-
PDF
- Split View
-
Views
-
Cite
Cite
Wendy Pamart, Bernard Majerus, Unusual complication after laparoscopic Nissen fundoplication, Journal of Surgical Case Reports, Volume 2021, Issue 2, February 2021, rjab023, https://doi.org/10.1093/jscr/rjab023
Close - Share Icon Share
Abstract
We describe a rare complication of Laparoscopic Nissen Fundoplication in the presence of a Gastric greater curvature Plication (LNFGP). An overweight 64-year-old woman was admitted for severe abdominal pain, dysphagia and fever 2 weeks after a Nissen fundoplication. She had pneumoperitoneum on scanner. At laparoscopy, we found a generalized peritonitis secondary to a perforated Nissen wrap in the presence of a gastric greater curvature plication. Gastric bypass and sleeve gastrectomy can be irrelevant in case of moderately and severely obese patients with gastroesophageal reflux disease. Four studies have investigated the risks and rewards of the LNFGP as an alternative. Only one case of leakage has been reported. We present another severe complication: the pylorus stenosis caused by a plication performed too close to the pylorus, causing gastric dilatation in the presence of the wrap, leading to wrap perforation.
INTRODUCTION
Roux-en-Y gastric bypass and sleeve gastrectomy are the most common bariatric procedures. In case of gastroesophageal reflux disease (GERD) in obese patients, no established procedure exists. We present a case of near-lethal complication after Nissen fundoplication for GERD.
CASE REPORT
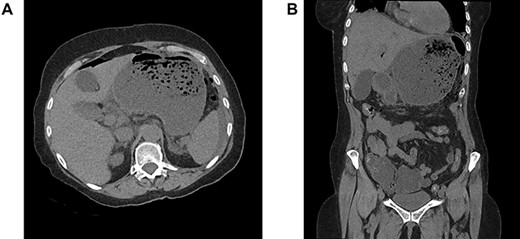
A 64-year-old woman was admitted in emergency for severe abdominal superior pain, nausea, dysphagia and fever. She explained having undergone a Nissen fundoplication 2 weeks earlier at another hospital, complicated a few days later by persistent dysphagia leading to redo-laparoscopy. Past medical history included hypertension, chronic obstructive pulmonary disease, hypothyroidism and appendectomy. On physical examination, she was septic (38.2°C, 110/70 mmHg, 110 bpm) with diffuse abdominal guarding. The blood test revealed a high grade of inflammation (C-reactive protein 17.35 mg/dL, white blood count 20.9 1000/mm3, lactic acid 3.2 mmol/L). The computed tomography scanner showed signs of perforation with hugely dilated stomach (Fig. 1A and B). Laparoscopic exploration attested to a generalized purulent peritonitis. Surprisingly, we found also a gastric greater curvature plication leading to a pyloric obstruction (Fig. 2A and B). Dismantling the Nissen wrap and the gastric plication allowed to find the gastric perforation on the top of the wrap (Fig. 3A and B). Simple closure of the perforation and large peritoneal lavage were performed. Postoperative recovery was marked by a left subphrenic abscess resolved under antibiotherapy. The patient was discharged on postoperative day (POD) 22.
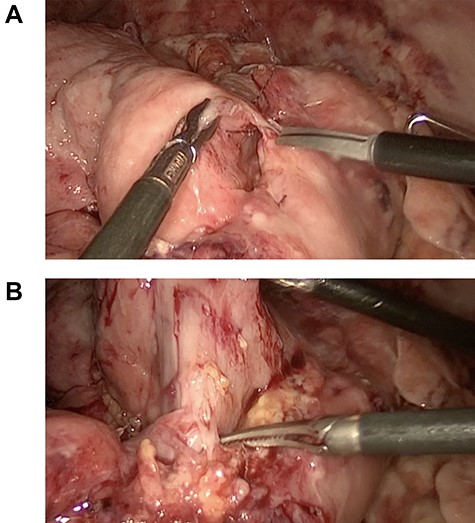
(A) gastric greater curvature plication, (B) pylorus obstruction.
