-
PDF
- Split View
-
Views
-
Cite
Cite
Piotr Sumislawski, Carolin Ludwig, Roman Rotermund, Ulrich Grzyska, Jörg Flitsch, Internal carotid artery false aneurysm as a fatal complication of transsphenoidal surgery, Journal of Surgical Case Reports, Volume 2021, Issue 4, April 2021, rjab146, https://doi.org/10.1093/jscr/rjab146
Close - Share Icon Share
Abstract
False aneurysm of internal carotid artery (ICA) is a rare but serious vascular complication observed after transsphenoidal pituitary surgery. Here, we present a 41-year-old woman with a pseudoaneurysm in the ophthalmic1 segment of the left ICA after exoscopic transsphenoidal pituitary surgery. The initially uneventful procedure was complicated by a subarachnoidal hemorrhage 10 days after the surgery, which was confirmed by cranial computed tomography scan. The emergency angiography revealed a pseudoaneurysm of the ophthalmic1 part of the left ICA. Despite repeated endovascular treatments with a flow diverter and coiling, the patient experienced a re-bleeding with consecutive vasospasms, occlusion hydrocephalus and finally bifrontal intracerebral hemorrhage with fatal outcome. As a conclusion in irregular post-operative courses with for example headache, a post-operative magnetic resonance imaging with vessel presentation using TOF sequence and contrast-enhanced MRA might be recommended in order to detect a possible pseudoaneurysm in an early stage.
INTRODUCTION
Intracranial false aneurysms account for around 1% of all intracranial aneurysms and are associated with high mortality (up to 50%). The common causes are trauma, infectious diseases, irradiation, iatrogenic injuries, collagen vascular diseases or rupture of true aneurysm [1]. Iatrogenic injuries can be a complication of different surgical procedures, including ventriculoperitoneal shunt insertion [2], endoscopic third ventriculostomy [3], endonasal sinus [4] or transsphenoidal surgery [5]. The reported incidence of false aneurysms after transsphenoidal surgery varies between 0.2 and 2% [6]. The most common affected vessel is not only the internal carotid artery (ICA) within the cavernous but also the ophthalmic (Bouthillier-classification), supraclinoid (Gibo-classification) and C2 (Fisher-classification) segment [7, 8]. The reported therapy options comprise of microsurgery, endovascular, combination of both techniques or conservative treatment. Endovascular techniques include coiling, stent protected coiling, covered stents and pipeline devices [6, 9] or at least ICA sacrification (coil occlusion). Early diagnosis and treatment of potentially life-threatening complications from ruptured aneurysm, such as subarachnoid hemorrhage, vasospasms or hydrocephalus, have a great impact on the outcome [10, 11].
CASE REPORT
A 41-year-old woman presented with recurring Cushing’s disease for renewed resection of the pituitary adenoma (Fig. 1a). The intraoperative and initial post-operative course was uneventful. The patient remained neurological intact without any signs of liquorrhea, headaches, nausea or emesis. Laboratory testing showed a drop of ACTH and cortisol and no signs of pituitary insufficiency, diabetes insipidus or SIADH. The patient was discharged after 4 days.
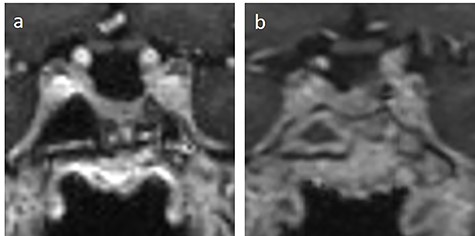
(a) preoperative and (b) post-operative MRI T1-weighted coronal image with contrast medium of the sella.
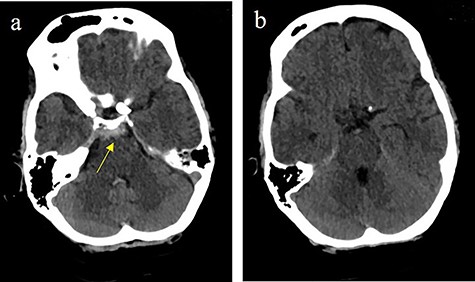
Subarachnoidal bleeding into the basal cistern-axial cranial computed tomography (cCT) at the level of (a) prepontine cistern (arrow) and (b) pentagonal cistern.
