-
PDF
- Split View
-
Views
-
Cite
Cite
Aghyad Kudra Danial, Abdulqader Klaho, Abdulaziz Abou Redn, Zeina Al-Najjari, Joudi Tarabishi, Sara Chabarek, Ahmad Sankari Tarabishi, Ahmad Alhaj, A rare case of peritoneal Xanthogranuloma in a 23-year-old woman, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjaa533, https://doi.org/10.1093/jscr/rjaa533
Close - Share Icon Share
Abstract
Xanthogranuloma is a very rare tumor when it comes to abdomen. Macroscopically, it is characterized by formation of multiple, golden yellow or bright yellow nodules, whereas histologically, the lesion is predominantly composed of foamy cells mixed with acute and chronic inflammatory cells. We report a case of 23-year-old woman presented to the hospital with chronic constipation, colic abdominal pain and recurrent vomiting. The patient had a history of sigmoid colon volvulus. Radiological investigations showed sigmoid colon elongation, multi-density formations in the left iliac region and pelvis and a small amount of pelvic fluid. Laparoscopy followed by excisional biopsy of the formations were made, and pathological examination showed Xanthogranuloma with no ovarian parenchyma. Hence, Xanthogranuloma should be considered as a differential diagnosis for idiopathic abdominal pain. Laparoscopy and excisional biopsy are suggested procedures when short-term therapy is concerned.
INTRODUCTION
Xanthogranuloma is a very rare tumor when it comes to abdomen, and it was first described by Oberling in 1935 [1].
Macroscopically, it is characterized by formation of multiple golden yellow or bright yellow nodules; histologically, it is predominantly composed of foamy histocytes mixed with acute and chronic inflammatory cells [1].
We report in this case, a patient who presented with recurrent colic abdominal pain, accompanied by vomiting of unknown origin. The patient was diagnosed with intraperitoneal Xanthogranuloma through several diagnostic procedures and recovered after laparoscopic excisional biopsy of xanthogranulomatous formations.
CASE REPORT
A 23-year-old woman presented to hospital complaining of chronic constipation that had started 2 month earlier. It was accompanied by colic abdominal pain and recurrent vomiting. Her general condition, appetite, urination, sleep and vital signs were all normal. As a history, she was admitted in a hospital previously with bowel obstruction due to sigmoid colon volvulus, but she was discharged after 2 days without any intervention. On physical examination, there was hypogastric pain without tenderness and visceral movements were slightly increased in the hypogastric and periumbilical regions. On radiology investigations, chest X-ray and echography of abdomen were all normal. CT scan showed multi-density formations in the left iliac region with a small amount of pelvic fluid (Fig. 1). The Barium Enema showed sigmoid colon elongation, without filling defects.
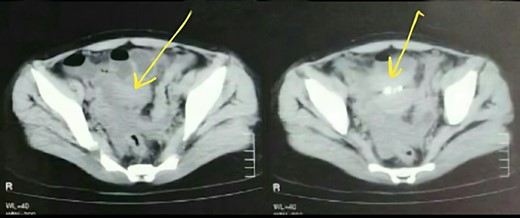
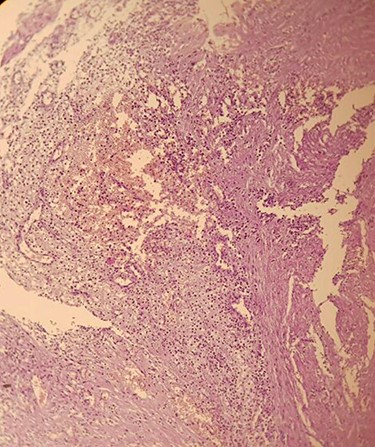
We performed exploratory laparoscopy and found a mass measured (2 × 3 cm) on the left pelvic between the bladder and the uterus, adjacent to the left ovary. A 100-ml serous fluid was found in the pelvis and was aspirated. Furthermore, we noticed formations on the left iliac region adjacent to the parietal peritoneum. We resected the mass and the other formations and sent them to pathology that revealed an aggregation of lipid laden macrophages (foamy cells) (Fig. 2) that is infiltrated by lymphocytes and neutrophils and blood vessels congestion (Fig. 3). These findings suggested Peritoneal Xanthogranuloma with massive necrosis and no ovarian parenchyma. The aspirated fluid was bloody and inflammatory with no signs of malignancy.
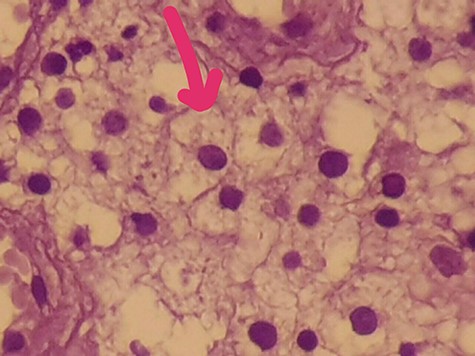
Aggregation of lipid laden macrophages (foamy cells) that is infiltrated by lymphocyte and neutrophils with blood vessels congestion.
After 10 days of surgery, the patient had a good general condition with no complications. Two months later, Abdominal and pelvic ultrasound showed no abnormalities and no fluids were noticed.
DISCUSSION
Xanthogranuloma is a very rare tumor that makes up an extremely small fraction of intra-abdominal tumors. It was first described by Oberling in 1935 [1]. Macroscopically, it is characterized by the formation of multiple golden yellow or bright yellow nodules, whereas microscopically, the lesion is predominantly composed of foamy cells mixed with acute and chronic inflammatory cells [1, 2].
The presence of necrosis as it was described in our case is unusual in such cases. The pathogenesis is vague so far but some related mechanisms are suggested such as defective lipid transport, immunologic disorders, recurrent infection and adjacent obstruction of lymphatic drainage [2].
Xanthogranuloma has been reported to occur in the endometrium, ovary, fallopian tubes, vagina, testis epididymis, stomach, bone, urinary bladder, thyroid and adrenal glands. Nevertheless, gallbladder and kidney recorded the highest occurrence rates [2].
In some cases, retroperitoneal lesions could cause compression of renal arteries, ureters and other retroperitoneal organs.
Usually, Xanthogranuloma in size (2 × 3 cm) is unlikely to be discovered due to the absence of probable compressional symptoms. In similar cases, the tumor caused early symptoms due to urinary tract involvement [3]. However, in our case, the tumor adhered to an intestinal loop; therefore, there was an incomplete intestinal obstruction causing remittent symptoms and a moderate pain.
When it comes to treatment, many therapeutic options were performed based on the numerous conditions in the cases. Many similar cases have been treated with surgical excision, sometimes followed by adjuvant radiotherapy or chemotherapy [4], and steroids have also been used [5]. In our case, excisional biopsy through laparoscopy was successfully performed due to the small size of the tumor.
In other cases, the tumor resolved spontaneously. However, despite having and applying different therapeutic procedures, relapse was always possible to occur. Nevertheless, surgical excision appears to be the best therapeutic option in such cases because it can at least delay the complications related to local spread of Xanthogranuloma. Therefore, when having a localized tumor in an accessible site, we can follow the previous option with the minimal possibility of relapse. The unusual localization of Xanthogranuloma in the abdominal cavity should be taken into consideration. Diagnostic tools are still limited to discover and diagnose Xanthogranuloma due to the lack of specific clinical manifestations. For the short-term therapy, laparoscopy and excisional biopsy are sufficient procedures for treating small sizes of Xanthogranuloma like the one in our case.



