-
PDF
- Split View
-
Views
-
Cite
Cite
Amale Ghandour, Renzo Cecere, Treatment of device thrombus in the HeartWare HVAD: surgical exchange through thoracotomy, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab425, https://doi.org/10.1093/jscr/rjab425
Close - Share Icon Share
Abstract
Pump thrombosis can occur in patients with a left ventricular assist device (LVAD). It can be treated medically with thrombolytic agents or surgically. We present a case of a man who successfully underwent an LVAD swap via left anterior thoracotomy due to recurrent thromboses in the inflow cannula.
INTRODUCTION
Pump thrombosis is one of the possible adverse effects that can occur following the insertion of the HeartWare ventricular assisted device (HVAD), with a higher incidence rate in recent years [2]. It can be treated medically with thrombolytic agents or surgically [2]. Surgically, it has been described successful in the literature with the HeartWare HVAD [2]. Within Canada, to our knowledge, only one hospital has shared an experience about a pump thrombosis requiring a surgical intervention [3].
Thus, we will present a case of a patient that had multiple HVAD thromboses treated initially by thrombolysis, but then required ultimately a pump exchange.
CASE REPORT
A 56-year-old male, due to end stage ischemic cardiomyopathy, successfully underwent left ventricular assist device (LVAD) HeartWare implantation through median sternotomy. He was discharged on ASA 325 mg once a day combined with warfarin for an INR of 2.0–3.0.
The patient was readmitted 1 month later for subtherapeutic INR (1.57). On admission, LVAD parameters indicated increased power (5.0–6.2 W), as well as increased flows (8 L/min). The lactate dehydrogenase (LDH) was at 3237 U/L. A computed tomography (CT)-cardiac was performed to rule out any outflow graft obstruction. No evidence of thrombus was found. He was treated with systemic alteplase infusion consisting of a bolus of Alteplase 10 mg, followed by a bolus of 20 mg over 20 minutes, and an infusion of 1 mg/h over 24 hours. The target of INR was then increased to a range between 2.5 and 3.5.
The patient then presented to emergency multiple times for the same issue. It was decided to add clopidogrel 75 mg once a day to the medication regimen of aspirin and warfarin.
The patient was also seen by the Hematology team. They found that he was indeed responsive to ASA. The patient also was tested for factor V deficiency, lupus anticoagulant, prothrombin gene mutation and thrombophilia. All these tests were negative. Moreover, a CT chest and a CT urogram was done to rule out malignancy. No malignancy was found. Cystoscopy showed no tumor.
On 29 August 2020, the patient was admitted again for LVAD thrombosis. His INR was 2.54 and his LDH was at 1441 U/L. He received the protocol of thrombolysis. During this hospitalization, the patient experienced new onset diplopia. A CT-head confirmed a cerebral vascular accident in the region of his superior left cerebellar hemisphere. He was discharged in stable condition.
Three weeks later, the patient presented to the Emergency Department with chest pain accompanied by flows of 6.5 L/min at 6.0 W. His INR was 2.93. He was seen by the neurology team due to his recent stroke. The team established that there was a high risk of hemorrhagic transformation with alteplase. The cardiac surgery team decided that the HVAD exchange was the only possible solution.
The patient underwent an LVAD swap via left anterior thoracotomy on left femoro-femoral bypass. The retention screw on the inflow connector was released. The original device pump was disconnected from the apical connection ring. The outflow graft connection was freed from the outflow graft, clamped and divided. The pump was mobilized, and the driveline was severed. The remaining portion of the driveline was excised from its subcutaneous tunnel. A new HeartWare pump was brought into the field. The inflow connection was securely established, and then the outflow connection was made to the outflow graft with 4–0 prolene. The pump was carefully de-aired, and its operation initiated after passing the driveline through a fresh subcutaneous tract.
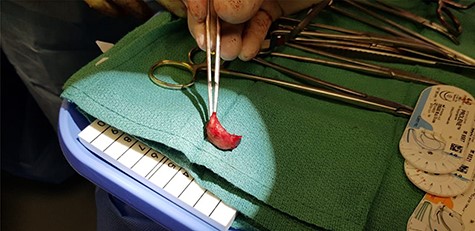
During the operation, there was a clot found around the inflow cannula (Fig. 1). The postoperative recovery was uneventful.
DISCUSSION
The patient presented in this case study underwent a minimal invasive approach to exchange his pump device. In the retrospective study conducted by the Toronto General Hospital, only one HeartWare was exchanged, and it was done through sternotomy [3].
The best moment to administer thrombolytic agents or to perform a surgical intervention to exchange the HeartWare due to a pump thrombosis should be individualized to each patient. There are risks associated with both intravenous thrombolytic therapies, as well as for surgical exchange. Throughout the literature, no score to identify the risk of mortality for a LVAD exchange has been found.
There is evidence showing that the surgical exchange has a higher success rate than medical therapy for pump thrombosis resolution, with lower mortality and lower recurrence [2]. To minimize the risk, the approach through left thoracotomy instead of resternotomy seems to be an effective surgical approach, avoiding right ventricular injury [1]. In our case, the patient remained in the intensive care unit 2 days and was discharged home on the 10th postoperative day.
CONCLUSION
This case study has demonstrated that the surgical intervention itself has been effective. The decision making to treat a device thrombosis should be made in accordance with patient characteristics and the device-related factors. Thoracotomy seems to be a safe approach, from one type of durable LVAD to another.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors report no funding sources.



