-
PDF
- Split View
-
Views
-
Cite
Cite
Shih-Feng Huang, Wen-Chung Liu, A rare case of primary cutaneous diffuse large B-cell lymphoma, leg type, presenting as cellulitis: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab227, https://doi.org/10.1093/jscr/rjab227
Close - Share Icon Share
Abstract
Primary cutaneous diffuse large B-cell lymphoma, leg type, accounts for only 4% of all cutaneous lymphomas and bears a worse prognosis than other cutaneous B-cell lymphomas. Diagnosis at an early stage may be difficult due to its nonspecific manifestations. We report an 88-year-old female who was brought to our emergency department due to two rapidly growing painful skin lesions with local redness and swelling on her right lower leg. We performed incisional biopsy of the two right lower leg skin lesions and sent the specimens for histopathological examination. The pathological examination was compatible with diffuse large B-cell lymphoma. Primary cutaneous diffuse large B-cell lymphoma, leg type, is a rare condition that can present as skin cellulitis, thereby misleading clinicians and resulting in delayed treatment. This diagnosis should be considered when assessing skin lesions.
INTRODUCTION
Primary cutaneous B-cell lymphomas (PCBCL) are a group of extranodal non-Hodgkin’s B-cell lymphomas, which are mainly characterized by primary skin involvement without extracutaneous disease at the time of diagnosis. PCBCLs were previously classified into three distinct subtypes by the World Health Organization: primary cutaneous marginal zone lymphoma, primary cutaneous follicle center lymphoma and primary cutaneous diffuse large B-cell lymphoma, leg type (PCDLBCL, LT) [1]. Additionally, in an update in 2018, a new provisional entity of Epstein–Barr virus positive mucocutaneous ulcer was included [2]. Among all the PCBCLs, PCDLBCL, LT has the worst prognosis, with a 5-year disease-specific survival between 40 and 60%. Recurrences and extracutaneous progression are common, including central nervous system involvement [3]. The aim of this case report is to report a rare case of PCDLBCL, LT, which initially presented as cellulitis.
CASE REPORT
An 88-year-old woman with dementia was brought to our emergency department (ED) due to two rapidly growing painful nodules on her right lower leg. Due to her dementia, the medical history was mostly obtained from her son, and the informed consent for this case report was signed by her son. She had poor performance status and was capable of only limited selfcare (Eastern Cooperative Oncology Group Performance Status Scale grade 3). She was confined to the bed or chair most of the time and was normally cared for at a nursing home. According to her son, the nodule on her right anterior lower leg appeared about 3 weeks previously, and she had begun to complain of right lower leg pain. The other tumor was located at the medial aspect of her right lower leg, and it had appeared only 1 week previously. The two nodules had grown rapidly, with increasing pain. She denied experiencing fever, night sweats or weight loss in recent months. She had been seen at a local clinic prior to her ED presentation. At the clinic, antibiotics had been prescribed and a needle aspiration of the larger skin lesions was attempted. No pus or fluid could be aspirated, and despite antibiotic treatment, the lesions were getting larger. Thus, she was transferred to our ED for further evaluation and treatment.
Physical examination revealed two red and violaceous skin lesions over the right lower leg, ~9 and 3 cm in size, respectively. The lesions were erythematous, had ill-defined borders and were tender on palpation. Local heat and swelling of the skin around the lesions were also noted. Laboratory data, including a complete blood count and biochemical studies, revealed no significant findings. Contrast-enhanced computed tomography of the lower limbs revealed an abnormal space-occupying lesion about 9 cm × 7.5 cm × 3.3 cm in size, at the anterior aspect of the right lower leg. It showed heterogeneous density, heterogeneous contrast enhancement, and involvement of the subcutaneous area, superficial fascial planes and muscle layer. Another small non-specific lesion about 3 cm in size was located at the medial aspect of the right lower leg, with similar radiological features (Fig. 1). With a provisional diagnosis of skin tumors with associated cellulitis of the right lower leg, she was subsequently admitted to our institution for further investigations and antibiotic treatment.

The picture shows (A) the skin lesion located at the anterior aspect of right lower leg (black star sign) after incisional biopsy; (B) the other lesion located at the medial aspect of right lower leg (black triangle) after incisional biopsy.
