-
PDF
- Split View
-
Views
-
Cite
Cite
Chloe Chan, Mohammed Zain Sohail, Pranai Buddhdev, Case report of combined iliac crest and ASIS apophysis avulsion fracture in an adolescent footballer, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab573, https://doi.org/10.1093/jscr/rjab573
Close - Share Icon Share
Abstract
Pelvic apophyseal avulsion fractures are uncommon injuries that typically occur in adolescents during sporting activities. Iliac crest (IC) apophyseal injuries represent a small percentage avulsion fracture around the pelvis with a reported incidence rate of 5%. We present a rare case of an adolescent boy who sustained a combined anterior superior iliac spine/iliac crest apophyseal avulsion fracture while playing football. With painful limited hip range of movement and inability to weight-bear, plain film and computed tomography scan illustrated a displaced fracture which was managed conservatively with an excellent clinical and radiological outcome. A review of apophyseal fractures around the pelvis, including incidence, mechanism of injury and treatment options regarding surgical versus conservative treatment, are discussed.
INTRODUCTION
Pelvic apophyseal avulsion fractures are unique injuries and were first described in the literature by Berry et al. in 1912 [1]. These injuries are usually sustained during sporting activities in the adolescents. The most common avulsion fractures occur at the anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS) and ischial tuberosity (IT) [2, 3]. Iliac crest (IC) apophysis avulsions are even more rare fractures with an incidence rate of just >5% among all apophyseal fractures around the pelvis [2, 3]. We present a rare case of an adolescent boy who sustained an avulsion fracture of the IC and ASIS apophysis.
CASE REPORT
A 15-year-old boy presented to our emergency department unable to weight-bear and complaining of severe right hip pain following a non-contact injury while playing football. He described a sudden onset of right hip and groin pain when he over-stretched for a ball with his right leg; his trunk rotated, hip flexed, knee fully extended and his foot internally rotated. He was unable to mobilize or weight-bear and required an ambulance to present to our institution. On physical examination, he had pain on all hip movements with limited hip flexion and internal rotation. There was bony tenderness on palpation along the anterior aspect of the hip and IC. Sensation within the dermatome of the lateral cutaneous femoral nerve (LCFN) was intact.
The anterior–posterior plain film X-Ray of pelvis demonstrated an avulsion fracture of the right ASIS and IC apophysis with 1.5 cm displacement (Fig. 1). Lateral view of the hip showed no extension into the joint. There was no radiological evidence of chronic overuse or previous injury. Computed tomography (CT) imaging was performed to better identify the injury; 3D volume reconstruction clearly demonstrated the unique fracture pattern of an ASIS avulsion in addition to an avulsion of the distal iliac apophysis extending ~5 cm with the described displacement (Figs 2–4).

AP radiograph following injury, demonstrating a large avulsion from the right hemipelvis, including the ASIS and portion of the IC apophysis (R - Right).
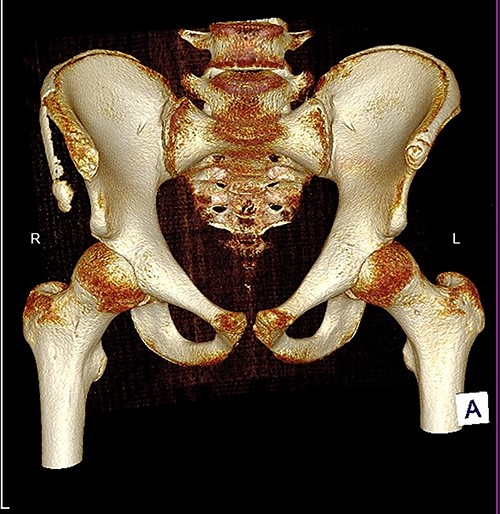
3D reconstruction of tomographic CT scan illustrating avulsion fracture of ASIS and IC apophysis with its latero-inferior displacement (R - Right, L - Left, A - Anterior).
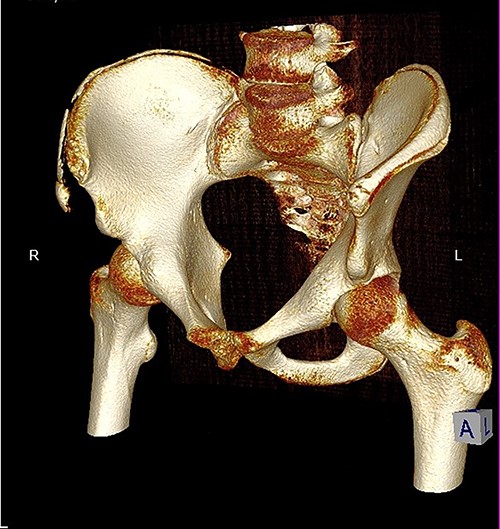
3D reconstruction of tomographic CT scan illustrating avulsion fracture of ASIS and IC apophysis with its latero-inferior displacement (R - Right, L - Left, A - Anterior).
