-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroaki Shidei, Shota Mitsuboshi, Koen Akihiro, Hiroe Aoshima, Tamami Isaka, Masato Kanzaki, Robot-assisted thoracoscopic surgery using a narrow-profile vascular stapler through an 8-mm robotic port, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab157, https://doi.org/10.1093/jscr/rjab157
Close - Share Icon Share
Abstract
The number of robot-assisted thoracoscopic surgery (RATS) procedures performed for thoracic disease has been increasing. Recently, a narrow-profile vascular stapler (Signia small-diameter reload, Covidien Japan, Tokyo, Japan) has been developed to provide superior access and precise staple placement in video-assisted thoracoscopic surgery (VATS) procedures. A 70-year-old man who was an exsmoker visited our hospital with a complaint of coughing. Chest computed tomography revealed a tumor with a cavity, ~55 mm in diameter, in the right-middle lobe. A 4-arm RATS right-middle lobectomy was performed with a 4-cm utility thoracotomy with da Vinci Xi (Intuitive Surgical, Sunnyvale, CA, USA). The pulmonary vessels were divided using a narrow-profile vascular stapler through an 8-mm port. No complications occurred in the postoperative course. With a narrow-profile vascular stapler, portal RATS can be performed after VATS lung biopsy using 8-mm ports.
INTRODUCTION
After treatments for malignant lung and mediastinal tumors have been covered by the national health insurance since 2018, thoracoscopic surgery has been actively performed, but the proportion of robot-assisted thoracoscopic surgery (RATS) has increased in Japan [1]. In portal RATS lobectomy/segmentectomy, robotic trocars are usually used via three 8-mm ports and one 12-mm port. The conventional endoscopic stapler cannot pass through the 8-mm port, so 8- to >10-mm ports were used instead. Recently, a narrow-profile vascular stapler has been developed to provide superior access and precise staple placement in video-assisted thoracoscopic surgery (VATS) procedures. Currently, a narrow-profile vascular stapler with an 8-mm-diameter shaft and 6.3-mm-diameter anvil that can be used through an 8-mm robotic port is being developed and can be used with the body of a conventional stapler. Therefore, this narrow-profile vascular stapler (Signia small-diameter reload, Covidien Japan, Tokyo, Japan) can be used through an 8-mm robotic port.
Herein, we report a successful case of using RATS with a narrow-profile vascular stapler through an 8-mm port.
CASE REPORT
A 70-year-old man who was an exsmoker visited our hospital with a complaint of coughing. The patient had undergone thyroid cancer surgery and had atrial fibrillation. His vital signs showed no abnormalities as follows: temperature, 36.3°C; blood pressure, 106/78 mm Hg; heart rate, 91 beats; respiratory rate, 16 breaths per minute; and oxygen saturation, 98% in room air. His laboratory data showed the following values: serum carcinoembryonic antigen, 1.1 ng/ml (normal, < 5 ng/ml); serum progastrin-releasing peptide, 35.5 pg/ml (normal, <81 pg/ml); serum squamous cell carcinoma-associated antigen, 1.3 ng/ml (normal, <1.5 ng/ml); and serum cytokeratin 19 fragment, 2.9 ng/ml (normal, <3.5 ng/ml).
Chest radiography revealed an abnormal shadow in the right-middle lung field (Fig. 1A). Chest computed tomography (CT) revealed a tumor with a cavity, ~55 mm in diameter, in the right-middle lobe (Fig. 1B). The tumor was diagnosed as a lung squamous cell carcinoma by transbronchial biopsy.
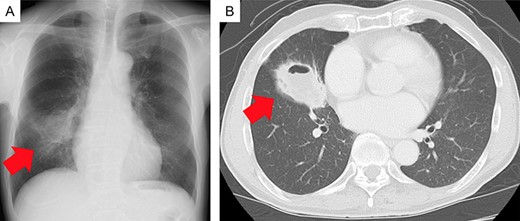
Imaging findings. (A) Chest radiograph showing an abnormal shadow in the right-middle lung field (red arrow). (B) Chest computed tomography scan showing a tumor with a cavity, ~55 mm in diameter, in the right-middle lobe (red arrow).
