-
PDF
- Split View
-
Views
-
Cite
Cite
Maria Zarokosta, Aikaterini Foutsitzi, Iraklis Mpartziotas, Alexandros Manthas, John Tsiaoussis, Theodoros Mariolis-Sapsakos, Anomalous anatomic trajectory of the superior thyroid artery encountered during thyroidectomy. A rare case report, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab030, https://doi.org/10.1093/jscr/rjab030
Close - Share Icon Share
Abstract
Superior thyroid artery (STA), which is one of the primary arteries supplying to the thyroid gland, constitutes a severe consideration of both surgeons and interventional radiologists. Knowledge of the origin, the trajectory, the branching patterns and the anatomic aberrations of STA are of paramount clinical significance, due to its proximity to the external branch of the superior laryngeal nerve and the potentiality of accidental hemorrhage. The present manuscript reports for the first time the anomalous trajectory of the left STA, coursing superficially, through the left sternothyroid muscle and underlines the clinical significance of such aberrations.
INTRODUCTION
Superior thyroid artery (STA), which is one of the primary arteries supplying to the thyroid gland, constitutes a severe consideration of both surgeons and interventional radiologists [1, 2]. Indeed, the origin and the trajectory of STA are of paramount clinical significance when performing radiological interventions or head and neck surgeries due to its proximity to the external branch of the superior laryngeal nerve (ESLN) and the potentiality of accidental hemorrhage [1, 3]. In the literature, anatomical variances of the origin and the branching pattern of STA are highly reported [1, 2, 4, 6]. However, to our knowledge, the present manuscript describes for the first time an anomalous trajectory of STA crossing over the sternothyroid muscle.
CASE REPORT
A 53-year-old female proceeded to our institution with the diagnosis of benign multinodular goiter. The patient had been receiving T4 per os as medication for 4 years according to the endocrinologist’s instructions, but the size of the nodules had been increased significantly. Clinical examination detected tumescent palpable, movable nodules, without palpable cervical lymph nodes or hoarseness of voice. Blood tests, including T3, T4 and TSH were in the normal spectrum. Subsequent ultrasound of the thyroid gland revealed multiple nodules on both thyroid lobes. Following these, total thyroidectomy has been scheduled.
During the operation, surgeons gently retracted the skin and subcutaneous tissue overlying the platysma muscle. Both the platysma muscle and sternocleidomastoid muscles were exposed. As the dissection continued to the level of the muscles surrounding the hyoid bone, the left STA was incidentally detected coursing through the left sternothyroid muscle (Figs 1 and 2). Such an aberration is of major surgical significance, since posing a potential risk of accidental injury and bleeding. The left STA was meticulously ligated, and all the anatomical structures around right STA were gently dissected in detail. Careful dissection revealed that the origin of both STAs were the right and the left external carotid artery (ECA), respectively.
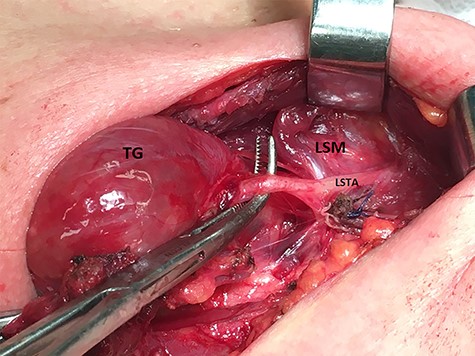
Meticulous exposure of the operative field. TG: thyroid gland, SM: sternothyroid muscle and LSTA: left superior thyroid artery.