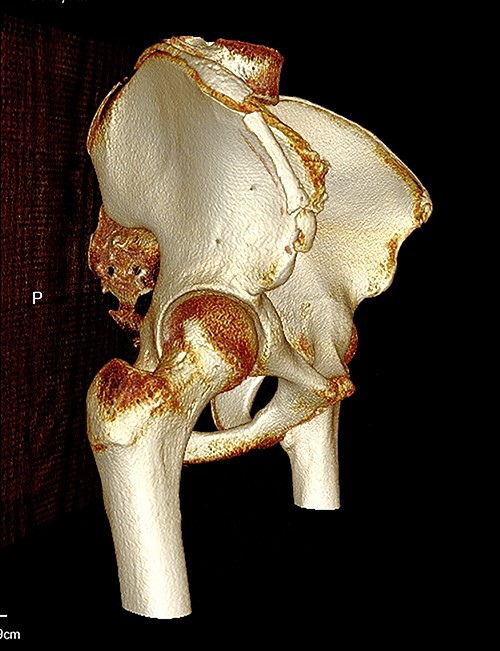
3D reconstruction of tomographic CT scan illustrating avulsion fracture of ASIS and IC apophysis with its latero-inferior displacement (P - Posterior).
After discussion of the surgical risks of fixation, including hardware irritation and LCFN dysfunction, a shared decision to treat the patient conservatively was reached. The patient was instructed to mobilize with crutches and attempt weight-bearing as comfort allowed. At a 4-week follow-up review, the patient presented with complete resolution of symptoms, full active hip range of motion, nil palpable tenderness and the ability to mobilize independently without walking aids. Radiographs performed showed significant callous formation between the pelvis and the fragment (Fig. 5). Return to sport was achieved by 8 weeks as per medical advice following a period of closed-chain exercises and self-directed rehabilitation.

Plain AP radiograph 4 weeks following injury, demonstrating callus formation between avulse bony fragments and right hemipelvis (L - Left).
DISCUSSION
Apophyseal avulsion fractures are unique injuries of children and adolescents. Apophyses are secondary ossification centres that contribute to the shape and size of the bones but not length [4]. Apophyses are the weakest point of the muscle–tendon-bone complex, resulting in their increased propensity for avulsion fractures secondary to sudden eccentric contractions of attached muscle groups. Due to the wide variety of presentations, clinicians need to have in-depth knowledge of the muscle groups and their attachments to the individual apophyses for appropriate management of these injuries.
The mean age of apophyseal avulsion fractures around the pelvis is 14.5 years [5]. The most commonly injured apophyses and their attachments include: the AIIS by the straight head of rectus, IT by the hamstrings, the ASIS by sartorius and parts of the tensor fascia lata (TFL) and the IC by the oblique abdominal muscles [4, 6, 7]. Frequently reported mechanisms of injuries include sprinting, kicking and tennis [3, 4, 6, 8, 9].
IC avulsion fractures account for ~5% of all apophyseal fractures around the pelvis and are most typically seen in sprinters who jump up and run with slight rotation of trunk [9]. They have also been reported in other sports, including gymnastics [10], wrestling [11] and football [8, 12]. These fractures typically displace proximally in accordance with the muscular pull of the abdominal oblique muscles [5, 8, 9]. Our case described a combined avulsion of the ASIS and IC apophysis with lateral and inferior displacement due to the action of TFL.
There are no established treatment guidelines for avulsion fractures of the ASIS or IC in the literature; however, the vast majority of cases treated conservatively have good outcomes [2, 3, 5, 7]. Displacement of >3 cm has been considered as a threshold for surgical management with open reduction internal fixation [11, 13]. A case series published by Li et al. [13] concluded patients who undergo surgical management have an expedited recovery and return to activity. Despite this, surgical management is associated with risk of injury to the lateral cutaneous nerve and irritation of the metal work [5]. We recommend a patient-centred approach with informed decision making regarding the outcomes of different treatment options and reserve surgical options for patients with associated articular injuries, neurovascular compromise and in cases where displacement is >3 cm.
Avulsion injuries of the apophyses around the hip and pelvis are common in adolescents who partake in sports. Knowledge of the common mechanisms, radiographic findings and treatment options should be highlighted to all those caring for this patient population to ensure appropriate and timely recognition and management.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



