-
PDF
- Split View
-
Views
-
Cite
Cite
Masakatsu Hihara, Masashi Kihara, Toshihito Mitsui, Natsuko Kakudo, Atsuyuki Kuro, Kenji Kusumoto, Urethral functional reconstruction using a pedicled thigh flap for urethral cutaneous fistula after vulvar necrotizing fasciitis, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab363, https://doi.org/10.1093/jscr/rjab363
Close - Share Icon Share
Abstract
The penile and scrotal skin are often resected after vulvar necrotizing fasciitis, so functional and aesthetic vulvar reconstruction is extremely challenging. With widespread and deepened infections, urethral fistulas can develop, forcing penis and scrotal amputations. In cases complicated with a urethral fistula, the wound cannot be treated by simple skin graft surgery, and complicated flap surgery is required. We verified that urethral functional reconstruction using a pedicled thigh flap is a useful technique for managing urethral cutaneous fistulas that develop after necrotizing fasciitis.
INTRODUCTION
The penile and scrotal skin are often resected after vulvar necrotizing fasciitis, so functional and aesthetic vulvar reconstruction is extremely challenging. Urethral functional reconstruction using a pedicled thigh flap is a useful technique for managing urethral cutaneous fistulas that develop after necrotizing fasciitis.
CASE PRESENTATION
Case 1
A 47-year-old man was taken to our critical care center for septic shock due to necrotizing fasciitis, and his vulvar skin was extensively necrotic. Extensive skin necrosis further progressed, with about half of the total penile skin lost in the penis, bilateral testicular exposure and urethral cutaneous fistula. Two months after admission, the raw surface was able to be closed by mesh skin grafting, but the urethral cutaneous fistula widened steadily (Fig. 1).
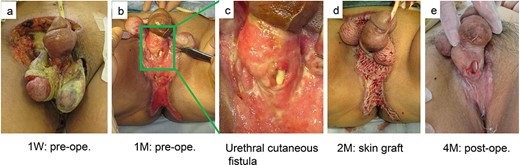
(a) A 47-year-old man was taken to our critical care center for septic shock due to necrotizing fasciitis, and his vulvar skin was extensively necrotic. (b, c) Extensive skin necrosis further progressed, with about half of the total penile skin lost in the penis, bilateral testicular exposure and urethral cutaneous fistula. (d, e) Two months after admission, the raw surface was able to be closed by mesh skin grafting, but the urethral cutaneous fistula widened steadily.
Although penectomy was also considered, his strong demand for penis preservation resulted in the development of a novel reconstructive plan 1 year after admission. First, the damaged tissue around the fistula was refreshed, and then the medial thigh perforator flap with the descending branch of the lateral femoral circumflex vessels was harvested. Second, epithelial component of the medial thigh perforator flap was inserted invertedly to the urethral mucosal defect, and the de-epithelized component of the flap was adhered to the de-epithelized penile dermis; consequently, the urethral cutaneous fistula was closed. Finally, a mesh skin graft was placed on the fat layer at the back of the flap to form a scrotum-like shape (Fig. 2).
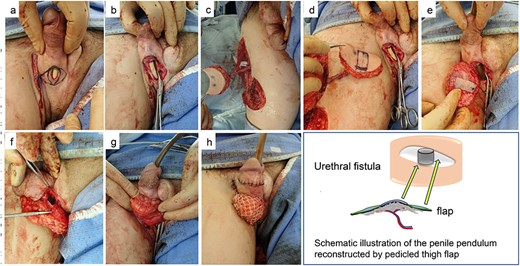
(a–c) One year after admission, the damaged tissue around the fistula was refreshed, and then the medial thigh perforator flap with the descending branch of the lateral femoral circumflex vessels was harvested. (d–f) Epithelial component of the medial thigh perforator flap was inserted invertedly to the urethral mucosal defect, and the de-epithelized component of the flap was adhered to the de-epithelized penile dermis; consequently, the urethral cutaneous fistula was closed. (g, h) A mesh skin graft was placed on the fat layer at the back of the flap to form a scrotum-like shape.
One year and 6 months after reconstruction, urethrography showed no relapse of the fistula.
The patient regained the ability to excrete residual urine in his bladder by himself with high urine flow rate (uroflowmetry; peak 23.8, average 12.1, voided volume 201, residual urine 0 ml). In addition, he regained the feeling of ejaculating through masturbation (Fig. 3).
