
We retrospectively reviewed the medical charts of all patients who underwent TOETVA from 1 August 2019 to 31 December 2019, in our institution. The patients’ clinicopathologic data and postoperative outcomes were recorded. The institution’s research ethics committee approved this study (Protocol Code 2-2020-005). Written informed consent was provided by all patients.
Preoperatively, all patients underwent ultrasound of the cervical neck, serum thyroid hormone testing and fine-needle aspiration biopsy of the most dominant or suspicious nodule. All procedures were performed by a senior surgeon (M.V.) experienced in open thyroid and laparoscopic surgeries and who already completed 20 TOETVA procedures elsewhere. We adopted most of Anuwong’s indications and operative steps in performing TOETVA (Fig. 1) [4].
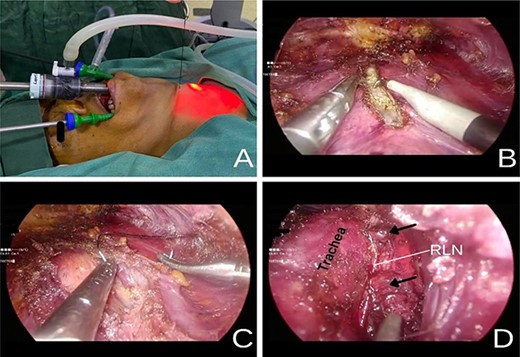
(A) Placement of a transcutaneous silk 2-0 holding suture on the midline to aid in initial dissection. (B) Division of the strap muscles along the median raphe using an L-hook cautery. (C) Retraction of the strap muscle cephalad and laterally with a transcutaneous silk 2-0 suture to expose the right thyroid lobe. (D) Right PGs (black arrow) and RLN identified after completely removing the thyroid gland.
A total of nine patients underwent TOETVA (eight females and one male) with a median age of 54 ± 12 years. The mean nodule size was 3.1 cm with almost 80% of the patients having a multinodular disease. All patients had total thyroidectomy via TOETVA with a mean operative time of 149.8 ± 20.5 minutes. The final biopsy showed benign colloid goiter in six patients and papillary thyroid cancer (PTC) in three patients. The sixth case was converted to open thyroidectomy due to adherence of tumor (PTC on final biopsy) to surrounding strap muscle. No other intraoperative complications/events were recorded. The majority of the patients had a blood loss of <100 ml and no patient required blood transfusion postoperatively. The mean visual analog scales (VAS) were 2.6 and 1.5 on postoperative days (POD) 1 and 2, respectively. Six patients received penicillin-based antibiotics while cephalosporin was given in three patients. Patients were discharged home after a mean of 3.1 days (range 1.8–8.9) (Table 1). After a mean follow-up of 10 months (range 8–12), five patients developed hypocalcemia (three transient and two permanent) and two patients reported transient lower lip numbness that resolved within 1 month. There was no wound hematoma, surgical site infection, wound dehiscence (Fig. 2A) or hoarseness (Table 2). One patient with a malignant biopsy underwent radioactive iodine therapy 2 months after surgery. The status of a patient’s cervical neck at 6 months postop is shown in Fig. 2B.