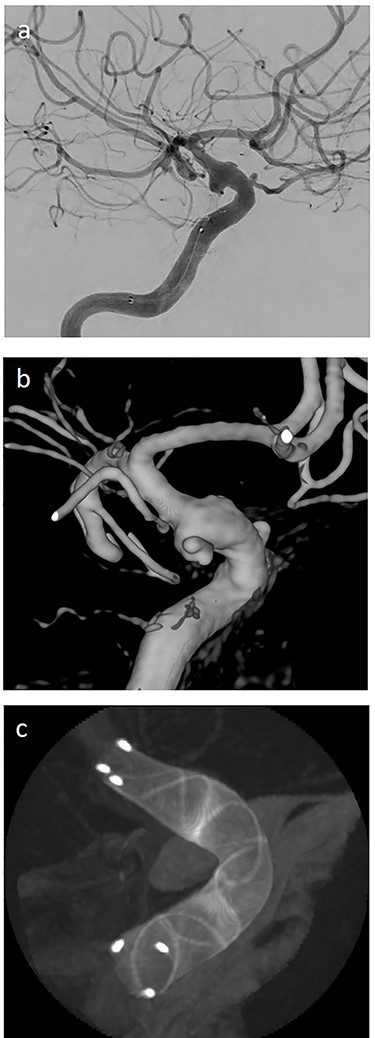
(a) lateral angiogram of left carotid artery showing an ICA aneurysm; (b) 3D reconstruction of the pseudoaneurysm with (c) flow diverter (Derivo®—4,5/20) reconstruction.
On post-operative Day 5, the patient presented to the emergency room with severe headaches VAS 8/10, neck stiffness and photosensitivity and she was re-admitted to our department. Initially, a meningitis was suspected without rhinoliquorrhea on examination, and a lumbar puncture was performed. The cerebrospinal fluid (CSF) examination revealed pleocytosis and hypoglycorrhachia, therefore an empirical intravenous antibiotic therapy was started. The patient showed clinical improvement with reduction of headaches, photophobia and stiff neck. On Day 8 after surgery, there was no sign of growth in the CSF culture. Antibiotic therapy was terminated. A magnetic resonance imaging (MRI) of the sella was performed and revealed normal post-operative finding. (Fig. 1b).
On the next day (Day 9 post-op), the patient suffered from acute and devastating headaches, with screaming and enuresis. An emergency computed tomography (CT) was carried out and displayed a prepontine and retroclival subarachnoid hemorrhage (Hunt & Hess Grade I), (Fig. 2). For further evaluation, a digital subtraction angiography (DSA) was conducted, and it showed a pseudoaneurysm of ophthalmic1/supraclinoid2/C23 part of the left ICA, which was directly treated by a flow diverter (Derivo®—4,5/20), with remaining rest flow (Fig. 3). The patient was transferred to the ICU, transcranial doppler sonography was performed and revealed normal flow. In the following course, the patient suffered from Terson’s syndrome and hyponatremia due to SIADH, but after clinical improvement, was transferred back to normal station after 10 days of post-operative monitoring. Furthermore, the patient was plagued with cephalgia and nausea, which could not be compensated with analgetics and antiemetics. On the 20th post-operative day after the epileptic seizure with postictal vigilance reduction, an emergency CTA was conducted showing progressive SAH (Fig. 4) and a growing pseudoaneurysm as well as generalized vasospasm with posthemorrhagic hydrocephalus. For an emergency CSF diversion, an external ventricle drain was placed. The repeated DSA showed a growing false aneurysm which was treated with two additional flow diverters (2× Derivo®—4,5/20) as well as coiling (HydroSoft™ 2/3 and 2× 1,5/2) by endoleak (Fig. 5). The vasospasms were treated by an intraarterial spasmolysis (Fig. 6).
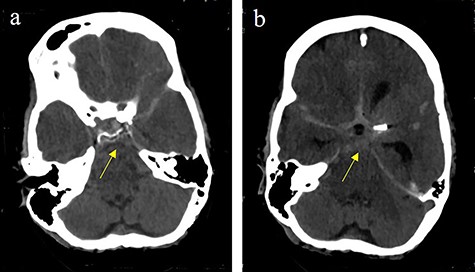
Massive progress of SAH axial cCT at the level of (a) prepontine cistern (arrow) and (b) pentagonal cistern (arrow)
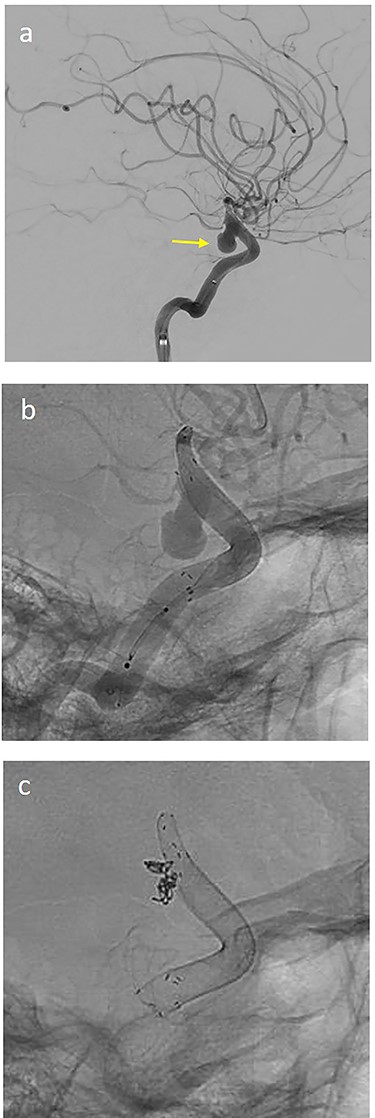
(a) lateral angiogram of left carotid artery showing ICA aneurysm before the second endovascular treatment; (b) Lateral view after implantation of two additional flow diverters (2× Derivo®—4,5/20); (c) Lateral view after additional coil embolization (HydroSoft™ 2/3 and 2× 1,5/2).
