-
PDF
- Split View
-
Views
-
Cite
Cite
Ramzi Mejri, Kays Chaker, Bibi Mokhtar, Sami Ben Rhouma, Yassine Nouira, Inguinal bladder hernia: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab386, https://doi.org/10.1093/jscr/rjab386
Close - Share Icon Share
Abstract
Inguinal hernia is a common disorder that requires urgent and adequate surgical management. Multiple organs may be associated with inguinal hernias, but bladder involvement is rarely seen. The diagnosis is frequently done during surgery. It can be evoked before surgery when the patient presents with irritative and obstructive lower urinary tract symptoms. Retrograde urethrocystography or intravenous urography confirms the diagnosis. We report a case of inguinal hernia involving the bladder at the right side with a 72-year-old man. We performed a hernia repair after reintegration of the bladder.
INTRODUCTION
Nowadays, inguinal hernia is a frequent pathology. It requires prompt and appropriate surgical management. Inguinal hernias can be associated with several organs, but bladder involvement is uncommon, occurring in <4% of cases. Bladder hernia in inguinal hernia is rare and accounts for 0.5–3% of lower abdominal hernias [1]. It is often asymptomatic and the diagnosis is usually made intraoperatively during the surgical cure. Therefore, it is clear that the diagnostic approach and intraoperative strategy can be problematic for the surgeon. We report here an unusual case of an elderly man who presented with a massive right-sided inguinoscrotal hernia with complete bladder involvement.
CASE REPORT
A 72-year-old man with a history of controlled diabetes and hypertension presented to our department with right inguinal swelling and intermittent lower urinary tract symptoms (LUTS) with pollakiuria, dysuria, prolonged micturition time and a sensation of a full bladder after micturition. He reported nausea, vomiting and right lower quadrant paint. The patient also reported having to manually compress the scrotum in order to empty the bladder. Physical examination revealed a slightly painful on palpation and reducible 6 cm right inguinal hernia extending into the right hemiscrotum. The body mass index of the patient was 31.4 kg/m2. His PSA was 4.3 ng/ml. On uroflowmetry, maximum flow rate (Qmax) was 13 ml/s and the voided volume was 180 cc. The uroflow curve was flat. The Bacteriological examination of urine was negative. Retrograde urethrocystography revealed right inguinal hernia containing a portion of the urinary bladder (Figs 1,2). He also had an intravenous urography in order to study the upper urinary tract and to have an idea of the renal function. This radiological exploration confirms the data of the retrograde urethrocystography and illustrates well the bladder hernia. However, a moderate left hydronephrosis with a nonobstructive pyelic calculus of 1.5 cm was observed on intravenous urography (Figs 3,4). Intraoperative findings revealed a direct right inguinal hernia with complete herniation of bladder into the scrotum. The bladder appeared healthy with no signs of injury and was restored to its normal anatomical position without resection. The hernia was repaired with a biologic mesh by the Lichtenstein technique. The patient had an uneventful postoperative course. Concerning his pyelic calculus problem, shock wave lithotripsy sessions were scheduled.
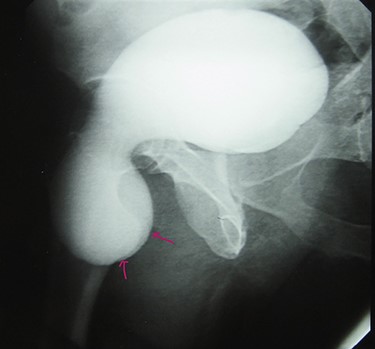
Retrograde urethrocystography: right inguinal hernia containing a portion of the urinary bladder.
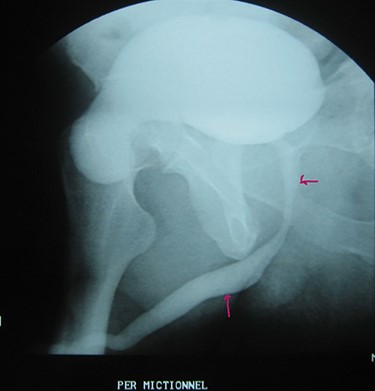
Urethrocystography: no obstruction under the bladder in the per mictional image.