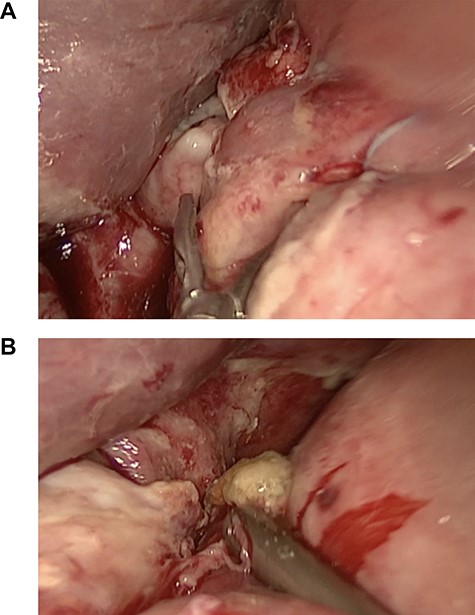
(A) Nissen wrap, (B) gastric perforation on the top of the wrap.
Medical record from the previous hospital mentioned a Nissen fundoplication for chronic GERD and a gastric plication for overweight and patient’s desire to lose weight. Redo-laparoscopy was performed on POD 16 because of dysphagia on narrow esophagogastroduodenal conduit and consisted of the section of the first point of the wrap.
DISCUSSION
Laparoscopic Nissen fundoplication (LFN) combined with Gastric greater curvature Plication (LNFGP) is not a common procedure. In the literature, it has been investigated by four studies. In total, 173 patients were enrolled and 115 underwent the LNFGP procedure (18 patients [1], 56 patients compared with 58 patients operated from LNF [2], 25 patients [3] and 16 patients [4]). The inclusion criteria were broadly the same: age between 18 and 62 years, moderate obesity [body mass index (BMI): 30 to 39 kg/m2] and history of GERD. The exclusion criteria were also similar: previous gastric surgery, cardiovascular risk factors and uncontrolled diabetes mellitus. The aim of this procedure was to provide an attractive and safe management of GERD in moderate and severe obesity. Roux-en-Y gastric bypass is the gold standard for bariatric patients suffering from GERD but due to its potential long-term consequences, it could be irrelevant in moderate and severe obesity. Preoperative GERD contraindicates sleeve gastrectomy. Gastric greater curvature plication alone increases gastric pressure and subsequent reflux [2]. The main outcomes of the mentioned studies were weight loss and cure of GERD. Regarding weight loss, included obese patients had BMI over 30 [1, 2] and 32 kg/m2 [3, 4]. Mean excess weight loss reported was of 45% [2], 46% [3], 48% [1] and 58% [4]. Compared to Roux-en-Y gastric bypass with an excess weight loss (EWL) reaching 70% 1 year after surgery [5], LNFGP is less efficient. Regarding cure of GERD, Ospanov reported that acid exposure was significantly decreased after LNFGP but found no difference either in acid exposure in the esophagus or for GERD-HRQL mean score within the group LNF and LNFGP [2]. The authors defend the LNFGP for three reasons. First, it could improve the control of GERD through weight loss [2, 4]. Secondly, it could lower traction on the fundoplication improving bloating syndrome from Nissen [1, 4]. Finally, it could lower the risk of leak secondary to failed stapling [4]. No complications were reported by Talha [1] and Khazzaka [4]. Ospanov [2] reported two cases of postoperative hemorrhage (splenic injury, short gastric vessels bleeding). Lee [3] reported one case of leakage from the right side of the gastric wrap on POD 2 and another case of subphrenic abscess, both treated by sleeve gastrectomy (8% of major complications). Our report put forward a potentially lethal complication of LNFGP. We believe that the gastric perforation is the consequence of an antral obstruction due to a plication performed too close to the pylorus, leading to a high gastric pressure in the presence of a continent fundoplication. The main technical point is to end the gastric plication 3 to 6 cm above the pylorus in order to avoid this pylorus obstruction [1, 2, 3]. The plication is described as a double-layer suture, two interrupted [2] or inner interrupted and outer continuous suture [3]. Finally, the initial indication for performing a combined LNFGP in our patient remains subject to debate. We could not find any information about her weight before LNFGP but she was only overweight (BMI of 25.9 kg/m2) when arriving at our hospital. Resistance to the patient’s desire in regard to non-scientifically established procedures is advised.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest.



