-
PDF
- Split View
-
Views
-
Cite
Cite
Mirwais Khan Hotak, Christo Joseph, A case of haemorrhagic cholecystitis with no risk factors, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab542, https://doi.org/10.1093/jscr/rjab542
Close - Share Icon Share
Abstract
Haemorrhagic cholecystitis (HC) is a rare cause of cholecystitis that can be fatal if management is delayed. HC could present in the setting of trauma, malignancy and bleeding diathesis, such as renal failure, cirrhosis and anticoagulation. Its symptoms are easily confused with acute calculous or acalculous cholecystitis and might include haemobilia or hematemesis as blood drains from the gallbladder into the gastrointestinal tract. Imaging of HC can be misleading unless the possibility of this diagnosis is considered. In this report, we present an interesting case of HC in a patient with none of the above comorbidities and the patient who was not on anticoagulation neither anti platelets. The case includes relevant imaging and a review of the literature on this rare subject.
INTRODUCTION
Haemorrhagic cholecystitis (HC) is a rare complication of acute cholecystitis [1]. Direct clinical diagnosis is nearly impossible because HC can appear with symptoms such as uncomplicated cholecystitis or bile duct obstruction, acute abdominal pain with hemodynamic repercussion and even hematemesis [2]. A haemorrhage within the gallbladder lumen may occur for a variety of reasons, including trauma, percutaneous interventions, obstructive cholecystitis, bleeding disorders, biliary neoplasms, biliary parasites or bleeding disorders. Imaging especially computed tomography (CT) can help diagnose by demonstrating the characteristic findings of wall thickening of the distended gallbladder and the heterogeneous materials inside. Here, we report the case of a patient with no anticoagulation or antiplatelet therapy with HC and no other risk factors.
CASE REPORT
We present the case of a 51-year-old patient who presented with 4-day history of colicky right upper quadrant (RUQ) pain that got worse over the preceding 12 hours. The abdominal pain was mainly localized to epigastric and RUQ, and the patient did not report any other symptoms. Her past medical history included asthma, hypothyroidism, appendectomy and two caesarean sections. She was not on any anticoagulant or antiplatelet agents. She had a similar but mild episode in the past, which correlated with gluten and resolved spontaneously or with buscopan. Physical examination revealed direct tenderness over the RUQ and epigastric region with rebound tenderness and guarding in the region of RUQ. Pathology test revealed white cell count of 13.1 (neutrophil 10.2) and C-reactive protein (CRP) of 116. Liver function test revealed a total bilirubin of 24, alkaline phosphatase of 74, alanine aminotransferase of 34, gamma-glutamyl transferase of 33 and lipase of 11.
CT abdomen with intravenous contrast revealed a distended gall bladder containing numerous lamellate calculi and high-density fluid along with gall bladder wall thickness and pericholecystic fluid compatible with acute haemorrhagic calculus cholecystitis (see Figs 1 and 2).
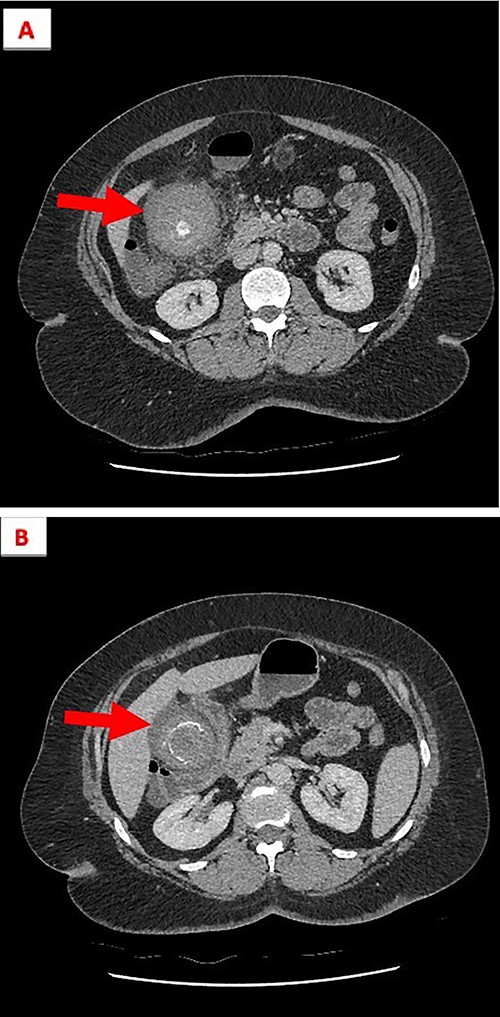
(A) The gallbladder contains numerous lamellated calculi and is distended with high-density fluid. (B) Gall bladder wall thickening and high-density fluid, both features are compatible with acute HC.
