-
PDF
- Split View
-
Views
-
Cite
Cite
Ayaka Asakawa, Hironori Ishibashi, Masashi Kobayashi, Toshizumi Shirai, Kenichi Okubo, A rare case of thymoma with entire-tumor calcification, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjaa545, https://doi.org/10.1093/jscr/rjaa545
Close - Share Icon Share
ABSTRACT
A 49-year-old woman presented with cough, and chest X-rays showed an abnormal shadow. Chest computed tomography showed an anterior mediastinal 40-mm mass with massive calcification. The patient underwent mediastinal tumor excision performed using video-assisted thoracoscopic surgery. Pathological findings revealed the tumor to be a type B3 thymoma, with massive calcification occupying almost all of the thymoma. Due to high risk of recurrence, we performed completion thymectomy. Pathological findings revealed no remaining thymoma tissue in the residual thymus. Mediastinal tumor with entire calcification could be a candidate for surgical excision.
INTRODUCTION
Thymoma is the most common type of anterior mediastinal tumor. Calcification of thymoma sometimes occurs, but calcification rarely occupies the entire thymoma. Here, we report a rare case of thymoma with massive calcification.
CASE REPORT
A 49-year-old woman was admitted to the hospital presenting with a productive cough. The patient had no past medical history of note excluding a pneumothorax surgery in her twenties, and blood examinations were normal. Chest radiography showed an abnormal shadow in the anterior mediastinum (Fig. 1A), and chest computed tomography showed a 40-mm tumor with massive calcification in the anterior mediastinum (Fig. 1B and C). Magnetic resonance imaging (MRI) showed T1-weighted and T2-weighted heterogeneous signal intensities (Fig. 1D). Preoperative differential diagnoses were hamartoma, teratoma, calcified lymph node, hemangioma or thymic tumor with calcification. Excision of the tumor was performed using video-assisted thoracoscopic surgery, but intraoperative pathological diagnosis was difficult due to massive calcification and ossification. The tumor measured 40 × 40 mm with almost all parts showing calcification and ossification. Hematoxylin and eosin staining revealed calcification with focal round and oval cells and lymphocytes (Fig. 2A). An immunohistochemical analysis revealed that round and oval cells were positive for AE1/3, CAM 5.2 and negative for CD5 (Fig. 2C and D). The lymphocytes were CD3-positive immature T cells, and the tumor was diagnosed as type B3 thymoma.
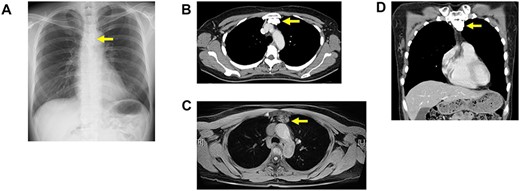
(A) Chest X-ray showing a calcification tumor in anterior mediastinum (arrow). (B) A chest computed tomography scan of horizontal section showing a 40-mm calcification tumor in anterior mediastinum. (C) A chest computed tomography scan of coronal section showing a 40-mm calcification tumor in anterior mediastinum. (D) MRI scan showing T1-weighted heterogeneous signal intensities.
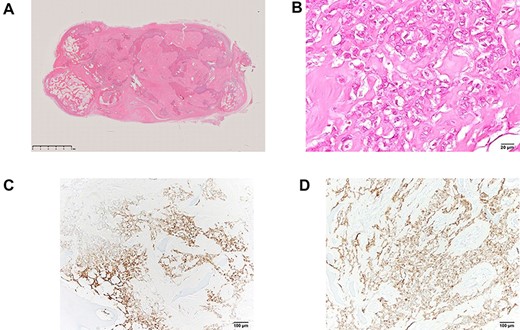
(A, B) Pathological finding revealed that mediastinal tumor was type B3 thymoma with massive calcification. (C, D) Immunological staining of the tumor showed positivity for AE1/3 (C) and CAM 5.2 (D). CD3-positive T-cells and CD5-positive T-cells were infiltrated around the tumor, whereas the tumor was negative for CD3 and CD5.
Due to risk of recurrence, the patient was then referred to our hospital. We performed completion thymectomy using video-assisted thoracoscopic surgery. Pathological findings revealed no residual thymoma in the resected thymus. There was no evidence of recurrence 2 years after the first surgery.
DISCUSSION
Calcification of thymoma can sometimes occur, with frequency ranging from 10 to 40%, especially in type B thymomas [1, 2]. Calcification of thymoma is associated with abnormal disposition of calcium salts, lipid metabolism and degenerative or necrotic tissues, as well as existence of other diseases, which cause dystrophic calcium or exposure of asbestos. Ossification, on the other hand, is related to the roles of osteoblasts and osteocytes and can indicate abnormal endocrine status, metabolism, genetics and growth factors [3]. Calcification shape patterns in thymoma can be classified as nodular, stippled and ringed [4, 5, 6]. In general, small nodular calcifications are common in thymoma, but entire-tumor calcification is rare and, to our knowledge, has never been reported previously. Nakada et al. [5] divided thymoma calcification into three types (inner, outer and miscellaneous) based on the area of calcification. In general, inner calcification is more common than outer calcification. In miscellaneous type, calcification arises from the calcification wall and is related to chronic inflammation. Regarding prognosis of thymoma with calcification, Harris et al. [7] concluded that thymic calcification did not seem to have diagnostic or prognostic value, but also stated that thymic calcification was more common in invasive thymoma than in non-invasive thymoma. Additionally, the incidence of intratumoral calcification in thymoma was not significantly different from that of thymic cancer. The use of thymic calcification or ossification for predicting prognosis of thymoma progression remains controversial. In the meantime, the recurrence of type B3 thymoma is higher than other types of thymoma. Weis et al. [8] reported that the 5-year recurrence rate of type B3 thymoma is 14%, whereas the recurrence rate of type A thymoma is 4%.
In our case, the patient had a tumor, which was almost completely occupied by calcification, with thymic epithelial tumor cells located around the calcification. Therefore, we speculate that the calcification had grown inside the thymoma. The patient had previously received pneumothorax surgery, so it was possible that local inflammation from surgery caused the calcification. Considering the high risk of thymoma recurrence, we performed completion thymectomy. Mediastinal tumor with entire calcification could be a candidate for surgical excision.
CONFLICT OF INTEREST
None declared.