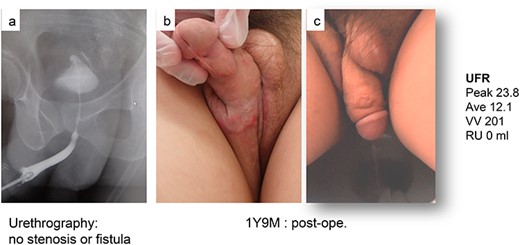
(a) One year and 6 months after reconstruction, urethrography showed no relapse of the fistula. (b, c) The patient regained the ability to excrete residual urine in his bladder by himself with high urine flow rate (uroflowmetry; peak 23.8, average 12.1, voided volume 201, residual urine 0 ml)
Case 2
A 62-year-old man developed sepsis after vulvar necrotizing fasciitis and underwent emergency incision and continuous lavage. Skin defects in the penile pendulum and scrotum developed 3 weeks later, consequently resulting in complication with urethral cutaneous fistula. To close the fistula, we planned reconstructive surgery using a veno-accompanying artery flap (VAF) [1] pedicled with the great saphenous vein and the accompanying artery of the cutaneous nerve. Using the same procedure as in Case 1, the de-epithelized component of the flap was extensively adhered to the de-epithelized penile dermis to close the urethral cutaneous fistula. Nine months after reconstruction, the fistula had not relapsed, but unfortunately, excreting urine by himself was still extremely difficult for the patient (Fig. 4).
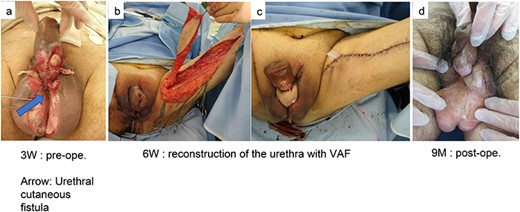
(a) A 62-year-old man developed sepsis after vulvar necrotizing fasciitis and underwent emergency incision and continuous lavage. Skin defects in the penile pendulum and scrotum developed 3 weeks later, consequently resulting in complication with urethral cutaneous fistula. (b) To close the fistula, we planned reconstructive surgery using a VAF pedicled with the great saphenous vein and the accompanying artery of the cutaneous nerve. (c) Using the same procedure as in Case 1, the de-epithelized component of the flap was extensively adhered to the de-epithelized penile dermis to close the urethral cutaneous fistula. (d) Nine months after reconstruction, the fistula had not relapsed, but unfortunately, excreting urine by himself was still extremely difficult for the patient
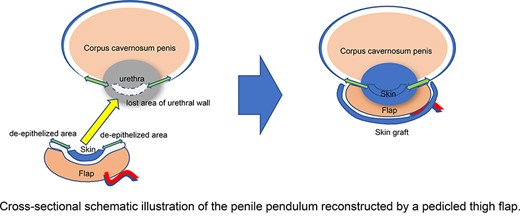
Cross-sectional schematic illustration of the penile pendulum reconstructed by a pedicled thigh flap.
DISCUSSION
In recent years, the number of cases of necrotizing fasciitis in Japan has been increasing because of the aging of the population and the increase in the prevalence of diabetes. Even after the septic shock period, urethral cutaneous fistula is often induced due to absolute debridement, making it difficult to reconstruct the vulva functionally and aesthetically.
Most reconstructive surgery of fistulas involves skin grafting, but penile amputation has frequently been applied in recent clinical practice. If the defect is confined to the skin, reconstruction of the vulvar skin defect, such as that using scrotal skin [2], a pudendal thigh flap [3], a local flap in the lower abdomen [4], using an outside-thigh flap [5], etc., can be applied. Especially in cases complicated with urethral fistulas due to a deep infection, local flap surgery using the surrounding skin is viable. However, this procedure has a high possibility of early recurrence of the fistula due to the low elasticity of the surrounding scar tissue and a low blood flow to the fragile skin.
To solve these problems, we devised a new procedure to reconstruct the urethral wall using pedicled distant thigh flaps. The epithelial component of the medial thigh perforator flap was inserted invertedly to the urethral mucosal defect, and the de-epithelized component of the flap had adhered to the de-epithelized penile dermis, consequently allowing the urethral cutaneous fistula to be closed (Fig. 5).
Only a few attempts have been made thus far at urethral reconstruction to imbue a self-urinating function after severe vulvar necrotizing fasciitis. This procedure is a novel and useful method that allows water-tight suturing and can cover the reconstructed urethra with a sufficient amount of tissue.
CONCLUSIONS
Reconstruction of a urethral cutaneous fistula after vulvar necrotizing fasciitis is challenging, but a pedicled distant thigh flap is useful for functional reconstruction of a urethral fistula.
AUTHOR CONTRIBUTIONS
Study design: M.H., N.K., M.K.
Data acquisition and analysis: T.M., A.K.
Drafting manuscript: M.H., N.K.
Critical revision of manuscript: K.K.
CONFLICT OF INTEREST STATEMENT
None declared.