Consequently patient had emergency laparoscopic cholecystectomy and intraoperative cholangiogram (IOC). A much distended oedematous gall bladder was found with omental adhesions, and the IOC showed no anatomical abnormality and filling defect.
The histopathology macroscopically revealed a thickened gall bladder wall up to 8 mm in thickness, and mucosa appeared affected with cream fibrous band and generally haemorrhagic appearance. Microscopically the gall bladder showed evidence of widespread HC.
DISCUSSION
HC is a rare entity of acute cholecystitis that carries a high morbidity and mortality rate if management is delayed [1]. Pathogenesis may be due to haemorrhage into an acalculous gallbladder as the primary cause of cholecystitis via chemical irritation. Alternatively, transmural infarction and erosion of the gallbladder wall in established acute cholecystitis, usually gangrenous, may cause bleeding secondarily. HC has many possible causes, including trauma, neoplasms, aneurysmal rupture, portal hypertension, coagulopathy or anticoagulation therapy. It is possible that the documented proliferating prescription of these agents may increase the incidence of this entity in the future [3].
Interestingly, a case of HC reported in a patient with acalculous HC and SARS-CoV-2 infection. The possible explanation was suggested by the trophism of SARS-CoV2 with the biliopancreatic tract might have been at the basis of the development of an acalculous cholecystitis, which is per se a relatively uncommon event, and it was probably worsened by the simultaneous administration of low-molecular weight heparin [4].
Pandya and O’Malley reported a case in which a patient on anticoagulants underwent an urgent cholecystostomy but unfortunately the hyperdense contents increased within common bile duct on follow-up CT, which required further exploration. This highlights that the treatment for HC in patients on anticoagulant therapy is an urgent cholecystectomy which is necessary to prevent more serious complications and morbidity to the patient [5].
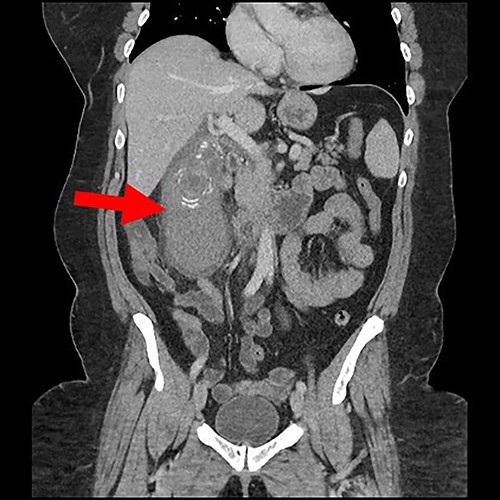
Coronal view of gall bladder with high-density fluid and calculi.
Regardless of cause, the treatment for cholecystitis should follow the Tokyo Guideline 2018 (TG2018). TG2018 states that cholecystectomy is a definitive treatment for cholecystitis, whereas a percutaneous cholecystostomy can be performed for acute management bridging to surgery in patients with significant comorbidities [6].
In summary, HC is rare but its complications are not. Complications can be associated with the risk of significant morbidity and mortality. When reviewing patients with symptoms of biliary colic or cholecystitis, it is prudent to maintain a high index of suspicion especially if the patient has predisposing factors like anticoagulant therapy. Early diagnosis of this potentially fatal complication is important to facilitate urgent surgical management.
Contrary to the above discussion, our patient was not on anticoagulation and did not have any other risk factors. She presented with acute calculus cholecystitis and required urgent cholecystectomy. The question raised here, do we need to treat HC patient differently with more urgency or treat them all the same as acute cholecystitis.