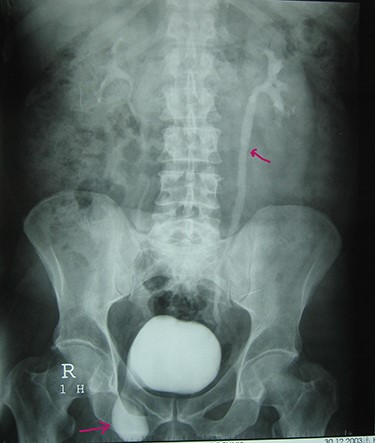
Intravenous urography: moderate left hydronephrosis and bladder addition image.

Intravenous urography: nonobstructive pyelic calculus of 1.5 cm.
DISCUSSION
Inguinal hernia of the bladder was first reported by Levine in 1951 as a scrotal cystocele [2]. The bladder is involved in <4% of all inguinal hernias. Most bladder hernias are direct, with a 70% male predominance, and most cases occur on the right side [3]. Inguinal bladder hernias occur mainly in the elderly and the associated risk factors are overweight, chronic urinary tract obstruction and weak pelvic muscles [4]. In our case, advanced age, male sex and obesity are the main risk factors used.
Pathologies associated with inguinal hernias of the bladder include benign prostatic hypertrophy, hydronephrosis with or without acute renal injury, vesico-ureteral reflux, urinary tract infections, bladder necrosis and scrotal abscesses [5]. However, it can be seen in infants, but usually disappears spontaneously with age. Most of the time, inguinoscrotal hernia is asymptomatic. It is often diagnosed intraoperatively during hernia repair surgery. Inguinoscrotal bladder hernia can be subdivided into the paraperitoneal, intraperitoneal and extraperitoneal type according to the relation with the parietal peritoneum [6]. In our case, the bladder was herniated directly without being covered by the peritoneum, which can be classified as the extraperitoneal type.
Patients with bladder hernias can present with LUTS. In cases of large inguinoscrotal bladder hernias, patients typically present with two-stage urination, involving spontaneous emptying of the bladder with a second step of manual compression of the hernia.
Radiological modalities include computed tomography, intravenous urogram and cystography. Ultrasound may be performed to detect the presence of hydronephrosis and to differentiate the bladder from other intrascrotal conditions [7]. A dog ear shaped bladder or a dumbbell shaped bladder may be a diagnosis on cystography. Computed tomography scan may be beneficial in obese men over the age of 50 with inguinal swelling and LUTS. This radiological investigation may be followed by cystoscopy to confirm the diagnosis and exclude other bladder pathology [8]. The presence of a bladder hernia does not modify the indications or the surgical strategy. The therapeutic procedure (open or laparoscopy) consists of fully reintegrating the bladder into the abdominal cavity and repairing the parietal defect. Currently, bladder resection is recommended only in cases with bladder wall necrosis, true herniated bladder diverticulum, a tight hernia neck or tumor in the herniated bladder [5]. Sometimes patients may opt for conservative treatment such as watchful waiting or intermittent catheterization [9]. Preoperative imaging is useful in planning the approach and anticipating difficulties.
CONLUSION
Inguinal bladder hernia is uncommon. It is often difficult to diagnose and remains a surgical challenge. It should be considered in obese men, over 50 years of age, with LUTS. Preoperative imaging is essential to prevent iatrogenic injury and complications. Cystography performed during intravenous or retrograde urography is a simple way to make the diagnosis. Treatment of this condition consists of returning the bladder to its anatomical position, repairing the inguinal hernia and treating subvesical obstruction if present.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest regarding the publication of this article.