| Case # . | Age . | Sex . | ASA . | BMI . | Nodularity . | Largest nodule size (cm) . | IV Antibiotic used . | Operative time (mins) . | EBL (ml) . | Final Biopsy . | LOHS (days) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | 1 | 22.8 | Multinodular | 3.2 | Meropenem | 145 | 100 | Colloid Goiter | 2.8 |
| 2 | 69 | F | 2 | 28.7 | Uninodular | 3.6 | Ampicillin + Sulbactam | 135 | <100 | Colloid Goiter | 1.9 |
| 3 | 54 | F | 1 | 24.3 | Multinodular | 2.5 | Cefoxitin | 170 | <100 | Colloid Goiter | 3.9 |
| 4 | 45 | F | 2 | 26.9 | Multinodular | 4.2 | Cefuroxime | 157 | <100 | Colloid Goiter | 1.8 |
| 5 | 41 | F | 1 | 22 | Multinodular | 3.7 | Ampicillin + Sulbactam | 151 | <100 | Papillary Thyroid Carcinoma | 1.8 |
| 6 | 58 | M | 2 | 24.9 | Uninodular | 4.8 | Ampicillin + Sulbactam | Converted to Open | Papillary Thyroid Carcinoma | 3 | |
| 7 | 28 | F | 2 | 21.5 | Multinodular | 1 | Ampicillin + Sulbactam | 130 | < 100 | Papillary Thyroid Carcinoma | 2 |
| 8 | 57 | F | 2 | 26.9 | Multinodular | 2.6 | Ampicillin + Sulbactam | 185 | 150 | Colloid Goiter | 8.9 |
| 9 | 56 | F | 2 | 24.1 | Multinodular | 2.6 | Amoxicillin + Clavulanic | 125 | < 100 | Colloid Goiter | 1.9 |
| Case # . | Age . | Sex . | ASA . | BMI . | Nodularity . | Largest nodule size (cm) . | IV Antibiotic used . | Operative time (mins) . | EBL (ml) . | Final Biopsy . | LOHS (days) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | 1 | 22.8 | Multinodular | 3.2 | Meropenem | 145 | 100 | Colloid Goiter | 2.8 |
| 2 | 69 | F | 2 | 28.7 | Uninodular | 3.6 | Ampicillin + Sulbactam | 135 | <100 | Colloid Goiter | 1.9 |
| 3 | 54 | F | 1 | 24.3 | Multinodular | 2.5 | Cefoxitin | 170 | <100 | Colloid Goiter | 3.9 |
| 4 | 45 | F | 2 | 26.9 | Multinodular | 4.2 | Cefuroxime | 157 | <100 | Colloid Goiter | 1.8 |
| 5 | 41 | F | 1 | 22 | Multinodular | 3.7 | Ampicillin + Sulbactam | 151 | <100 | Papillary Thyroid Carcinoma | 1.8 |
| 6 | 58 | M | 2 | 24.9 | Uninodular | 4.8 | Ampicillin + Sulbactam | Converted to Open | Papillary Thyroid Carcinoma | 3 | |
| 7 | 28 | F | 2 | 21.5 | Multinodular | 1 | Ampicillin + Sulbactam | 130 | < 100 | Papillary Thyroid Carcinoma | 2 |
| 8 | 57 | F | 2 | 26.9 | Multinodular | 2.6 | Ampicillin + Sulbactam | 185 | 150 | Colloid Goiter | 8.9 |
| 9 | 56 | F | 2 | 24.1 | Multinodular | 2.6 | Amoxicillin + Clavulanic | 125 | < 100 | Colloid Goiter | 1.9 |
ASA, American Society of Anesthesiologists physical status classification; BMI, body mass index; EBL, estimated blood loss; IV, intravenous; LOHS, length of hospital stay (postoperative).
| Case # . | Age . | Sex . | ASA . | BMI . | Nodularity . | Largest nodule size (cm) . | IV Antibiotic used . | Operative time (mins) . | EBL (ml) . | Final Biopsy . | LOHS (days) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | 1 | 22.8 | Multinodular | 3.2 | Meropenem | 145 | 100 | Colloid Goiter | 2.8 |
| 2 | 69 | F | 2 | 28.7 | Uninodular | 3.6 | Ampicillin + Sulbactam | 135 | <100 | Colloid Goiter | 1.9 |
| 3 | 54 | F | 1 | 24.3 | Multinodular | 2.5 | Cefoxitin | 170 | <100 | Colloid Goiter | 3.9 |
| 4 | 45 | F | 2 | 26.9 | Multinodular | 4.2 | Cefuroxime | 157 | <100 | Colloid Goiter | 1.8 |
| 5 | 41 | F | 1 | 22 | Multinodular | 3.7 | Ampicillin + Sulbactam | 151 | <100 | Papillary Thyroid Carcinoma | 1.8 |
| 6 | 58 | M | 2 | 24.9 | Uninodular | 4.8 | Ampicillin + Sulbactam | Converted to Open | Papillary Thyroid Carcinoma | 3 | |