After admission, we performed incisional biopsy of the skin tumors (Fig. 2) and the specimens were sent for histopathological examination and bacterial/tuberculosis/fungal culture. An antibiotic (oxacillin 2 g every 6 hours) was administered as empiric therapy for cellulitis. Three days later, bacterial culture and tuberculosis acid-fast stain testing provided negative results. A week later, histopathological results indicated a malignant lymphoma. There was diffuse infiltration of large, atypical lymphocytes with centroblast and immunoblast features in the whole dermis without epidermal involvement. Immunohistochemical staining revealed the following results: CK AE1/AE3(−), CD3(−), CD20(+), CD30(−), BCL-2(+), CD10(− to dim, −/+), BCL-6(dim,−/+), MUM1(+), Cyclin-D1(−), Ki-67(85%) and IgM(−) (Fig. 3). The results were compatible with a diffuse large B-cell lymphoma, either primary or secondary. There was no evidence of lymphadenopathy elsewhere. Based on clinical and histopathological findings, a diagnosis of PCDLBCL, LT was made. The case was later referred to a team of oncologists, and her family refused further management due to old age. Therefore, the patient then received hospice palliative care.
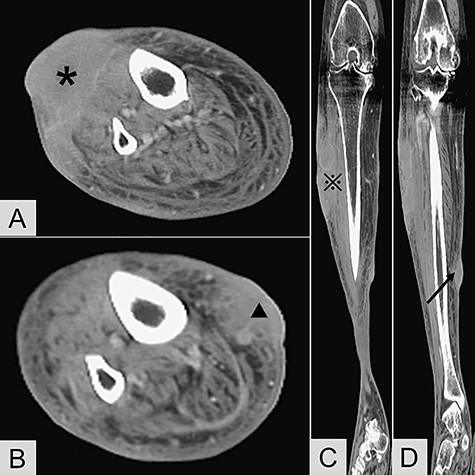
Contrast-enhanced computed tomography revealed (A) transverse view of the anterior lesion of right lower leg (*); (B) transverse view of the medial lesion of right lower leg (▲); (C) coronary view of the anterior lesion ( ); (D) coronary view of the medial lesion (black arrow).
); (D) coronary view of the medial lesion (black arrow).
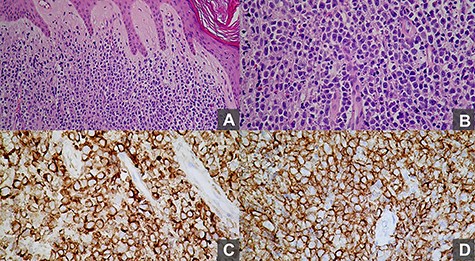
Histopathological examination revealed (A) monotonous, diffuse and non-epidermotropic infiltration of confluent sheets of immunoblasts and centroblasts (H&E, 20×); (B) monotonous and confluent sheets of immunoblasts and centroblasts, many with a striking round cell morphology (H&E, 40×); (C) the large lymphocytes are positive for Bcl-2 immunohistochemical staining (40×); (D) the large lymphocytes are CD20-positive B-cells (40×).
DISCUSSION
PCDLBCL, LT is a rare condition for a surgeon to encounter and represents only 4% of all cutaneous lymphomas. Compared with other cutaneous lymphomas, it has a significantly worse prognosis, with a 5-year overall survival of only 50–60% [4]. Owing to its aggressiveness, it is critical to diagnose PCDLBCL, LT, at an early stage, though this is often difficult. Diagnosis can be challenging due to non-specific symptoms and signs. Primary cutaneous B-cell lymphomas primarily involve the skin; however, the appearance of the skin lesion may vary from obvious masses, plaques or nodules to only redness and mild swelling that can mimic skin or soft tissue infection such as cellulitis and mislead less-experienced clinicians. Mistaking cutaneous diffuse large B-cell lymphomas for skin cellulitis may result in not only unnecessary interventions, such as needle aspiration or incision and drainage, but also a delay to proper antineoplastic treatment [5]. In this case report, we provide detailed clinical history and photographs of the skin lesions found in this condition. Nonetheless, as the patient’s son did not wish for further treatment, we were unable to report treatment-related outcomes in this case.
Due to a lack of randomized controlled trials, treatment recommendations for cutaneous B-cell lymphomas are mostly based on retrospective studies and experts’ experience. A multidisciplinary approach is required, with input from dermatology, medical oncology and radiation oncology. Many aspects of the natural history of PCDLBCL, LT are similar to those of systemic lymphoma. Therefore, systemic chemotherapy using a rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone regimen has been utilized for the treatment of PCDLBCL, LT and may be associated with improved remission and relapse rates [6].
In conclusion, PCDLBCL, LT is a rare condition that can mimic skin cellulitis initially. Early diagnosis is difficult because of its vague clinical presentation. This diagnosis should be considered in patients whose cellulitic skin lesion is refractory to empiric antibiotic treatment.
References
- edema
- b-lymphocytes
- cellulitis
- aged adult, 80 and over
- emergency service, hospital
- diffuse large b-cell lymphoma
- pain
- skin neoplasms
- diagnosis
- leg
- lower leg
- skin
- skin lesion
- incisional biopsy
- cutaneous lymphomas
- primary cutaneous b-cell lymphoma
- primary cutaneous diffuse large b-cell lymphoma
- histopathology tests
- time-to-treatment



