-
PDF
- Split View
-
Views
-
Cite
Cite
Tetsuya So, Naoki Yamashita, Hidehiko Shimokawa, Masatoshi Yamaoka, Daigo Kawano, Takashi Yoshimatsu, Tsunehiro Oyama, Paraneoplastic limbic encephalitis due to lung squamous cell carcinoma, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab156, https://doi.org/10.1093/jscr/rjab156
Close - Share Icon Share
Abstract
Paraneoplastic limbic encephalitis (PLE) is one of paraneoplastic neurological syndrome (PNS). We herein report a case of PLE due to lung squamous cell carcinoma. A 80-year-old woman visited because of several neurological symptoms. Brain magnetic resonance imaging revealed hyperintense signals at the splenium of the corpus callosum, suggesting limbic encephalitis. Chest X-ray and computed tomography showed a 17 × 14 mm tumor in the left lung field, suggesting lung cancer. Surgical examination revealed T1bN0M0 lung squamous cell carcinoma. She died 50 days after surgery due to the rapid progression of encephalitis. PLE is an extremely rare disorder, and even a case in the early stage of cancer shows poor prognosis. We should doubt a possibility of PLE, and detailed brain examination should be performed in case of consciousness disorder with rapid progression in the cancer patient.
INTRODUCTION
Paraneoplastic limbic encephalitis (PLE) is one of paraneoplastic neurological syndrome (PNS) [1]. PNS is a diverse group of disorders that can affect any part of the nervous system and is thought to be caused by autoimmune processes triggered by the cancer [2]. We herein report an extremely rare case of PLE due to lung squamous cell carcinoma.
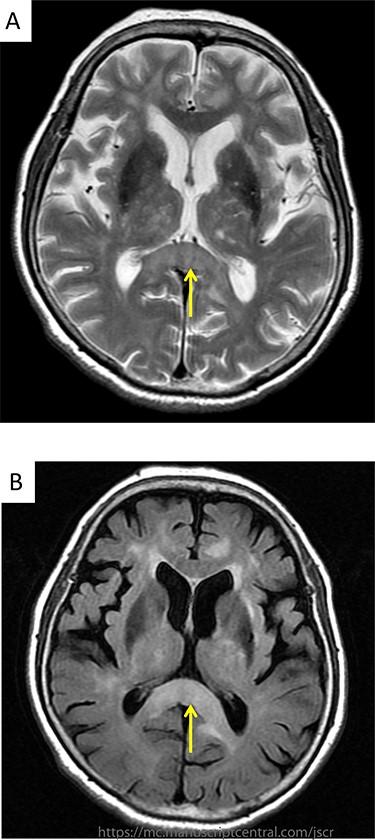
(A) Brain MRI revealed hyperintensity signals on T2-weighted image at the splenium of the corpus callosum; (B) brain MRI revealed hyperintensity signals on FLAIR images at the same region.
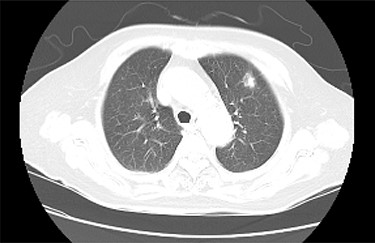
Chest CT detected a nodule with an irregular margin measuring 17 × 14 mm in size at the subpleural area of the left upper lobe S3 of the lung.
CASE REPORT
A 80-year- Japanese woman first visited our hospital in March 2017 with several neurological symptoms such as headache, incontinence, wobble and consciousness disorder (Glasgow Coma Scale: 14). She was a smoker (from 18 to 80 years of age, one pack per day, Brinkman Index: 1240) and had no family history of malignancies. Brain magnetic resonance imaging (MRI) revealed hyperintense signals on T2-weighted (Fig. 1A) and fluid attenuation inversion recovery (FLAIR) images at the splenium of the corpus callosum (Fig. 1B). These findings were compatible with limbic encephalitis. A cerebrospinal fluid analysis showed inflammation with negative cytology, and an electroencephalogram demonstrated normal study. Because PLE due to malignant tumor was suspected, a systemic examination was performed. Chest computed tomography (CT) detected a nodule with an irregular margin measuring 17 × 14 mm in size at the subpleural area of the left upper lobe S3 of the lung (Fig. 2). The enhanced systemic CT and brain MRI detected neither regional lymph node swelling nor distant metastases, and then it was classified as clinical stage T1bN0M0 according to the eighth edition of the TNM classification by International Association for the Study of Lung Cancer (IASLC). Her conscious level was worsening (Glasgow Coma Scale: 5). After obtaining informed consent, lung partial resection was performed via video-assisted thoracic surgery (VATS). The permanent pathological examination revealed squamous cell carcinoma (keratinizing type) (Fig. 3), and it was classified as pathological stage T1bN0M0. Anti-Hu antibody, one of onconeural antibodies, was investigated as part of the workup for PLE, but the result was negative. Her post-operative course was uneventful, but she died 50 days after surgery caused by the rapid progression of encephalitis.
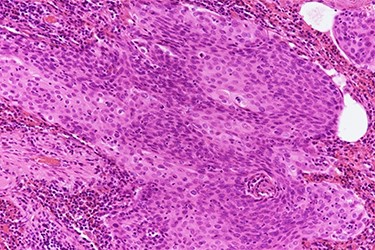
Histopathologic slide shows keratin pearls of squamous cell carcinoma (hematoxylin and eosin stain, 200× magnification).
DISCUSSION
PNS is an extremely rare disorder caused by the remote effects of cancer and causes severe neurological dysfunction. PNS is also considered as immune response to the molecules on cancer which cross-react with self-antigens in the nervous system. Henson and colleagues first reported mental disorder associated with cancer in 1954 [3]. There have only been a few studies addressing the incidence and prevalence of PNS in the overall cancer types. Among the cancer types, small cell lung cancer (SCLC) accounts for about half, while non-small cell lung cancer (NSCLC) is very rare and only 4~10% of the total [4]. Corsellis and colleagues first described limbic encephalitis and its association with cancer in 1968 [5]. According to the medical database, only three manuscripts have been described about the case of lung squamous cell carcinoma with PLE, therefore our case seems to be rare.
The diagnosis of PLE required the neurological symptoms and the existence of cancer. Furthermore, several examinations such as brain MRI, cerebrospinal fluid analysis and onconeural antibody assessment might assist in making this diagnosis as well [4]. A variety of onconeural antibodies, including anti-Hu, anti-Ma1 and Ma2 and anti CV2, have been associated with PLE. Among them, anti-Hu antibody was usually found in patients with SCLC but rarely in patients with NSCLC. Gultekin and colleagues also observed neurological improvement by cancer treatment in 38% of patients with anti-Hu antibody and 64% of patients without onconeural antibodies [4]. In our case, these findings were almost compatible with PLE. Therefore, the presence of anti-Hu antibody was considered as a poor neurological prognostic factor.
In conclusion, PLE is an extremely rare disorder, and even a case in the early stage of cancer shows poor prognosis. We should doubt a possibility of PLE, and detailed brain examination should be performed in case of consciousness disorder with rapid progression in cancer patient.
ACKNOWLEDGEMENTS
We thank all staff of Shinkomonji Hospital for their professional help.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