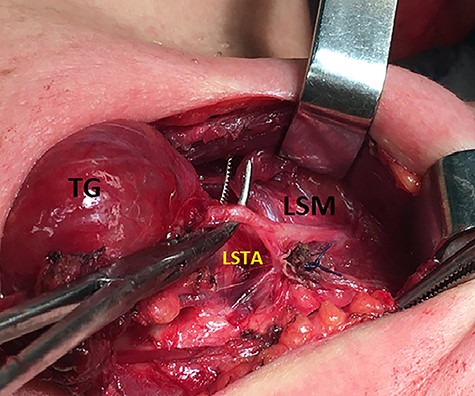
Meticulous exposure of the operative field. TG: thyroid gland, SM: sternothyroid muscle and LSTA: left superior thyroid artery.
The operation continued in the usual fashion. Finally, whole the anterior cervical region was meticulously investigated for possible hemorrhage or thyroid tissue remnants, and a drainage was placed. The operation was uneventful, and the drainage was removed the second postoperative day, when the patient was discharged. At the follow-up, the 10th postoperative day, the patient had no complication.
DISCUSSION
STA is one of the major arteries supplying to the thyroid gland, which typically originates from the ECA, below the greater cornu of the hyoid bone [1, 2, 6]. STA dispenses arterial branches to the neck region, including the overlying skin, the adjacent muscles and the upper larynx [2]. Herein, anatomical variations of STA are of paramount clinical significance when performing radiological interventions and head and neck surgeries [1, 3, 5].
Anatomical variances concerning the origin, thickness, course and branching patterns of the STA may differ among individuals [1, 2]. More specifically, it is reported that the typical origin of STA is the ECA with an incidence of 30–70% [6]. However, STA may also arise from the common carotid artery (CCA) and the common carotid bifurcation (CB) [1, 2, 4, 6].
Toni et al. [7] (2004) documented that STA arises with a greater incidence from ECA in Caucasian individuals in comparison to East Asians, whose STA more frequently originates from CCA. The embryology of these anatomic variances remains vague, and despite ethnic differences, individuals’ sex seems irrelevant to the origin of STA [2, 5–7].
Skandalakis [8] also reported double and unilateral STA. Moreover, although the average diameter of STA is 3.2 mm, it may vary between 1.5 and 4.5 mm and subsequently surgical maneuvers should be extremely gentle [5].
Referring to STA branching types, it is reported that STA typically parallels ESLN, coursing proximally to the thyroid gland and distributing five arterial twigs: (1) terminal arterial branches for the thyroid and the parathyroid glands, (2) the superior laryngeal, (3) infrahyoid, (4) sternocleidomastoid and (5) cricothyroid artery [3, 5]. Hu et al. [5] classified the probable branching types of STA into six categories, but still, adequate research must be done.
Besides, variations of the trajectory and branching patterns of STA, in addition to its relationship with adjacent anatomical structures seems being even more crucial to surgeons than the origin of STA [2]. Given the seriousness of uncontrolled hemorrhage in surgery, or ESLN palsy, thorough knowledge of STA variances is fundamental [1, 2, 5]. Therefore, the present manuscript describes for the first time, anomalous superficial course of left STA, through the left sternothyroid muscle.
Both surgical and invasive radiological maneuvers request an excellent knowledge of the STA topographical anatomy and its variations. Ignorance of such anatomical variances may lead to serious complications when performing radiological interventions or head and neck operations, such as the surgical treatment of metastatic cancer to the neck, aneurysms and congenital wastes, thyroidectomy, microcatheterization, and tracheotomy that may lead to hemorrhage, which is related to serious morbidity and mortality [1, 2, 5].
Finally, since preoperative observation of STA anatomical variations is not feasible without CT angiography, the fundamentals to avoid accidental injury are: (a) adequate exposure of the trajectory and the origin of STA, since it is quite evident that probable novel anatomic variations could be unexpectedly detected during surgery, (b) avoidance of STA ligation out of the pretrachial fascia in order to minimize the risk of ESLN injury [5] and (c) meticulous hemostasis.
Conclusively, since even an anatomic variance of minor degree may affect the outcome of such procedures, surgeons’ and interventional radiologists’ deep anatomical knowledge remains the cornerstone for safe therapeutic outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



