-
PDF
- Split View
-
Views
-
Cite
Cite
Jessica Schembri Higgans, Keith Pace, John Sciberras, Warren Scicluna, Systemic BCGosis following intra-renal instillation of BCG: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab544, https://doi.org/10.1093/jscr/rjab544
Close - Share Icon Share
Abstract
Bacillus Calmette-Guerin (BCG) immunotherapy is a mainstay of adjunctive therapy for non-muscle-invasive bladder cancer. The instillation of BCG in the upper urinary tract after complete tumour eradication has also been studied and used after kidney-sparing management. It is effective in increasing the length of remission. However, it is also associated with rare but severe local and systemic side effects which may potentially become life-threatening. We present a case report of a 37-year-old gentleman who developed BCGosis following intra-renal instillation of BCG immunotherapy. The patient presented with systemic symptoms of jaundice, fever, myalgia and arthralgia, rather than local symptoms. Mycobacterium bovis infection was confirmed on blood cultures. The patient also developed hepatosplenomegaly, dyspnoea and pancytopaenia. BCGosis following intravesical instillation has been well documented in literature; to the best of our knowledge, this is the first case report documenting BCGosis following intra-renal instillation.
INTRODUCTION
Bacillus Calmette-Guerin (BCG) is instilled intravesically after transurethral resection of bladder (TURB) tumour for non-muscle invasive bladder cancer (NMIBC) and is superior to TURB alone or TURB with chemotherapy for preventing the recurrence of NMIBC [1]. It has been in use for over 40 years [2]. BCG immunotherapy has been studied as topical treatment for upper tract urothelial carcinoma (UTUC) in kidney-sparing management. It is usually well tolerated; however, it may lead to local and systemic infectious complications [3]. Disseminated BCG infection is also known as BCGosis. Dissemination may occur via the haematogenous route or vesicoureteric reflux [4]. Diagnosis requires a high index of suspicion. When accompanied by a relevant clinical history, the presence of randomly distributed granulomas should prompt consideration of BCGosis. In such cases, stains for acid-fast bacilli and targeted molecular assays should be performed [5]. Although systemic BCGosis following intravesical immunotherapy has been well documented in literature, there is little information about BCGosis following renal instillation.
CASE REPORT
A 37-year-old gentleman, diagnosed with right renal pelvis low grade non-invasive papillary UTUC and treated with a right flexible ureteroscopy and laser ablation, was receiving 6 monthly cycles of 100 mg BCG powder diluted in 60 ml of saline, delivered retrograde via a ureteric catheter into the right pelvi-calyceal system at 60 ml per hour.
He presented with right sided abdominal pain associated with jaundice, fever, myalgia and arthralgia after receiving his second dose of the penultimate cycle of intra-renal BCG instillation. He did not have any tuberculosis contacts. His parameters on admission were stable. C-reactive protein levels were 230 mg/l and white cell count (WCC) was 6.51 × 109/l. His liver function tests were deranged, with a mixed obstructive and hepatitic picture. A CT kidneys, ureters and bladder (KUB) showed mild diffuse dilatation of the right ureter and renal pelvis with minimal amount of peri-ureteric fat stranding (Fig. 1). A CT scan of the abdomen with intravenous contrast (IV) was performed, this showed a distended right ureter down to the vesicoureteric junction, peri-ureteric fat stranding and lymphadenopathy in the aorto-caval space together with splenomegaly and atelectatic changes (Fig. 2).

An initial CT KUB showed mild diffuse dilatation of the right renal pelvis (as indicated by the arrow).
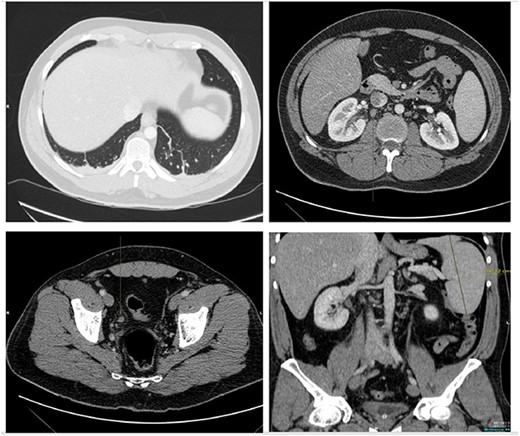
A CT scan of the abdomen with IV contrast showed atelactic changes in the lung bases (top left), reactive hilar nodes (top right), a distended right ureter all the way down to the vesicoureteric junction surrounded by fat stranding (bottom left) and splenomegaly (bottom right).
The patient was treated with IV piperacillin-tazobactam. However, he continued to have febrile temperature spikes. No growth was initially detected on blood cultures. The patient developed shortness of breath and respiratory alkalosis, for which a CT pulmonary angiography was done to exclude pulmonary embolism. Only dependent bilateral changes in the lower lobes and signs of mild pulmonary venous congestion were reported (Fig. 3). He was started on hydrocortisone, ethambutol, pyridoxine and rifampicin as empirical treatment for BCGosis. Hydrocortisone was eventually tailored down to prednisolone. Virology tests including hepatitis and immunodeficiency virus were run and these were negative. He continued spiking high temperatures and a repeat CT abdomen with IV contrast was performed which was largely unchanged from the previous scan (Fig. 4). An echocardiogram ruled out infective endocarditis. Incidentally he was in contact with a COVID-19 positive patient and was placed under quarantine for 14 days. Fortunately, he never developed COVID-19 infection. Another CT pulmonary angiography was performed in view of persisting shortness of breath but only mosaic attenuation in the lungs was present.
