-
PDF
- Split View
-
Views
-
Cite
Cite
William D Parker, Keith Jones, Burkitt’s lymphoma: an unexpected cause of dental pain, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa557, https://doi.org/10.1093/jscr/rjaa557
Close - Share Icon Share
Abstract
We would like to describe a case of Burkitt’s lymphoma in a 37-year-old lady, who initially presented to her General Dental Practitioner (GDP) complaining of pain and episodic numbness in the right lip and chin. The initial diagnosis was irreversible pulpitis of the lower right second molar (LR7) and despite having an extraction of the affected tooth her problems persisted. The patient also developed pain in the spine and limbs, accompanied by lethargy and weakness.
After seeing multiple different practitioners, she was referred to her local Oral and Maxillofacial Surgery department. Cross-sectional imaging was requested and demonstrated disseminated malignancy. Histology following open trans-oral biopsy revealed a diagnosis of Burkitt’s lymphoma prompting an urgent haematology referral, and she successfully completed a chemotherapy regimen. This case highlights the importance of a thorough diagnostic process in the presence of persistent and/or atypical symptoms.
INTRODUCTION
Burkitt’s lymphoma is a highly aggressive non-Hodgkin B-cell lymphoma, considered as the one of the fastest growing human tumours. Burkitt’s is divided into three subtypes: endemic, sporadic and immunodeficiency associated. In countries where malaria is endemic, especially equatorial Africa, it is commonly associated with Epstein–Barr virus (EBV) infection. Elsewhere, it usually develops sporadically with no identifiable trigger. Sporadic Burkitt’s usually originates as a rapidly enlarging mass in the abdomen. EBV-related Burkitt’s commonly presents in the jaw and kidney, whereas jaw involvement in sporadic and immunodeficiency-associated Burkitt’s is much less common [1].
Dental and associated mandibular pain is a very common presentation in the general population. The pain is most commonly odontogenic in origin and is caused by pulpitis of the tooth [2]. It is rare for conditions such as pulpitis, or even apical pathology of the tooth, to directly cause impaired sensation of inferior alveolar or mental nerves, and thus cause perioral numbness [3].
This case explores the diagnostic and therapeutic process of a relatively young patient who presented with dental and jaw pain and concurrent paraesthesia. Initially, no cause other than of dental origin was investigated. The patient was treated for dental infection repeatedly before the diagnosis of Burkitt’s lymphoma was eventually established.
CASE PRESENTATION
A 37-year-old fit and well lady presented to her General Dental Practitioner (GDP) complaining of pain in the right side of her mandible and episodic numbness in the ipsilateral mental nerve distribution. An orthopantomogram (OPG) (Fig. 1) was taken, with the GDP contentiously identifying an area of increased radiolucency at the apex of the right lower second molar. The patient was referred to a specialist dentist for root canal treatment of the tooth, with the GDP suspecting irreversible pulpitis.
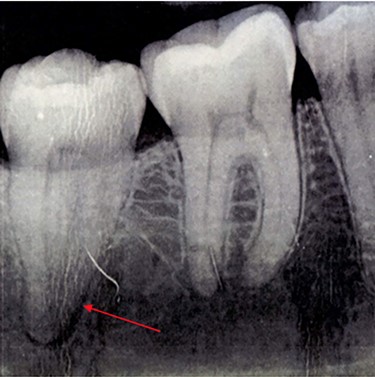
OPG taken on patient’s first visit to GDP. Demonstrates radiolucency at apex of LR7.
The pain began to radiate along the jaw to the right ear and the numbness became more frequent. Soon, the symptoms became intolerable and extraction of the tooth was performed instead. Significant bleeding was noted during the procedure. The jaw pain eased for several days, before returning as aforementioned. This prompted several returns to the GDP, who reassured the patient, attributing the return of symptoms to lack of bone regrowth and subsequently granuloma formation in the extraction site. The adjacent tooth on the lower right side was noted to have low-grade mobility and antibiotics were prescribed in case of infection.
‘Excruciating’ pains throughout the thoracic spine and rest of the body developed over the next month, and the patient had experienced unusual heavy menstrual bleeding. The patient had routine blood tests that revealed low platelets (120 × 109/L) and vitamin D (25 nmol/L), otherwise bloods were unremarkable. Her GP made a referral to the rheumatologist due to her non-specific myalgia and arthralgia.
The patient’s swelling and pain intensified, while her generalized lethargy and weakness became debilitating. Palpable, painless ‘lumps’ began to appear on her scalp and the patient organized a Maxillofacial Surgery (OMFS) appointment through a private dentist. In the meantime, the rheumatologist had seen the patient and attributed her symptoms to an underlying jaw infection.
At her OMFS appointment, the consultant was concerned by the abnormal appearance of the extraction site intraorally, combined with the evolving systemic symptoms (Figs 2–4). Urgent magnetic resonance imaging (MRI) head and neck (Figs 5 and 6) and computerized topography (CT) mandible scans were requested and completed in an extremely short time frame.

Photo taken on admission to RDH illustrating right-sided submandibular swelling.

