-
PDF
- Split View
-
Views
-
Cite
Cite
Chiharu Tanaka, Hidekazu Furuya, Masaomi Yamaguchi, Kazuo Kanabuchi, Kenji Kuwaki, Reconstruction for rupture of profunda femoris artery aneurysm in a patient with sarcopenia, Journal of Surgical Case Reports, Volume 2021, Issue 9, September 2021, rjab384, https://doi.org/10.1093/jscr/rjab384
Close - Share Icon Share
Abstract
Profunda femoris artery aneurysm (PFAA) is rare and has a high incidence of rupture. Herein, we report the case of an 80-year-old man who developed sarcopenia after gastric surgery. The patient presented to our hospital with a reddish thigh and was diagnosed with PFAA rupture. We performed aneurysmectomy and graft interposition in emergency. Postoperative enhanced computed tomography revealed an interposed graft, and the patient was discharged on postoperative Day 7. We considered that the PFAA patients with sarcopenia has a high risk of rupture because the muscles surrounding the profunda femoris artery became weak, and should be followed-up closely.
INTRODUCTION
True profunda femoris artery aneurysm (PFAA) is extremely rare and generally affects men over 70 years. Herein, we report a case of PFAA rupture in a patient with sarcopenia who underwent surgical reconstruction.
CASE REPORT
An 80-year-old man, who was followed up for peripheral arterial ischemic disease and iliac aneurysm for 2 years, presented with edema and ecchymoma on the left anterior surface of the thigh for 4 days. A history of distal gastrectomy for gastric cancer 2 years ago and low cardiac function without coronary disease was noted. The patient was previously a smoker, and had received cilostazol. An endovascular procedure was planned for the right ischemic limb after postoperative recovery from gastric surgery. The right common femoral artery (CFA) and superficial femoral artery (SFA) were occluded with an ankle-brachial index value of 0.3. The right common iliac artery had an aneurysmal change of 34 mm in diameter. The measurement of psoas muscle mass index at the third lumber vertebrae level was 4.62 cm2/m2.
The patient looked pale but was conscious. He was thin and weighed 40 kg (body mass index, 14.5) due to loss of appetite after gastric surgery; however, his left thigh was reddish, edematous and painful (Fig. 1). Hemodynamics, such as blood pressure and heart rate, were stable. Blood tests revealed a hemoglobin level of 3.41 mmol/l. Ultrasonography showed a 72 × 52 mm PFAA with a thick thrombus and hematoma extending into the adductors (Fig. 2). A venous thrombus was also observed in the left femoral vein. Enhanced computed tomography (CT) revealed a ruptured left PFAA 64 × 54 mm in diameter (Fig. 3A and C). In addition, right iliac artery aneurysm and right CFA and SFA occlusion were also observed.
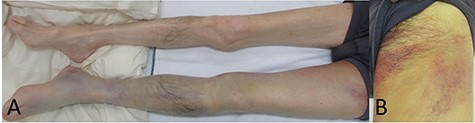
(A) Picture of the lower extremities of the patient. His left limb was edematous and hemostatic. (B) Picture of the left thigh. The patient’s thigh appeared reddish and had pain.
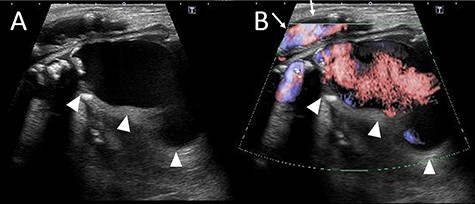
(A) The ultrasound image. The deltas point the PFAA. (B) Color Doppler imaging using ultrasonography. The deltas indicate the PFAA, and the arrows indicate the blood flow of the SFA.
