-
PDF
- Split View
-
Views
-
Cite
Cite
Peer W Kämmerer, Daniel Müller, Friedemann Linz, Priscila Ferrari Peron, Andreas Pabst, Patient-specific 3D-printed cutting guides for high oblique sagittal osteotomy—an innovative surgical technique for nerve preservation in orthognathic surgery, Journal of Surgical Case Reports, Volume 2021, Issue 8, August 2021, rjab345, https://doi.org/10.1093/jscr/rjab345
Close - Share Icon Share
Abstract
Bilateral sagittal split osteotomy (BSSO) of the mandible according to Obwegeser/Dal Pont is considered to be gold standard in orthognathic surgery. Frequently reported complications of BSSO are injuries of the mandibular nerve resulting in paresthesia/anesthesia as well as inadequate mandibular bone fracturing (‘bad split’). High oblique sagittal osteotomy (HOSO) was introduced to overcome these complications. We present an innovative HOSO modification using patient-specific 3D-printed cutting guides positioned on the outside of the ascending mandibular ramus and fixed in the incisura semilunaris, precisely marking the optimal height and angle of the osteotomy. Advantages are a decreased operation time due to the simplicity of this less invasive procedure, a potentially reduced frequency of mandibular nerve damage and bad splits as well as a lower bleeding risk.
INTRODUCTION
Surgical methods for mandibular osteotomy in orthognathic surgery underwent a multitude of modifications. Currently, bilateral sagittal split osteotomy (BSSO) according to Obwegeser/Dal Pont is most common and is performed in nearly 60% of cases. Major complications of BSSO in general are irritations and/or partial or even complete damage of the mandibular nerve in up to 20–50% of cases. This results in a sensitive deficit of the lower posterior teeth, the lower jaw’s vestibular soft tissues as well as the lower lip and chin area. For the affected patients, this is associated with a significantly reduced quality of life also resulting in professional impairments for those requiring lip sensitivity [1, 2]. Next, BSSO is dealing with a relevant number of unexpected and incorrect mandibular bone fractures (‘bad split’) with incidences reported of up to 2.3% [1]. Concerning the risk of severe bleedings during and after BSSO, a systematic review evaluated a mean blood loss of about 436 ml (±208 ml) [3]. To overcome these complications and to simplify the surgical procedure of BSSO, high oblique sagittal osteotomy (HOSO) was developed. Compared with BSSO, HOSO exclusively includes one single and complete horizontal osteotomy line above the mandibular foramen, dividing the ascending mandibular ramus in an upper part including the temporomandibular joint (TMJ) and a lower part including the lower teeth and mandibular nerve [4]. We present an innovative surgical technique using patient-specific 3D-printed cutting guides for intraoperative marking of the correct level of the mandibular nerve as well as the level and the angle of the osteotomy line in HOSO to overcome limitations such as nerve damage.

(A and B) The clinical baseline of the patient with a skeletal Class III (a) malocclusion with a rotation of the maxilla to the right and a rotation of the mandible to the left side (b: black lines).
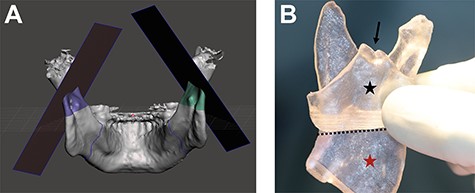
(A and B) Digital planning of the bilateral mandibular osteotomy (a). (b) 3D-printed model of the ascending mandibular ramus (red asterisk) including a patient-specific 3D-printed cutting guide for HOSO (black asterisk) positioned on the outside of the ascending mandibular ramus and fixed by hooking in the incisura semilunaris (black arrow). The 3D-printed cutting guide is marking the osteotomy line on the outside of the ascending mandibular ramus above the mandibular foramen (black line) as well as the angle of the osteotomy line.
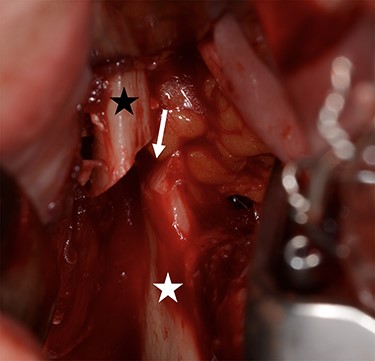
Intraoperative situation after HOSO osteotomy of the right ascending mandibular ramus (white arrow) demonstrating the ascending upper mandibular bone carrying the joint (black asterisk) and lower mandibular bone carrying the teeth (white asterisk).

Postoperative situation showing a normal occlusion without any nerve disturbances.
