-
PDF
- Split View
-
Views
-
Cite
Cite
Marcus Vinicius Danieli, João Paulo Fernandes Guerreiro, Alexandre Oliveira Queiroz, Guilherme José Miyasaki Piovesana, Early tibial component loosening of medial UKA after severe medial plateau SONK—report of three cases, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab242, https://doi.org/10.1093/jscr/rjab242
Close - Share Icon Share
Abstract
Spontaneous osteonecrosis or subchondral bone insufficiency fracture of the knee is a frequent injury in elderly female patients. The medial femoral condyle followed by the medial plateau is the most prevalent sites. When its evolution after conservative treatment is not favorable, medial unicompartimental arthroplasty is a surgical option with good results. We report three cases of early tibial component loosening of medial unicompartimental arthroplasty that could be related to a severe subchondral bone insufficiency fracture of the tibial plateau. In these cases of severe involvement of the tibial plateau, a more careful evaluation would be recommended to choose between unicompartimental and total knee replacement to avoid this early loosening.
INTRODUCTION
Spontaneous osteonecrosis of the knee (SONK), also known as subchondral bone insufficiency fracture of the knee (SIFK), is described as a subchondral bone injury, with uncertain pathogenesis [1]. Primary vascular insult, mild trauma in an osteoarthritic joint, meniscal injuries and even osteoporosis are cited as possible related factors [1–4]. This disease affects more females over 60 years old [4]. The most frequent affected site is the medial femoral condyle (MFC), followed by the medial plateau (MP) [4].
Conservative treatment with rest, analgesics and avoid weight bearing on the affected limb is effective in most of the cases [4]. However, in some patients, the evolution may not be favorable. In these situations, unicompartimental knee arthroplasty (UKA) would be a possible solution.
UKA surgery has evolved in recent years due to implant design, surgical technique improvements and better patient selection [5, 6]. This surgery would have the advantage of preserving bone stock, less surgical trauma, faster recovery and better functional results when compared with total knee replacement (TKR) [7, 8]. Despite this, the rate of early revisions (before 2 years after surgery) is higher in UKA [5–9]. In these early failures, aseptic tibial loosening is cited as the most common cause [5–8, 10, 11]. However, literature does not relate this failure to the previous existence of a severe SIFK.
Thus, we report three cases of early tibial component aseptic loosening of medial UKA in patients with previous severe MP SIFK.

Left knee T2 coronal MRI (top left) showing MP and femoral condyle SIFK with articular failure of both surfaces; Top right: same image (T1); Bottom left: orthostatic anterior view X-ray image of the same patient showing medial compartment bone-on-bone contact; Bottom right: lateral view X-ray image of the same patient.

