-
PDF
- Split View
-
Views
-
Cite
Cite
Rika Odajima, Soh Nishimoto, Kenichiro Kawai, Hisako Ishise, Masao Kakibuchi, A traumatic ulnar artery aneurysm in an infant, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab098, https://doi.org/10.1093/jscr/rjab098
Close - Share Icon Share
ABSTRACT
Ulnar artery aneurysm is very rare in infancy. Only a few reports have been done. We report an 8-month-old baby with true ulnar artery aneurysm on her hypothenar eminence. She had no specific past medical history, but an episode of falling. We resected the pulsating mass compressing the ulnar nerve, utilizing a surgical microscope. Reconstruction of the vascular deficit was not performed. She presented no functional deficit of the hand and no evidence of growth disturbance so far. As hypothenar eminence is a susceptible part for repetitive strikes, and as vein is fragile to the pressure, bypassing arterial route with vein graft is not recommended unless there is no other option.
INTRODUCTION
Acquired ulnar artery aneurysm is not a common condition, even though they are famous as hypothenar hammer syndrome. Symptoms caused by the pressure on the parallelly running ulnar nerve are frequently seen. Digital ischaemia may occur subsequently. Surgical treatment is the gold standard and vascular reconstruction with vein grafts are done often. In children, ulnar artery aneurysms are scarcely be seen. Here, we report a case of an infant with true ulnar artery aneurysm due to trauma. The aneurysm was resected without vascular reconstruction.
CASE REPORT
An 8-month-old infant was referred our department for a mass on her right hand. She had an episode of falling from her bed. Before that, parents did not realize any abnormality of her hand. A dull rise with thrill was observed on the hypothenar eminence. Tenderness and neuro-radiating pain was not evident, highly possibly because of her age. She did not present any other disorder. No bone fracture was observed. Ultrasonography revealed arterial blood flow inside. Contrast-enhanced magnetic resonance imaging (MRI) illustrated a bulge of artery in her hypothenar part (Fig. 1). An ulnar artery aneurysm was suspected. Blood route continuity from the radial artery to both deep and superficial palmar arches was confirmed.
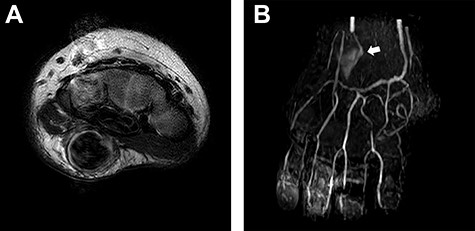
Presurgical images. (A) MRI revealed existence of a subcutaneous mass with the size of 9 x 9x 17 mm. (B) MR angiogram showed that the ulnar artery flow was reduced and deviated at the mass (white arrow). Continuity of the arterial network from the radial artery to the fingers was confirmed.
As the mass showed growing, a surgical exploration with an intension of excisional biopsy was planned. Reconstruction of the deficit was discussed. Blood flow to the fingers was estimated to be maintained even after the mass extirpation. Long-term complications from the replacement of the artery with vein graft were also discussed. Reconstruction was not planned pre-surgically.
Under general anaesthesia, air tourniquet was applied. After a zig-zag incision on her right hypothenar eminence, all procedures were done under a surgical microscope (Fig. 2). The mass appeared just beneath the skin. Meticulous dissection through the fascia was carried out and ulnar nerve was identified. Vessel loops were applied around the arterial branches to control. Proximal part of the artery to the mass was ligated and severed. Dissecting back side of the mass was carried out from proximal to distal. Both deep and superficial branches of the ulnar nerve were identified. Arterial branches distal to the mass were ligated and cut. At this moment, the tourniquet was released. Blood flow to the fingers and pulsation of the severed artery branches were reconfirmed. As preoperative planning, reconstruction of the arterial deficit was not done.