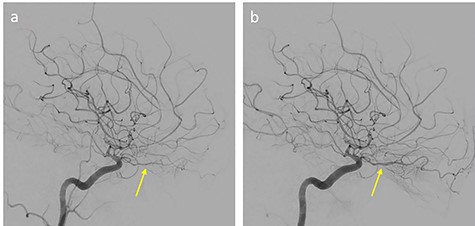
Anteroposterior left carotid artery angiograms; (a) during vasospasm (arrow) and (b) after intraarterial 2 mg nimodipin administration (arrow)
The patient was transferred to the ICU. During the next days, there was no clinical improvement of vasospasms despite daily intraarterial spasmolysis. EEG showed moderate–to-high epileptic activity. A wake-up attempt was not successful. Because of epileptic seizures despite anticonvulsive treatment, sedation therapy needed to be continued. Transcranial doppler ultrasound showed further the signs of vasospasm, but the patient showed spontaneous eye opening with untargeted movements of her upper right extremity after 11 days from ICU takeover.
During the next days, the clinical status was stable. On the 43th post-operative day, the clinical situation worsened by an epileptic state with development of maximally dilated pupils without light reaction. CT revealed a massive bifrontal bleeding with rupture into the ventricles and brain herniation (Fig. 7). On the 44th post-operative day, brain death was diagnosed.
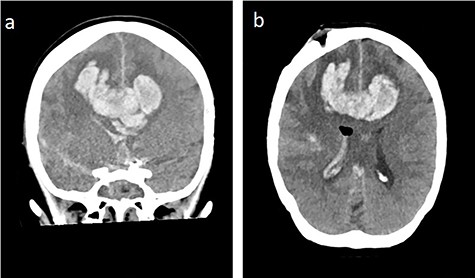
Bifrontal intracerebral bleeding with brain swelling and herniation: (a) coronal cCT, (b) axial cCT
DISCUSSION
The development of a pseudoaneurysm is a rare but serious vascular complication after transsphenoidal pituitary surgery [12]. There are several risk factors described in the literature, such as previous surgery, radiation, or treatment with dopamin agonists, as well as cavernous sinus invasion and carotid anomalies [12]. In the presented case, the aneurysm is located at the inherent artery but distant to the surgical field outside the cavernous sinus. Additionally, factors such as organization of subarachnoidal space, it’s texture and other properties, which stabilize the position and support the walls of arteries may play a huge role in predisposition to aneurysm formation and consecutive subarachnoidal bleeding [13]. The direct pathomechanism remains unclear. At our case report, at least iatrogen involvement is suggested. The treatment of a false aneurysm remains a great challenge. Different therapeutic approaches have been reported, including a conservative strategy, surgical (clipping, wrapping and trapping with bypass) and endovascular treatments (balloon occlusion, coil embolization or flow diversion) [6, 9]. The surgical approach seems to be associated with higher risks of complication and morbidity [12]. The endovascular treatment has been described as effective and less invasive, therefore its` usage expanded over the last years [9]. Especially, flow diverters revealed similar effectiveness to other endovascular methods with a lower complication profile [14, 15], but they require long-term inhibition of thrombocyte aggregation.
CONCLUSION
Our case report shows that even proper management of a false aneurysm according to common standards may result in fatal outcome. We therefore postulate that the problem of pseudoaneurysm management requires interdisciplinary and multicentric analysis of a larger number of cases regarding diagnostic and therapeutic options. Moreover, from our point of view, for patients with strong post-operative headaches and nausea, we would recommend a post-operative MRI with vessel presentation using as a first-line diagnostic tool TOF sequence and contrast-enhanced MRA, which additionally can be used to assess the extent of resection.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- angiogram
- pseudoaneurysm
- magnetic resonance imaging
- computed tomography
- hemorrhage
- magnetic resonance angiography
- cerebral hemorrhage
- hydrocephalus
- false aneurysm
- headache
- internal carotid artery
- fatal outcome
- cranium
- subarachnoid space
- surgical procedures, operative
- eye
- pituitary gland surgery
- vascular complications
- endovascular procedures
- fluid flow



