-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Alkhaibary, Noura Alsubaie, Ahoud Alharbi, Noor Alghanim, Sami Khairy, Makki Almuntashri, Mohammed Alwohaibi, Abdulaziz Alarifi, Ahmed Aloraidi, Ahmed Alkhani, Oculomotor nerve palsy following coronary artery bypass graft surgery: can pituitary apoplexy complicate the post-operative course of cardiac surgery?, Journal of Surgical Case Reports, Volume 2021, Issue 7, July 2021, rjab312, https://doi.org/10.1093/jscr/rjab312
Close - Share Icon Share
Abstract
Oculomotor nerve palsy, due to pituitary apoplexy, has been previously reported in the literature. However, the association with coronary artery bypass graft surgery (CABG) is rarely investigated. This article reports a case of pituitary apoplexy presenting with oculomotor nerve palsy following CABG. A 65-year-old male, known to have ischemic heart disease, diabetes mellitus and hypertension, presented with ptosis, diplopia and anisocoria that developed after 1 day of CABG. Radiological imaging demonstrated a pituitary adenoma with acute/subacute hemorrhage causing mild mass effect on the cavernous sinus. Considering the acute state of bypass surgery and pre-existing cardiac co-morbidities, expectant management was considered. The visual acuity and palsy gradually improved. Pituitary apoplexy, following CABG, is a rare phenomenon in the post-operative period. High index of suspicious is required to promptly identify high-risk patients to avoid further neurological sequelae.
INTRODUCTION
The oculomotor nerve consists of parasympathetic and general somatic efferent fibers [1]. Together, these fibers mediate pupillary constriction, elevation of the eyelid through the levator palpebrae superioris and movement of most extra-ocular muscles, namely, the medial rectus, superior rectus, inferior rectus and inferior oblique muscles [1].
The development of oculomotor nerve palsy after coronary artery bypass graft surgery (CABG) is rare. A review of the literature reveals few reported cases. Considering the rarity of such phenomenon, we hereby report the clinical presentation, radiological imaging and outcome of a patient with oculomotor nerve palsy following CABG. In addition, a review of the pertinent literature is discussed.
CASE DESCRIPTION
Clinical presentation
A 65-year-old male, known to have three-vessel coronary artery disease, diabetes mellitus and hypertension, was referred to the neurosurgery department due to ptosis and anisocoria that developed 1 day after CABG. The patient was noted to have right ‘eyelid drop, dilated pupil and double vision’ upon elevation of the eyelid. The patient reported no history of headache, vomiting, loss of consciousness, symptoms suggestive of brainstem involvement or pituitary axis hypo/hypersecretion upon initial presentation.
Physical examination
The patient was vitally stable, alert and oriented to person, place and time with a Glasgow coma scale (GCS) of 15/15. There was right-sided paresis of the levator palpebrae superioris and the extra-ocular muscles; medial rectus, superior rectus, inferior rectus and inferior oblique muscles with a 5-mm dilated pupil. The left eye extra-ocular muscles were intact. The left pupil measured 3-mm and was reactive to light and accommodation with no gaze preference. The visual acuity was slightly impaired. The remainder of the neurological examination was unremarkable.
Neuroradiological imaging
Computed tomography (CT) scan revealed widening of the sella turcica with an isodense soft tissue lesion in the pituitary gland (Fig. 1A). Magnetic resonance imaging (MRI) demonstrated a pituitary adenoma with acute hemorrhage causing right-sided mild mass effect on the cavernous sinus (Fig. 1B–D).
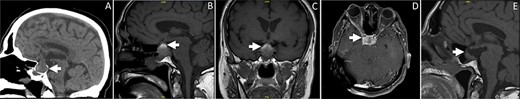
(A) Sagittal brain CT showing an isodense lesion in the pituitary gland associated with widening of the sella turcica. The lesion is causing a slight displacement of the pituitary stalk and optic chiam. (B–C) Sagittal and coronal sections of T1-weighted brain MRI without contrast. The MR images are demonstrating heterogneous signal of the pituitary lesion. The lesion is mainly hyperintense on T1-weighted images, indicating acute to subacute hemorrhage. The lesion is involving the sella and suprasellar region. (D) Axial T1-weighted brain MRI post contrast demonstrating enhancement of the pituitary lesion. (E) Sagittal MRI of the sella showing marked interval reduction in the size of the hemorrhagic cystic pituitary lesion. The small residual is measuring 1.1 × 0.5 cm. Interval resolution of the mass effect on the optic chiasm is noted.