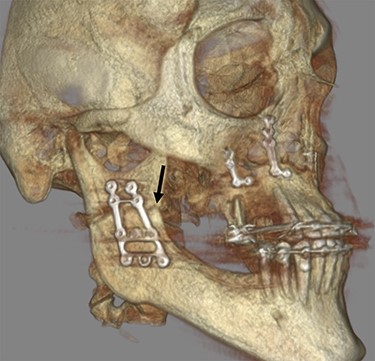
The 3D reconstruction of the postoperative CBCT scan is illustrating the right ascending mandibular ramus including the HOSO osteotomy line (black arrow) and the inserted osteosynthesis plates in the maxilla and the mandible after bimaxillary osteotomy.
CASE REPORT
A 33-year-old patient presented with a skeletal class III malocclusion. The planned surgical procedure included a LeFort I osteotomy of the maxilla with a forward displacement and midline rotation to the left as well as a bilateral mandibular displacement via HOSO with a midline rotation to the right (Fig. 1a and b). As part of the preoperative diagnosis and with a view to digital planning, a cone beam computed tomography (CBCT) scan was carried out and saved as a Digital Imaging and Communications in Medicine dataset. Using Medical Imaging Interaction Toolkit (version 2018.4.0), the CBCT dataset was segmented and converted into a *.stl dataset. The *.stl dataset was imported into Autodesk Meshmixer (version 3.5). After visualizing the inferior alveolar nerve and the mandibular foramen, the best possible osteotomy line for the high oblique mandibular osteotomy on the right and left ascending mandibular branches was planned digitally with a safety distance of 3 mm between the cranial osteotomy and the nerve entry point. In addition, the appropriate angles of the osteotomy line, both in the horizontal and in the vertical dimension, were planned. All information from the digital planning was then brought together in two saw templates for the right and left lower jaw. Those templates were designed for intraoperative fixation in the incisura semilunaris in order to maintain a secure position of the templates (Fig. 2a and b). Prior to the 3D-guided HOSO of the mandible, a LeFort I osteotomy of the maxilla was performed using piezosurgery and the prefabricated occlusal splint. For the correct positioning of the 3D-printed cutting guide for the mandibular osteotomy, preparation of the contact area at the outside of the ascending ramus up to the incisura semilunaris was necessary. After adjustment of the 3D guide, bilateral HOSO osteotomy was performed via piezosurgery following the predicted level of the osteotomy of the ascending mandibular ramus. From the lingual aspect of the ramus, a raspatory was inserted at the location of the osteotomy only. In accordance, neither the nerve nor the mandibular foramen was exposed in order to prevent traumatization (Fig. 3). After HOSO osteotomy on both sides, a realignment of the detached mandible to the newly adjusted maxilla with the final occlusal splint was performed, bringing the mandible into the precalculated position. Then, a bilateral osteosynthesis was carried out using mini-plates (MODUS® Mandible, Medartis®, Basel, Switzerland) and an angled screwdriver (KLS Martin, Tuttlingen, Germany; Fig. 4). The postoperative CBCT control showed regular osteotomy lines in the upper and lower jaw with the inserted osteosynthesis material (Fig. 5). So far, in the clinical course of 1.5 years, a stable situation without any nerve disturbances and no tendency to relapse was seen.
DISCUSSION
For HOSO, clinical advantages such as a reduced risk of mandibular nerve injury and/or damaging, a lower risk of unexpected fractures of the mandibular bone (‘bad split’), a decreased risk of intra- and postoperative bleeding episodes as well as a shorter operation time due to the simplicity of the surgical procedure was reported [4–6]. These complications could be further minimized using patient-specific 3D-printed cutting guides raising HOSO to a new surgical level. The reduced bone contact area in HOSO compared with BSSO might result in a less stable result including impaired wound healing and bone regeneration disturbances. In this context, not only the distance of mobilization but also the angle of HOSO is significantly relevant due to the resulting stress on the contact surface between the bone segments [7]. Three-dimensional-printed models and patient-specific 3D-printed cutting guides give the surgeon a precise guideline for the best angle, limiting the stress on the osteosynthesis plates and optimizing the bony contact area. In accordance, concerning 3D-printing technologies in orthognathic surgery, a significantly increased accuracy when using 3D-printed cutting guides for mandibular osteotomy was seen, and it was concluded that 3D-printing techniques can increase the frequency of optimal functional and esthetic outcomes, of surgical precision, and overall patient satisfaction [8]. Although patient-specific 3D-cutting guides were reported for BSSO, there is no literature available reporting about patient-specific 3D cutting guides for HOSO.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