| 7 | 28 | F | 2 | 21.5 | Multinodular | 1 | Ampicillin + Sulbactam | 130 | < 100 | Papillary Thyroid Carcinoma | 2 |
| 8 | 57 | F | 2 | 26.9 | Multinodular | 2.6 | Ampicillin + Sulbactam | 185 | 150 | Colloid Goiter | 8.9 |
| 9 | 56 | F | 2 | 24.1 | Multinodular | 2.6 | Amoxicillin + Clavulanic | 125 | < 100 | Colloid Goiter | 1.9 |
| Case # . | Age . | Sex . | ASA . | BMI . | Nodularity . | Largest nodule size (cm) . | IV Antibiotic used . | Operative time (mins) . | EBL (ml) . | Final Biopsy . | LOHS (days) . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | F | 1 | 22.8 | Multinodular | 3.2 | Meropenem | 145 | 100 | Colloid Goiter | 2.8 |
| 2 | 69 | F | 2 | 28.7 | Uninodular | 3.6 | Ampicillin + Sulbactam | 135 | <100 | Colloid Goiter | 1.9 |
| 3 | 54 | F | 1 | 24.3 | Multinodular | 2.5 | Cefoxitin | 170 | <100 | Colloid Goiter | 3.9 |
| 4 | 45 | F | 2 | 26.9 | Multinodular | 4.2 | Cefuroxime | 157 | <100 | Colloid Goiter | 1.8 |
| 5 | 41 | F | 1 | 22 | Multinodular | 3.7 | Ampicillin + Sulbactam | 151 | <100 | Papillary Thyroid Carcinoma | 1.8 |
| 6 | 58 | M | 2 | 24.9 | Uninodular | 4.8 | Ampicillin + Sulbactam | Converted to Open | Papillary Thyroid Carcinoma | 3 | |
| 7 | 28 | F | 2 | 21.5 | Multinodular | 1 | Ampicillin + Sulbactam | 130 | < 100 | Papillary Thyroid Carcinoma | 2 |
| 8 | 57 | F | 2 | 26.9 | Multinodular | 2.6 | Ampicillin + Sulbactam | 185 | 150 | Colloid Goiter | 8.9 |
| 9 | 56 | F | 2 | 24.1 | Multinodular | 2.6 | Amoxicillin + Clavulanic | 125 | < 100 | Colloid Goiter | 1.9 |
ASA, American Society of Anesthesiologists physical status classification; BMI, body mass index; EBL, estimated blood loss; IV, intravenous; LOHS, length of hospital stay (postoperative).

Follow-up at 6 months from surgery showing the patient’s (A) oral vestibule and (B) anterior neck totally free from ascar.
| VAS, mean + SD | |
| POD 1 | 2.6 ± 1.8 |
| POD 2 | 1.5 ± 1 |
| POD 3 (n = 2) | 2 ± 1 |
| Complications | n = 8 |
| Tracheal perforation | 0 |
| Hematoma | 0 |
| Surgical site infection | 0 |
| Wound dehiscence | 0 |
| Hypocalcemia | |
| Transient | 3 |
| Permanent | 2 |
| Hoarseness/RLN injury | 0 |
| Lower lip numbness | |
| Transient | 2 |
| Permanent | 0 |
| VAS, mean + SD | |
| POD 1 | 2.6 ± 1.8 |
| POD 2 | 1.5 ± 1 |
| POD 3 (n = 2) | 2 ± 1 |
| Complications | n = 8 |
| Tracheal perforation | 0 |
| Hematoma | 0 |
| Surgical site infection | 0 |
| Wound dehiscence | 0 |
| Hypocalcemia | |
| Transient | 3 |
| Permanent | 2 |
| Hoarseness/RLN injury | 0 |
| Lower lip numbness | |
| Transient | 2 |
| Permanent | 0 |
SD, standard deviation.
| VAS, mean + SD | |
| POD 1 | 2.6 ± 1.8 |
| POD 2 | 1.5 ± 1 |
| POD 3 (n = 2) | 2 ± 1 |
| Complications | n = 8 |
| Tracheal perforation | 0 |
| Hematoma | 0 |
| Surgical site infection | 0 |
| Wound dehiscence | 0 |
| Hypocalcemia | |
| Transient | 3 |
| Permanent | 2 |
| Hoarseness/RLN injury | 0 |
| Lower lip numbness | |
| Transient | 2 |
| Permanent | 0 |
| VAS, mean + SD | |
| POD 1 | 2.6 ± 1.8 |
| POD 2 | 1.5 ± 1 |
| POD 3 (n = 2) | 2 ± 1 |
| Complications | n = 8 |
| Tracheal perforation | 0 |
| Hematoma | 0 |
| Surgical site infection | 0 |
| Wound dehiscence | 0 |
| Hypocalcemia | |
| Transient | 3 |
| Permanent | 2 |
| Hoarseness/RLN injury | 0 |
| Lower lip numbness | |
| Transient | 2 |
| Permanent | 0 |
SD, standard deviation.
