-
PDF
- Split View
-
Views
-
Cite
Cite
Mavra Masood, Tameem Jamal, Anthony Nye, Syed Shah, Sofia Shea, Surgical management of a local angioinvasive fungal soft tissue infection in the knee: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 1, January 2022, rjab546, https://doi.org/10.1093/jscr/rjab546
Close - Share Icon Share
Abstract
A 58-year-old male with an insignificant past medical history presented with chronic myelogenous leukemia in blast crisis. He began induction chemotherapy complicated by neutropenic fever. The patient then developed a nontender 1.5 cm violaceous firm indurated papule above the left patella with satellite lesions on his wrist and chest. A biopsy of the left patella showed obliterated blood vessels in the deep reticular dermis and numerous hyphae with septation and acute angle branching in the vessel wall consistent with angioinvasive aspergillosis. He was started on liposomal amphotericin and empiric voriconazole. Urgent local surgical excision of the primary lesion was recommended for source control. There is no clear recommendation on surgical intervention for angioinvasive aspergillosis, and further direction is needed. We present a case that illustrates surgical debridement for angioinvasive aspergillosis to be an effective method of source control along with systemic antifungal therapy.
INTRODUCTION
Angioinvasive fungal soft tissue infections are a rare but significant source of morbidity and mortality in immunocompromised individuals and require urgent intervention [1–4].
CASE REPORT
A 58-year-old male with a history of hypertension, hyperlipidemia, asthma, and newly diagnosed Hepatitis C presented with leukocytosis consistent with chronic myelogenous leukemia in blast crisis. He was given hydroxyurea and started on induction 7 + 3 idarubicin and cytarabine chemotherapy. The patient then developed neutropenic fever with multidrug-resistant Escherichia coli bacteremia and VRE enterococcus faecium. After 5 days of neutropenic fever, he developed a ‘knot’ on his left leg (Fig. 1). Physical exam revealed a nontender 1.5 cm violaceous firm indurated papule 2 cm above the left patella without evidence of cellulitis or infection. A total of 2 days later, the patient developed smaller satellite lesions on the left dorsal hand and chest. Dermatology was consulted and performed two 4 mm punch biopsies of the left patellar lesion for tissue staining and culture. Hematoxylin and eosin (H&E) staining revealed an obliterated blood vessel in the deep reticular dermis and numerous hyphae with septation and acute angle branching within the vessel wall consistent with angioinvasive fungus most consistent with angioinvasive aspergillosis (Figs 2 and 3). Biopsy of the wrist and further tissue cultures of the knee did not show any organisms but had reactive changes. Additionally, a chest computed tomography revealed new pulmonary nodules and atypical pneumonia with concern for disseminated disease. He was started on liposomal amphotericin and empiric voriconazole. At this time, urgent local excision of the knee was recommended for source control. A 4 × 5 cm lesion above the knee was excised with biopsy-proven clear margins and dressed with packing and a wound vaccum assisted closure (vac), as the lesion was proximal to a joint (Fig. 4). One month later, the patient received a split thickness skin graft. The patient tolerated surgical intervention well and had re-epithelialization of the donor site. He received three months of voriconazole for angioinvasive aspergillosis. One year later, there has been no recurrence or persistence of angioinvasive soft tissue or lung infection.

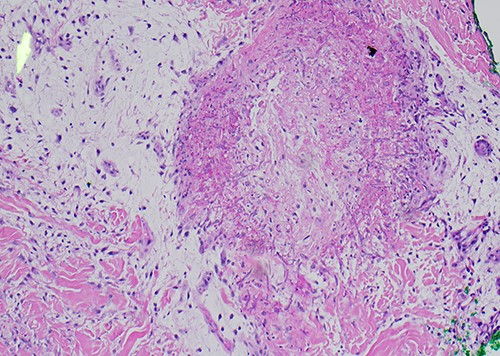
Original biopsy with numerous fungal hyphae demonstrating angioinvasion (H&E).