Top: anterior (left) and lateral view (right) X-ray images of the immediate postoperative period (medial UKA); Bottom: anterior (left) and lateral view (right) X-ray images of the same patient with 5 months of follow-up with tibial component loosening.
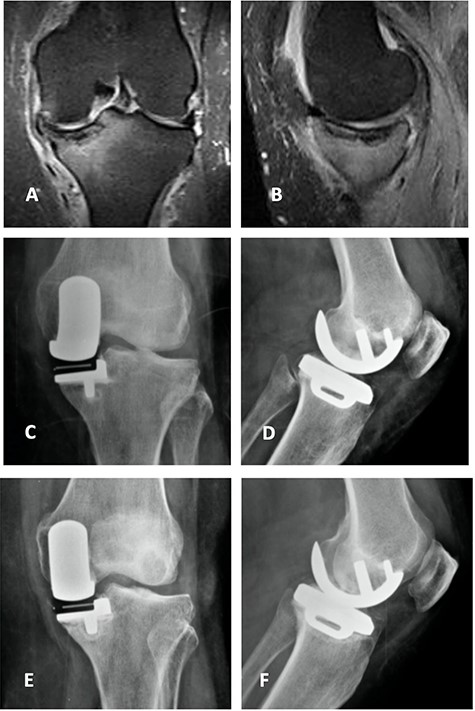
Coronal (A) and sagittal (B) T2 MRI—left knee—showing severe MP SIFK; Anterior (C) and lateral view (D) X-ray images of immediate postoperative period (medial UKA); Anterior (E) and lateral view (F) X-ray images with 3 months of follow-up with tibial component loosening.
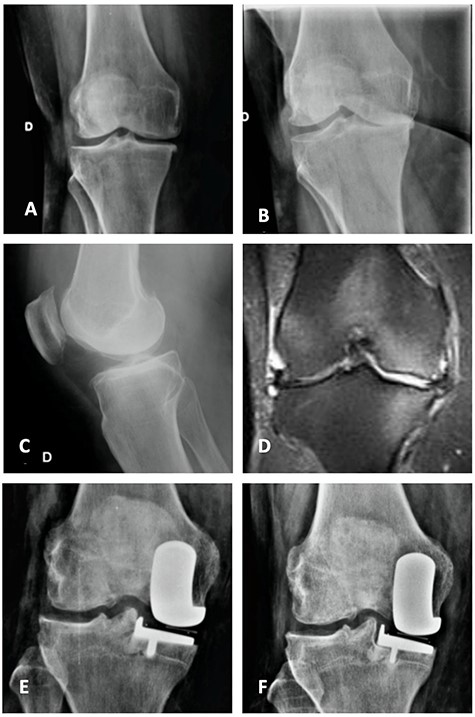
Orthostatic anterior view (A) and Rosenberg (B) X-ray images with medial osteoarthritis—right knee; Lateral view X-ray image of the same knee (C); T2 coronal MRI (D) with severe MP and femoral condyle SIFK; Immediate postoperative X-ray image (E) and 3 months after surgery (F) showing tibial component loosening.
CASES REPORT
The study was authorized by the research ethics committee (CAAE: 40632520.7.0000.5696). All patients signed a Consent Form for use of clinical data and images, respecting their anonymity.
Between August 2017 and August 2020, we performed medial mobile bearing UKA (Oxford®—Biomet) on 35 knees (31 patients). Of these, in 26 the surgical indication was due to anteromedial osteoarthritis, in 2 due to MFC SIFK, in 4 due to MP SIFK and in 3 patients due to SIFK in the MFC and MP. Early failure occurred in five patients, one due to instability and four to aseptic loosening. Of these last four patients, one had anteromedial osteoarthritis, and the other three are the patients reported here. There were no cases of femoral component loosening.
The three patients were female, aged between 66 and 70 years old. They had history of sudden onset knee pain (two left and one right knee). Magnetic resonance images (MRI) showed severe MP SIFK in all cases and involvement of the MFC in two cases. After a minimum of 3 months of conservative treatment, none of the patients showed improvement. Thus, medial cemented UKA (Oxford®—Biomet) was indicated.
To indicate surgery preoperative X-rays were performed, in addition to MRI of the affected knee [11].
During surgery good bone was observed, leading to adequate cementation. Patients had good outcomes for 3 months, restarting pain symptoms after that (in the medial side, worse when standing or walking). X-ray images showed tibial component loosening in the three cases (Figs 1–4). Septic loosening was ruled out with blood tests and joint aspiration to analyze liquid cellularity and culture.
All patients underwent revision surgery, where the tibial component loosening was confirmed.
DISCUSSION
SONK has its name under discussion because some authors suggest that necrosis is not the main involved factor. Due to its relationship with mechanical overload and focal stress on the subchondral bone resulting in small fractures, the suggestion is this would better be called subchondral bone insufficiency fracture [1, 3, 12].
This pathology affects more elderly female patients, where the incidence of osteopenia or osteoporosis is more frequent. Despite this, the bone mass deficit has not been definitively correlated [2, 9].
Some risk factors are related to worse prognosis like meniscal extrusion, a SIFK affecting >40% of the involved site, advanced age, varus alignment and Kellgren & Lawrence radiographic classification > III [3, 4, 12]. In our reported cases, all patents presented large involvement of the MP (> 40%).
When evolution is not favorable with unicompartimental involvement without ligament failure, reducible varus deformity <15°, flexion deformity <15°, minimum range of motion of 100° (under anesthesia) and absence of rheumatological diseases, the UKA would be an effective option [11].
Bergeson et al. [7] showed that UKA has a 10 and 20 years survival rate of 98 and 91%, respectively, being the tibial aseptic loosening the main cause of early failure. This was confirmed by other authors but without associating with the surgery indication (osteoarthritis or SIFK) [5, 6, 10].
The implant used in our patients has a mobile bearing. Finite element analysis studies have already shown this prosthesis increases the tension forces just below the tibial component in the immediate postoperative period [11]. Thus, if the bone is not of good quality an early loosening could have a greater chance of occurring (author’s hypothesis). If the SIFK is very extensive, this bone may be compromised and cannot support this increased tension force. Our cases demonstrated this is a possible theory, because such failure did not occur in other cases without severe involvement of subchondral bone (Fig. 5). The use of mobile or fixed bearing implants could be a concern. However, literature shows no difference related to clinical outcomes, radiographic evaluation, revision rates and survivorship [13].

Top: coronal (left) and sagittal (right) T2 MRI with MP SIFK and a mild articular irregularity; Bottom: anterior (left) and lateral view (right) X-ray images 2 years after surgery with good clinical and functional results.
Kaneko et al. [14] suggests evaluating the tibiofemoral angle and the tibial component alignment as risk factors for UKA postoperative complications. LoPresti et al. [8] cites the main factor related to complications would be articular line changes in coronal plane. However, no article relates the degree of tibial plateau SIFK involvement with early component loosening.
The cemented UKA are related to higher incidence of radiolucent lines (RLL) not related to pain, poor clinical outcomes or survivorship compromising compared with cementless [11, 15]. In our cases, RLL were not innocent because of the patients’ symptoms.
Our series of medial Oxford® UKA shows that early failure due to aseptic tibial component loosening is a concern that repeats literature experience. Thus, in cases of surgery indication with severe affected tibial plateau by SIFK, perhaps it would be safer to perform a TKR, for better load distribution and to prevent such complication.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interests.