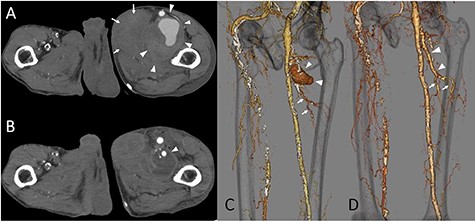
(A) The CT scan image. The deltas indicate the PFAA, which was 64 × 54 mm. The arrows indicate the hematoma inside the adductors. (B) Postoperative CT image. The delta point interposed the PFA. The hematoma inside the adductors decreased. (C) The 3-dimension image obtained by the CT scan. The deltas indicate the PFAA. The arrows indicate the terminal branches toward the muscles. (D) The 3-dimension image obtained by postoperative CT. The deltas point to the artificial graft. The arrows indicate the preserved branches from the PFA toward the muscles.
Emergency surgery was performed due to an aneurysmal rupture associated with severe anemia. The junction of the profunda femoris artery (PFA) and the terminal portion of the aneurysm were marked using ultrasonography preoperatively. The left CFA, which was severely calcified, and SFA were exposed. PFA was also exposed at the junction and caudal end of the aneurysm. The femoral vein and its branches were engorged. Heparin administration followed by clamping of the PFA inflow and outflow of the aneurysm was performed. The aneurysm was filled with an atheroma and hematoma. A branch containing retrograde blood flow to the aneurysm was ligated. Aneurysmal PFA was interposed with PROPATEN 6 mm (W. L. Gore Associates, Inc., CA, USA). Transfusion was performed during surgery due to severe anemia.
The patient’s postoperative recovery was uneventful. On postoperative Day 5, enhanced CT showed an interposed PFA with no complications, perforating branches originating from the distal portion of the interposed vessel and a reduction in the hematoma (Fig. 3B and D). The patient was discharged on postoperative Day 7.
DISCUSSION
PFAA is rare, accounting for 0.5% of peripheral aneurysms and 1–2.6% of all femoral aneurysms [1, 2]. PFAA tends to enlarge without being noticed and has a high frequency of rupture. The lifetime rupture rate was reported as 30–45% [3, 4]. Lawrence et al. reported that the rupture rate in asymptomatic PFAA was associated with a diameter > 5.7 ± 1.3 cm. They concluded that asymptomatic PFAA has a high risk of rupture with a diameter > 3.5 cm or intraluminal thrombus [5]. PFA is surrounded by the deep muscles in the thigh; however, the pressure from the muscles becomes weak in elderly patients with sarcopenia, which may lead to a high possibility of rupture. Rapid enlargement of the aneurysm leads to rupture; therefore, the present case should be considered as a possibility more frequently.
The patient was elderly and presented with sarcopenia which was diagnosed by the psoas muscle mass index [6]. His hemoglobin level decreased to 3.41 mmol/l, which was a lethal situation. The diagnosis was quickly made using ultrasonography and CT scan; however, the rupture point was not clearly discriminated. Intraoperative diagnosis of rupture was previously reported [7], but we could not identify the rupture point. The aneurysm was then replaced with heparin-bonded expanded polytetrafluoroethylene (PROPATEN). Interposition was performed because the left lower peripheral artery was affected by atherosclerosis, and the perforating arteries to the muscle described by the preoperative CT were better preserved. Ligation was an alternative choice if the aneurysm was limited to the distal PFA. Some studies have reported that if the ipsilateral femoropopliteal lesion is patent without stenosis, the ligation may be sufficient [4, 8, 9]. However, Igari et al. argued that PFAA should be treated with both aneurysmectomy and vascular reconstruction to preserve the PFA blood flow, which may positively affect future limb salvage [10]. We agree that reconstruction should be performed if the general condition is good. Moreover, the inflow branch to the aneurysm should be observed from inside the aneurysm and ligated, especially in patients with severe anemia preoperatively.
Lawrence et al. reported that a PFAA < 3.5 cm in diameter has a rare incidence of acute complications [5]. Harbuzariu suggested that elective surgery should be performed in low-risk patients with PFAA > 2 cm [3]. The cut-off value of surgical intervention for PFAA should be considered, including the aneurysmal diameter, surgical risk, the physical state of the patient and whether the intramural thrombus exists. Furthermore, patients with PFAA who are thin and sarcopenic should be followed-up closely, and surgical intervention should be considered in the early stage.
CONFLICT OF INTEREST STATEMENT
All authors have no conflict of interest.