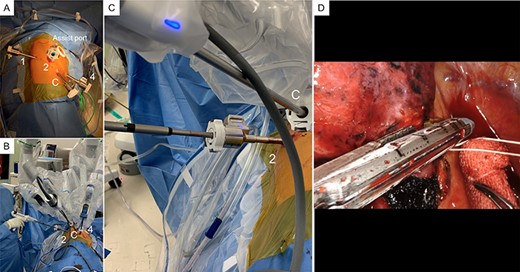
Robotic-assisted thoracoscopic surgery (RATS) findings. (A) A 4-cm utility thoracotomy performed at the fourth intercostal space (ICS) in the middle axillary line. Two 8-mm robotic trocars are inserted in the eighth ICS at the middle axillary line as a port for the robotic camera and the posterior side of the tip of the scapula as port 1, respectively. Two 12-mm robotic trocars were inserted in the seventh ICS anteriorly along the anterior axillary line as port 4 and in the seventh ICS along the posterior axillary line as port 2. The line marked as ‘1’ indicates port 1; ‘2’, port 2; ‘C’, the camera port; and ‘4’, port 4. (B, C) An assistant using a narrow-type vascular stapler (Signia small-diameter reload, Covidien Japan, Tokyo, Japan) through an 8-mm port with port 2. The pulmonary vein was divided using the narrow-type vascular stapler. (D) The pulmonary vessels were divided using the narrow-profile vascular stapler (Signia small-diameter reload) through the 8-mm port.
Under general anesthesia, the patient was intubated with a double-lumen endotracheal tube and placed in the left lateral decubitus position. A 4-arm RATS right-middle lobectomy was performed with a 4-cm utility thoracotomy, using da Vinci Xi (Intuitive Surgical, Sunnyvale, CA, USA). Utility thoracotomy was performed at the fourth intercostal space (ICS) in the middle axillary line, and an XS size wound retractor (Alexis wound retractor, Applied Medical, Rancho Santa Margarita, CA, USA) was placed. Moreover, two 8-mm robotic trocars were inserted in the eighth ICS at the middle axillary line as a port for the robotic camera and on the posterior side of the tip of the scapula as port 1, respectively. Two 12-mm robotic trocars were inserted in the seventh ICS anteriorly along the anterior axillary line as port 4 and in the seventh ICS along the posterior axillary line as port 2. After which, daVinci Xi (Intuitive Surgery) was docked (Fig. 2A). The pulmonary vessels were divided using the narrow-profile vascular stapler (Signia small-diameter reload) through the 8-mm port (Fig. 2B–D). The resected lung was removed through the utility thoracotomy. The postoperative course was uncomplicated. The final pathological stage was stage IB.
DISCUSSION
Owing to the national health insurance coverage of RATS for malignant lung and mediastinal tumors since 2018 in Japan, the number of domestic robotic surgical procedures performed has been increasing rapidly [1]. As RATS lung segmentectomy has been additionally covered by the national health insurance since 2020, it can be expected that the number of RATS surgical cases will increase further.
Although no problem would arise if the diagnosis is confirmed before surgery, thoracoscopic lung biopsy has been performed to diagnose uncertain lung nodules. VATS lobectomy performed after intraoperative pathological examination indicates that the specimen was from a malignant tumor. In Japan, VATS lobectomy may be switched to the RATS procedure in many hospitals in the future.
In Japan, as a fusion thoracic surgery, a method using the surgical instruments used in VATS during RATS, especially the endoscopic stapler, has been proposed. When RATS lung resection was performed after a thoracoscopic biopsy, the conventional endoscopic stapler could not pass through an 8-mm port, so it was changed to 8- to >10-mm ports. Although a robotic stapler is usually used, it is such a ‘mottainai’ that the endoscopic surgical stapler used during thoracoscopic biopsy was not utilized in the following RATS. Although a robotic stapler is easy to use, additional use of a robotic stapler after VATS lung biopsy is more expensive [2, 3]. In endoscopic surgery, various automatic linear staplers are used depending on the thickness, length and location of the vessels [4, 5]. We have preferred the Signia stapling system (Covidien Japan) for VATS lung resections. Previously, manipulation of a long-shaft stapler in thoracoscopic biopsy and RATS lung resection was reported [4]. Although a 12- or 15-mm port is required when using a conventional Signia stapling system (Covidien Japan), the narrow-profile vascular stapler (Signia small-diameter reload, Covidien Japan) can be used through an 8-mm port. The narrow-profile vascular stapler is designed to access tight spaces such as the pulmonary artery surrounded by tumor or swollen lymph nodes and is suitable for procedures using an 8-mm robotic port. Use of the Signia small-diameter reload (Covidien Japan) for open surgical procedures for pulmonary artery resection had no problems as compared with the conventional stapler. We have always thought it as a mottainai that the endoscopic surgical stapler used during thoracoscopic biopsy is not used in following RATS. By utilizing a narrow-profile vascular stapler, portal RATS could be performed using 8-mm ports after VATS lung biopsy. In addition, postoperative pain can be reduced by avoiding the use of a 12-mm robotic port.
ACKNOWLEDGMENTS
The authors would like to thank Enago (www.enago.jp/) for the English language review.
CONFLICT OF INTEREST STATEMENT
Masato Kanzaki has received honoraria from Intuitive Surgical Japan. All other authors declare no competing interests.
FUNDING
None.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
AVAILABILITY OF DATA AND MATERIALS
All the data and materials supporting our findings are included in the article.