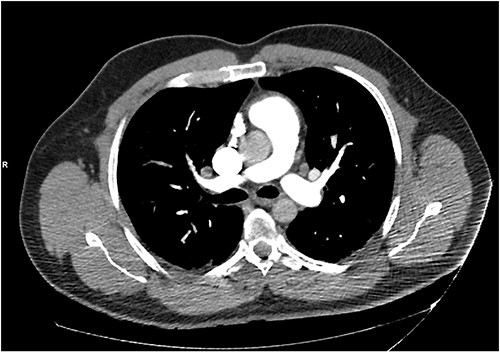
A CT pulmonary angiography was done to exclude pulmonary embolism. Only dependent bilateral changes in the lower lobes and signs of mild pulmonary venous congestion were noted.
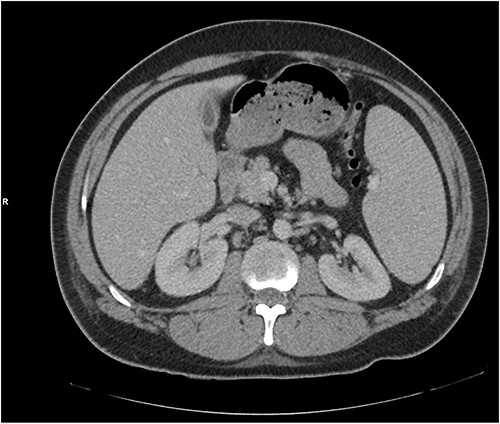
A repeat CT abdomen with IV contrast was performed which was largely unchanged from the previous scan, save for mild pericholecystic fluid.
The patient also developed pancytopaenia. The lowest WCC, haemoglobin and platelet count recorded were 1.51 × 109/l, 7.8 g/dl and 6 × 109/l, respectively. Three units of platelets were transfused to maintain platelet levels above 10 × 109/l. A bone marrow biopsy was performed but no mycobacterial growth was detected. Mycobacterium bovis was cultured 3 weeks after submission of blood cultures to the lab, and the anti-tuberculosis medications were continued. He was discharged after a total of 34 days of hospitalisation. Prednisolone was tailored down. Ethambutol was continued for a total of 2 months, whereas isoniazid and pyridoxine were continued for a total of 6 months. No further complications were reported.
DISCUSSION
TURB and BCG immunotherapy is recommended in international guidelines for NMIBC. Frequency and dosing of BCG depend on whether there is low, intermediate or high-risk disease [6]. Because of its efficacy, it is widely used, though one must be wary of the possible adverse side effects associated with BCG immunotherapy. In the EORTC study, 62.8 and 30.6% of participants experienced local and systemic side effects, respectively. The most common side effects included BCG induced cystitis, bacterial infection, urinary frequency, frank haematuria, malaise and fever. BCG sepsis was observed in 0.3% of patients [7].
In low-risk UTUC, kidney-sparing surgery is associated with lower morbidity without compromising oncological outcomes [8]. Since the patient was only 37 years old, kidney-sparing surgery with laser ablation was employed. Both antegrade and retrograde instillation of BCG immunotherapy have been studied after kidney-sparing surgery, with no known difference between method of administration in terms of recurrence or progression of disease. Both may result in ureteric obstruction and pyelo-venous influx which may lead to BCGosis [9]. Systemic manifestation of BCGosis can occur anywhere in the body. Multiple complications have been reported, ranging from prostatitis, to disseminated BCG infection and septicemia. Our patient developed hepatosplenomegaly and deranged liver function tests, dyspnoea and respiratory alkalosis. Pulmonary involvement in BCGosis is well document in the literature [3]. In this case, there was no evidence of military TB, pneumonia or granulomatous disease on imaging.
Fever of unknown origin and pancytopaenia secondary to BCGosis were also reported after intravesical instillation [10]. This complication has not been documented in literature after intra-renal instillation. Bladder mucosal damage and immunodeficiency were identified as host-specific risk factors for developing BCGosis. Apart from the history of UTUC, our patient was previously healthy. BCGosis has only been reported in males [3].
CONCLUSION
The insidious and possibly delayed onset and variety of local and systemic symptoms make the diagnosis of BCGosis difficult. Clinicians must have a low threshold for investigating patients with a history of BCG immunotherapy for mycobacterial infection in the presence of pyrexia of unknown origin and other ambiguous symptoms. Information about complications following intra-renal BCG instillation is scarce. This case report raises the importance of considering the diagnosis even following intra-renal instillation of BCG.
ACKNOWLEDGEMENTS
The authors would like to thank all the doctors, nurses and allied healthcare professionals who were involved in the patient’s care. Thanks also go to the Department of Surgery of Mater Dei Hospital, Malta.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding was sought or obtained.
ETHICAL APPROVAL
No ethical approval was necessary for this study. Data protection permission and approval was sought and obtained from the Mater Dei Hospital Data Protection Office.
CONSENT
A detailed consent form was signed by the patient and a copy of the case report was provided to the patient as well. The signed consent form can be provided upon request.
GUARANTOR
Jessica Schembri Higgans, E-mail: jessica.schembri-higgans@gov.mt.