DISCUSSION
In the Philippines, minimally invasive and endoscopic thyroid surgeries have already been performed but no local guidelines have been set up yet since the 2013 update on (local) clinical practice guidelines on thyroid nodules [7]. The American Thyroid Association stated that remote access thyroid surgery has a role in patients who fit strict selection criteria and that this approach requires to be performed by surgeons with a high level of expertise. However, their position statement was based on the most commonly utilized techniques in 2015 namely, endoscopic and robotic breast, axillary, bilateral axillo-breast and facelift approach [8].
The popularity of TOETVA started in 2016 after Anuwong successfully performed the first largest series of 60 patients. His inclusion criteria include (i) thyroid gland diameter of <10 cm, (ii) follicular neoplasm, (iii) Grave’s disease and (iv) papillary microcarcinoma without nodal metastasis [3]. Secondly, the ideal patient candidate is motivated to avoid a neck scar, has a benign nodule with a diameter of <4 cm, tumor/nodule located away from the recurrent laryngeal nerve (RLN) and pathologic thyroid lobe that is ipsilateral to the surgeon’s dominant hand. To safely implement such a technique in clinical practice, Razavi et al. [9] has recommended that the surgeon is well versed in procedures of the central neck, performs high-volume open thyroidectomies, familiar with laparoscopic/endoscopic instrumentation and is competent in neck/thyroid ultrasound.
We completed TOETVA in two out of three patients with PTC having a nodule size of 1 and 3.7 cm, respectively. A large single-center study has shown that TOETVA can be performed safely with central neck dissection in patients with PTC. There were no open conversions; however, the mean tumor size in their study was 0.7 ± 0.4 cm (largest 1.9 cm) [10]. Performance of a selective neck dissection to levels III and IV during TOETVA in patients with PTC has shown to be safe and feasible in a pilot study [11]. We believe that TOETVA may be safely done in patients with PTC of ≤4 cm in size but should be carefully screened and selected preoperatively. Additionally, the surgeon should have a low threshold for open conversion in case of tumor adherence. In a recent review article by Russel et al. [12], the rate of conversion to open surgery during TOETVA was 0.9% and the common reasons for such conversion were uncontrolled bleeding and unexpected tumorsize.
All patients in our study received total thyroidectomy via TOETVA with a mean operative time of 149.8 ± 20.5 minutes. The largest series comparing TOETVA and COT has shown that operative time was longer in the former group. Their mean operative time of bilateral thyroidectomy using TOETVA was 135.1 ± 37.6 minutes [3]. As the surgeon gains more experience with TOETVA, operative time is also expected to decrease given the short learning curve, ranging from 7 to 15 cases [12, 13].
The majority of our patients (75%) had a blood loss of <100 ml. In a comparative analysis, blood loss was lower in TOETVA compared with COT (38.25 ± 38.9 vs. 101.8 ± 126.6 ml) [14]. However, no significant difference in blood loss was found in a larger cohort of 216 patients [12]. It requires appropriate surgical skills, a meticulous technique and a careful selection of patients to achieve minimal bloodloss.
There were no occurrences of postoperative hematoma and seroma formation in our series. The rate of hematoma formation after TOETVA is low (0.1%) [12]. In a recent meta-analysis, no significant difference was observed between TOETVA and COT for such complications [15]. Likewise, the incidence of seroma formation after TOETVA in 425 patients is 4.7%. This phenomenon may be noted within POD 2–5 and can be managed with simple aspiration [3, 16]. In contrast to COT, the risk factors for seroma formation may be attributed to extensive flap creation, patient’s age, use of drain, operative duration, tumor size and surgeons’ operative volume. The use of no-drain in our series relied on the surgeon’s experience and comfort without its use in his experience with COT. Drain site on the skin can still yield scars in the postoperative setting. Albeit very small, this opposes the goal of having a totally ‘scarless’ procedure. Although still controversial, it is possible and safe to not put a drain in TOETVA but should be used with caution especially at the initial learning phase of the surgeon [17].