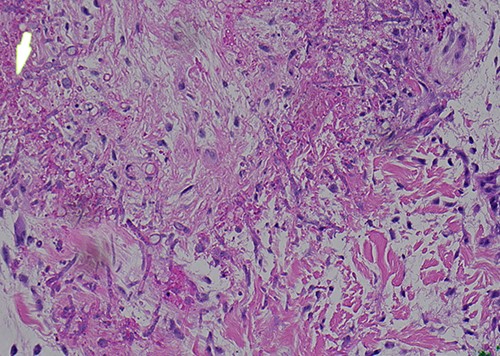
Higher magnification further demonstrating transmural invasion of fungal organisms (H&E).

DISCUSSION
Oncology patients undergoing severe neutropenia (defined as absolute neutrophil count <500/mL that lasts for >1 week) in the setting of lymphoma or leukemia high dose chemotherapy are at greatest risk of cutaneous fungal infection [1]. Opportunistic fungi such as Aspergillus, Mucor, Rhizopus and Fusarium are commonly implicated and infections can spread rapidly to deeper soft tissues and progress to fungemia. Angioinvasive fungal infections of soft tissue are a rare but significant source of morbidity and mortality due to obliteration of blood vessel walls, which leads to impaired wound healing of tissue and eventual necrosis. The mortality rate of disseminated Aspergillus is 75% [1]. Surgery is recognized as an important component of management in fungal sinusitis [1]. The debridement of necrotic and infected tissues enhances the chance of recovery and is recommended after patients undergo 1 week of appropriate antifungal therapy and have clearly demarcated borders of infection [1].
Aspergillus sp are usually inhaled as conidial spores and can cause disease most commonly in the lung in the form of allergic bronchopulmonary aspergillosis among others [2]. They are a slow sporulating and difficult to culture species [2]. Primary cutaneous aspergillosis is rare and usually is nosocomial in the setting of immunocompromise and damaged skin from adhesive tape dressings, venipuncture or catheter insertion sites, or burn scars [2]. Disseminated aspergillosis must be treated rapidly due to high fatality rate. Management includes removing immunosuppression and reversing neutropenia. First-line medical management includes voriconazole plus anidulafungin or caspofungin in patients with hematologic malignancy and severe neutropenia [3]. There are no clear guidelines on surgical management.
To our knowledge, this is the first report in the literature of surgical management in a case of angioinvasive aspergillosis in soft tissue. There is no clear recommendation on surgical intervention for angioinvasive aspergillosis, and further direction is needed [3].
Existing literature describes cutaneous aspergillosis in cancer patients with up to 85% of cases related to instrumentation [5]. Patients have received amphotericin B with or without surgical debridement. A review describes that around 50% who received treatment for cutaneous aspergillosis had no recurrence after therapy [5].
Through a multidisciplinary approach with hematology and oncology, dermatology, plastic surgery and infectious disease, it was felt that a request for surgical management was warranted at this time for a patient with evidence of disseminated disease and a potential source of primary infectious burden.
This case arose many questions on the risks and benefits of pursuing surgery. Namely, the surgery was over a joint and the true defect size was unknown and our patient’s severe immunocompromise made a relatively simple procedure much more complicated. Additional questions of margins, depth, and use of broad-spectrum antifungals needed to be answered. Our patient’s successful outcome can be attributed to maximized medical and/or surgical management. This case illustrates that surgical debridement for angioinvasive aspergillosis can be an effective method of source control along with systemic antifungal therapy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- amphotericin b
- biopsy
- aspergillosis
- leukemia, myelocytic, chronic
- debridement
- blast phase
- hyphae
- knee region
- knee joint
- liposomes
- patella
- soft tissue infections
- surgical procedures, operative
- wrist
- medical history
- chest
- voriconazole
- febrile neutropenia
- systemic antifungal treatment
- blood vessel wall
- papule
- excision
- chemotherapy, neoadjuvant
- reticular layer of dermis