Outcome and follow-up
The diagnosis of pituitary apoplexy was established after brain CT and MRI. Follow-up images showed marked improvement in the size of the cystic hemorrhagic pituitary lesion (Fig. 1E). Given the improvement of symptoms, the stable condition of the patient, the acute state of bypass surgery and the high-risk of peri-operative cardiac events under general anesthesia, conservative management was considered. Upon follow-up, the patient developed central hypoadrenalism and hypothyroidism. The patient is currently followed-up in neurosurgery, ophthalmology and endocrine clinics. The visual acuity and palsy had gradually improved.
DISCUSSION
Oculomotor nerve palsy due to pituitary apoplexy after CABG is uncommon. A review of the reported data in the literature identified only a few reported cases. We report an additional case encountered at our institution. The patient in the present case developed oculomotor nerve palsy with pupillary involvement, consistent with isolated, complete third cranial nerve palsy.
Oculomotor nerve palsy following CABG can develop secondarily to pituitary apoplexy or ischemic midbrain infarction [1, 2]. The pupils are commonly spared in patients who develop midbrain infarction after cardiac surgery [1]. As such, pupillary involvement serves as a physical finding to localize the lesion and its possible underlying culprit [1]. Furthermore, patients with midbrain infarction commonly present with additional brainstem-related deficits including, but not limited to, motor weakness, coma, locked-in syndrome and Horner’s syndrome [3, 4].
Multiple mechanisms have been proposed to elucidate pituitary apoplexy presenting with oculomotor nerve palsy after cardiac surgery. However, no single attributable cause can be identified to explain such phenomenon [2]. Some of the plausible implicated pathophysiological mechanisms include: decreased cerebral perfusion, extracorporeal bypass, embolization and intraoperative dampened arterial blood pressure, leading to ischemia of the pituitary gland with subsequent infarction [2, 5–7]. In turn, neuro-ophthalmological deficits tend to develop within 48 h of CABG, owing to the acute necrosis and hemorrhage within the pituitary adenoma. Subsequently, it causes mass effect on the adjacent para-sellar and suprasellar structures [2, 8].
Patients with pre-existing subclinical pituitary adenoma are susceptible to apoplexy after open cardiac surgery [2]. Therefore, healthcare providers should keep a high index of suspicion to promptly identify patients with the initial presentation of ophthalmoplegia, endocrinopathy, altered mental status or coma [2]. In the absence of early diagnosis, pituitary apoplexy can result in permanent neurological deficits, endocrinological disturbance requiring replacement and/or fatal outcome.
In the present case, all neuroradiological investigations were considered to search for alternative causes of pituitary apoplexy that may account for oculomotor nerve palsy after CABG. As such, the diagnosis was rendered after a thorough assessment of the patient. Although the clinical manifestations of the case are consistent with what has been previously reported in the literature, the present article discusses one of the acute possible causes of unexplained, isolated oculomotor nerve palsy in patients who undergo CABG.
CONCLUSION
Pituitary apoplexy, following CABG, is a rare phenomenon in the post-operative period of cardiac surgery. Such patients may present with unilateral pupillary dilation, ptosis and diplopia. High index of suspicious is required to promptly identify such complication to avoid further neurological sequelae.
CONFLICT OF INTEREST STATEMENT
The authors declare that the article content was composed in the absence of any commercial or financial relationship that could be constructed as a potential conflict of interest. The authors declare that they have no conflict of interest.
FUNDING
None.
References
Cooper DM, Bazaral MG, Furlan AJ, Sevilla E, Ghattas MA, Sheeler LR, et al.
- myocardial ischemia
- hypertension
- coronary artery bypass surgery
- diabetes mellitus
- cardiac surgery procedures
- hemorrhage
- diplopia
- anisocoria
- cavernous sinus
- oculomotor nerve diseases
- paralysis
- pituitary apoplexy
- postoperative period
- surgical procedures, operative
- visual acuity
- diagnostic imaging
- heart
- morbidity
- watchful waiting
- surgery specialty
- pituitary adenoma
- bypass
- cerebral mass effect
- neurologic complications