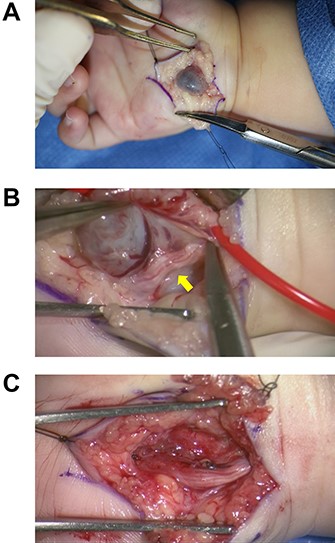
Surgical findings. (A) A subcutaneous mass was seen. (B) A vessel loop was put beneath the ulnar artery proximal to the mass. Adherence of the mass to the ulnar nerve (yellow arrow) was observed. (C) Soon after the resection of the mass. The ulnar nerve was preserved.
Histologically, it was diagnosed as a true aneurysm (Fig. 3).
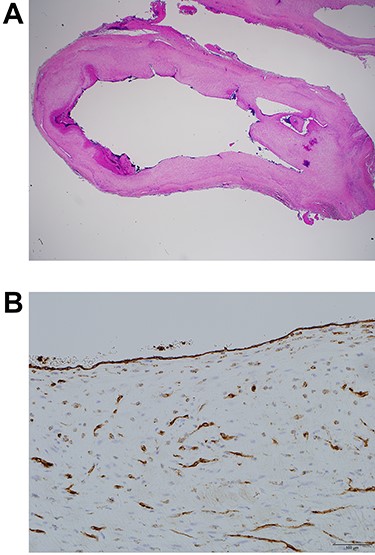
Histologically, it was diagnosed as a true aneurysm. (A) The aneurysm was sliced. Vascular lumen was maintained. All three layers of the arterial wall: tunica intima, media and adventitia were confirmed (Haematoxylin and eosin stain, 1.25x objective lens). (B) Lining of the lumen with endothelial cells was confirmed. Endothelial cells of vasa vasorum were also stained (CD31 stain, 20x objective lens).
Postoperative course of the patient was uneventful. At 9-months follow-up, she presented no functional deficit of the hand and no evidence of growth disturbance.
DISCUSSION
Although it is a famous occupationally acquired disease, known as hypothenar hammer syndrome, ulnar artery aneurysm in the hypothenar part is an unusual condition. The trauma, involving repetitive striking to the hypothenar eminence, during occupational or sports activities, is called to be the cause. It is a part of ulnar tunnel syndrome. Major symptoms are pain around the hypothenar eminence and paraesthesia of fingers as compression effect on the ulnar nerve, and cold intolerance as ischaemia effect with thrombosis. No many reports about paediatric cases have been done. Infantile cases are quite rare. There have been reports of congenital case operated at 1-year-old [1] and idiopathic one of 6-month-old [2]. The youngest traumatic case, found in our literature search, was a case of 6-month-old baby with a 2-months history of swelling [3]. In our presenting case, there was only one episode of falling, without bone fracture.
In paediatric cases usually, except when blood flow is not maintained due to vascular malformations, reconstruction has not been done [2, 4]. To reconstruct the blood route deficit, end-to-end anastomosis is the first choice, if applicable [5]. If not, interposition vein graft is usually used, considering the morbidity of harvesting arteries. A case in Pakistan, where preoperative evaluation of the palmar arterial arches was not possible, Y-shaped cephalic vein was used [3]. Great saphenous vein grafts had been the first choice for coronary artery bypass; though, long-term patency rate was inferior to internal thoracic artery graft [6], or to radial artery graft [7]. For ulnar artery reconstruction, patency rates of venous interposition grafts are not high (5 out of 14 in 43 months [8], 4 out of 18 in 118 months [9]) As there is no tunica-media, veins are vulnerable to the pressure. Veins will dilatate after arterial–venous shunting for haemodialysis. Lower leg vein will varicose when valve function fails. Hypothenar eminence is a susceptible part for repetitive strikes. There exists a report of a patient in 30s, with recurrent ulnar artery aneurysm after venous grafting [10]. Especially for young patients, placing vein at this part with high internal pressure is not recommended, unless there is no other option.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