(A) and (B) Photos showing the site of Burkitt’s tumour infiltrating the oral mucosa and extraction site of LR7 prior to incisional biopsies taken by the OMFS team.

OPG taken on admission to RDH. Note: LR7 has been extracted and there is a patch of radiolucency inferior to LR7/8.
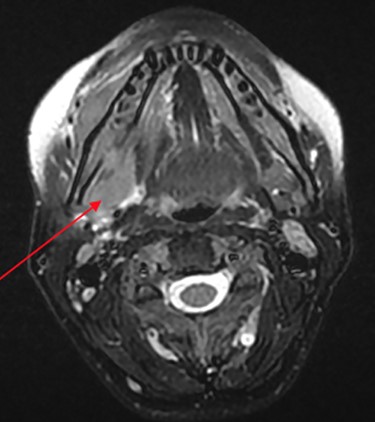
MRI head (axial view) showing Burkitt’s infiltrating the mandible and oral mucosa.
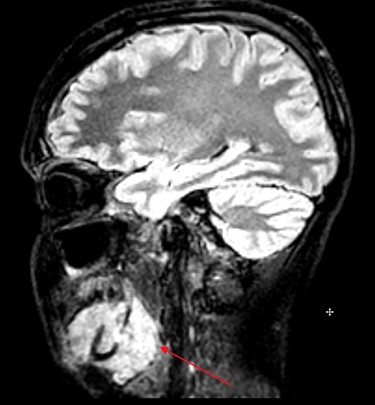
MRI head (sagittal view) showing Burkitt’s infiltrating the mandible and oral mucosa.
On the way to this scan, the patient experienced unilateral foot drop and was unable to walk. The scans revealed multifocal neoplastic deposits throughout the jaw, skull base, cervical spine and thyroid. These results, along with suspected malignant spinal cord compression (MSCC), prompted immediate admission to the head and neck ward at Royal Derby Hospital (RDH).
An MRI spine ruled out MSCC. A CT chest, abdomen and pelvis showed disseminated neoplasms involving the liver, peritoneum and pelvic adnexa. Incisional biopsies of the mandible and the adjacent buccal swelling were performed under general anaesthetic by the OMFS team. These revealed high-grade B cell lymphoma. Further analysis of the sample demonstrated the tumour cells were positive for CD20, CD10 and BCL6 markers, while almost 100% of cells were Ki-67 positive, revealing a definitive diagnosis of Burkitt’s lymphoma [4].
An aggressive chemotherapy regime called R-Codox-M/R-VAC, consisting of eight cytotoxic agents, was initiated immediately afterwards. This is the gold-standard treatment. It is given both intravenously and intrathecally, virtually eliminating the body’s entire marrow, leaving the patient severely pancytopenic and requiring specialist care in the haematology ward. Yet, with five-year survival of approximately 80–90%, it proves to be a highly effective treatment [5]. The patient has successfully completed the regime and is currently in remission.
DISCUSSION
Burkitt’s lymphoma constitutes for approximately 2% of non-Hodgkins lymphoma (NHL) in the UK each year with around 200 cases, mostly affecting children [6]. The low prevalence of Burkitt’s in the UK combined with the rarity of Burkitt’s presentation in the oral cavity and the young age of the patient makes the diagnosis of Burkitt’s totally unexpected [7].
When the mandible has been infiltrated by Burkitt’s tumour, dental pain and perioral numbness are the most commonly reported symptoms [8]. These symptoms have been attributed to ondontogenic infection where Burkitt’s has been the underlying pathology previously in the literature [9]. However, since atypical symptoms such as ipsilateral perioral numbness were present and persisted following prolonged treatment, head and neck malignancy must be ruled out.
Pulpitis and subsequent apical periodontitis are commonly caused by tooth decay, a result of poor dental hygiene. The patient reported having very few dental issues in the past, and moreover, the evolving symptoms were not in keeping with the usual disease progression of pulpitis. Such marked involvement of the mental and inferior alveolar nerves and continuation of symptoms post-tooth extraction indicated a high likelihood of alternative pathology. Infection-induced paraesthesia generally subsides once inflammation and infection are removed following antibiotic therapy or tooth extraction [10]. Both medical and dental professionals continued to treat the patient for benign odontogenic pathology without consideration of malignancy, and this delay in the correct diagnosis and treatment led to significant patient morbidity and almost mortality.
SUMMARY
This case has demonstrated that ipsilateral perioral numbness, and red flag symptoms in general, needs to be identified in the primary care setting and specialist referral made, where the necessary investigations such as MRI can be carried out. The threshold for making these referrals is diminished even further when initial treatments prove ineffective. Failure to rule out sinister pathologies, such as head and neck cancer, in these patients can ultimately prove fatal. Fortunately, once Burkitt’s is diagnosed, it can be effectively treated in the vast majority of patients.
ACKNOWLEDGEMENTS
I would like to thank the subject of this case report of her family for their time and permission to write this case report. I would also like to thank members of the maxillofacial and haematology departments at Royal Derby Hospital for providing me with insight and guidance in writing this case report.
CONFLICT OF INTEREST STATEMENT
None declared.