Compared with COT, TOETVA was found to have a significantly lower postoperative VAS, specifically on the neck, cervical back and swallowing, ranging from 0.8 to 2.3 in the first 48 hours [5, 18]. This benefit reflects the ‘minimally invasive’ nature of the technique. Interestingly, an oral vestibule incision is considered less painful compared with a Kocher incision. When compared with other techniques of thyroidectomy using the endoscopic or robotic approach, TOETVA requires less flap dissection leading to lower postoperative pain scores [5].
TOETVA is considered a ‘clean-contaminated’ case, thus requiring prophylactic antibiotics. The rate of wound infection in a review article is 0.1% and no significant difference was observed in a meta-analysis comparing TOETVA and COT [12, 15]. Varying antibiotic prophylaxis was used during the initial cases in our series but we have shifted to amoxicillin with clavulanic acid during the ninth and in the succeeding cases following the protocol of Anuwong et al. [3] where they reported no occurrence of surgical site infection out of 422 cases. Also, the use of preoperative oral mucosa antiseptic solution has to be emphasized aswell.
The most common complications following TOETVA are injuries to the parathyroid glands (PG) manifesting as hypoparathyroidism and/or hypocalcemia, RLN and mental nerves. Mental nerve injury, characterized as paresthesia on the lower lip has a rate of 2.29% after TOETVA [19]. To avoid such complications, we have adopted the revised technique to place the stab incisions and 5-mm working ports lateral to the canine teeth and on the lower lip [4]. Although no cases of permanent injury occurred in our series, previously reported cases were mainly transient, resolving within 4 months postoperatively [5].
In one study, the incidence of temporary and permanent RLN injury following TOETVA was reported at 4.7% and 0.7%, respectively [6]. As it remains a feared complication following COT, no significant difference was found in the incidence of both transient and permanent RLN palsy between COT and TOETVA [15]. Intraoperative neuromonitoring during TOETVA was shown to be safe and feasible in the identification and providing the functional status of the RLNs [20]. While it may reduce the risk of RLN injury following thyroidectomy, such an adjunct method is currently not available in our setting. Although no patient in our study developed postoperative hoarseness, we did not perform routine examination of the vocal cords under laryngoscopy.
The incidence of temporary hypoparathyroidism after TOETVA ranges from 10.9% to 14% [5, 21]. In a Korean population who underwent TOETVA, the reported incidence of permanent hypoparathyroidism was 1.3% [6]. Similar to COT, meticulous dissection is required to prevent iatrogenic injury to the PGs. Additionally, the surgeon should be attentive at all times to the position of the active blade of the ultrasonic device while usingit.
Other reported and unexpected complications in TOETVA that surgeons should be aware of include skin flap perforation and thermal lesions, subcutaneous emphysema, pneumomediastinum, pneumothorax, pneumoperitoneum, tracheal injury, suture dehiscence and carbon dioxide embolism [21, 22]. Lastly, we believe that patients who opt for a scarless thyroidectomy should be offered TOETVA. Multiple studies have shown that this approach has superior cosmetic outcomes and patient satisfaction and better quality of life compared with COT [23].
CONCLUSION
TOETVA is a safe and feasible novel procedure for both benign and malignant thyroid diseases. Given its similar outcomes other than the operative time with COT in published literature, care must be taken in selecting patients who opt for such procedure, and that surgeons should reassess their limitations before implementing this technique in their surgical practice especially in a resource-limited setting. As cases of TOETVA are increasingly being performed worldwide including in developing countries, we believe that this true ‘scarless’ procedure will soon become the standard approach if not over COT but among the endoscopic approaches.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
An educational grant through the Department of Surgery, Cebu Doctors’ University Hospital was provided by Johnson and Johnson (Parañaque City, Philippines), Inc.



