-
PDF
- Split View
-
Views
-
Cite
Cite
Ramesh De Silva, My Pham, Michael Devadas, Hosen Kiat, Long-term adjustable gastric band with resultant megaoesophagus causing cardiac compression, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab540, https://doi.org/10.1093/jscr/rjab540
Close - Share Icon Share
Abstract
Oesophageal dilatation following laparoscopic-assisted gastric banding (LAGB) is a well-described complication reported in up to 80% of LAGB patients [ 1, 2]. Severe oesophageal dilatation in addition to aperistalsis is known as megaoesophagus. Symptomatic compression cardiac compression from oesophageal dilatation as a complication of LAGB is an extremely rare complication and is presented in this case report.
INTRODUCTION
Megaoesophagus of sufficient volume to compress the left atrium causing shortness of breath is uncommon. While megaoesophagus is a rare complication of laparoscopic adjusted gastric banding (LAGB), which itself is now only employed in limited contexts, we believe it can be a clinically important consequence of an overinflated band and is under-reported.
Preoperative oesophageal manometry has a limited predictive value in identifying patients at risk of oesophageal dysmotility following LAGB [3]. Our case highlights megaesophagus as an adverse post-LAGB complication which can present late and that appropriate education for patients and their general practitioners and periodic follow-up surveillance by the surgeons of tell-tale symptoms may expedite early diagnosis and treatment.
CASE REPORT
The patient was a 57-year-old smoker who was referred with pre-syncope, gastroesophageal reflux symptoms in the setting of hypertension and dyslipidaemia. Four years prior to presentation, he underwent LAGB and he had achieved weight loss from 159 kg (body mass index (BMI): 51.3) to 96 kg (BMI: 30.9), 76.8% excess weight loss and 39.6% total body weight loss.
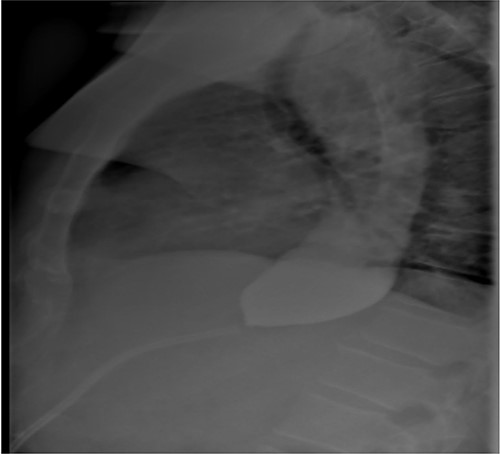
As part of the assessment, computed tomography (CT) coronary angiogram study was performed and it demonstrated a large fluid-filled oesophagus causing partial compression of the left atrium. Barium swallow (Fig. 1A and B), CT chest and abdomen (Fig. 2A and B) and transthoracic echocardiography (TTE) showed a 7.1-cm dilated oesophagus causing left atrial compression and a small hiatal hernia (Fig. 3).
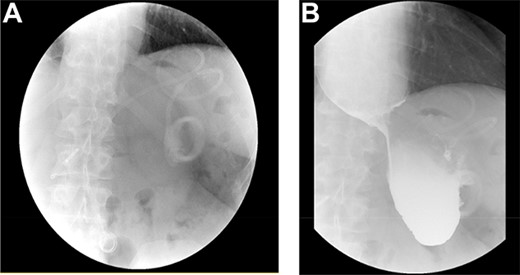
(A) LAGB more inferior and rotated consistent with band slippage; (B) marked distension of the oesophagus and contrast hold up at the level of the slipped band.
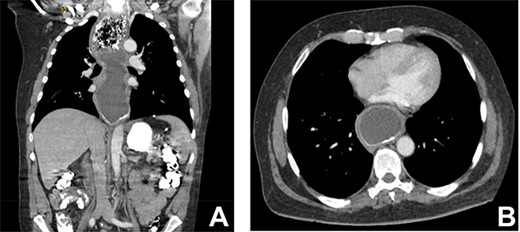
(A) CT coronal image of chest and abdomen demonstrating megaoesophagus secondary to the LAGB; (B) CT axial image of chest demonstrating megaoesophagus causing left atrial compression.
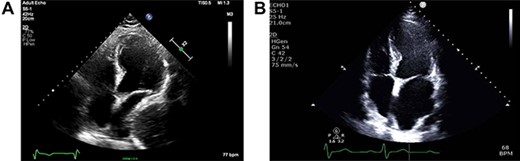
(A) ECHO showing left atrial compression from megaoesophagus during diastole; (B) ECHO showing normal-sized left atrium 3 months after band removal.
Given significant cardiac compression and PE’s symptoms, the LAGB was removed laparoscopically without complication. Capsulotomy was performed with immediate distension of the distal stomach once the band was removed, indicating that there was significant degree of obstruction. There was no ischaemia to the serosal surface of the stomach. Seven hundred millilitres of retained food and fluid in the oesophagus were evacuated during gastroscopy. The underlying oesophageal mucosa was cobble-stoned with histopathology, demonstrating severe chronic inflammation. There was no dysplasia or malignancy.
Three months after band removal, the patient reported complete resolution of his symptoms. Repeat gastroscopy demonstrated oesophageal mucosal healing and no residual hiatal hernia. TTE showed that left atrium was moderately enlarged (but to a lesser extent compared to previous study) and normal left and right ventricular systolic function and dimensions with estimated left ventricular ejection fraction of 60%. Furthermore, the post-operative Barium swallow study (Fig. 4) demonstrated a 6.7-cm oesophageal dilatation and dysmotility. There was no significant delay in passage of barium into a non-distended stomach. Since band removal his weight had increased by 17 kg (112.8 kg, BMI: 36.4). Further discussions with the patient led to laparoscopic sleeve gastrectomy a month later (Fig. 5).
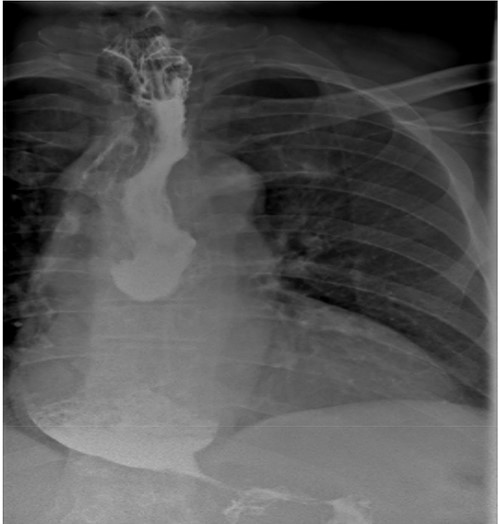
Barium contrast swallow study demonstrating ongoing oesophageal dilatation, however, free passage of contrast into the stomach.
Post-gastric sleeve barium contrast swallow study demonstrating ongoing oesophageal dilatation, but passage of contrast into remnant stomach.
DISCUSSION
This case features a late presentation of megaesophagus as a symptomatic sequala of an otherwise successful LAGB. Removal of the gastric band led to symptom resolution in our case and can be followed with more durable bariatric procedures.
Oesophageal dilatation following LAGB is a well-described complication reported in up to 80% of LAGB patients [1]. Severe oesophageal dilatation in addition to aperistalsis with new secondary and tertiary contractions is known as megaoesophagus [2]. The incidence of megaoesophagus varies in the literature (up to 71% of LAGB patients) with a contributing factor being that there is no consensus on the size of dilatation [2]. Megaoesophagus has been arbitrarily defined as 30% change of oesophagus width from baseline in a study [1]. Another study defined it as >35 mm regardless of preoperative oesophageal size [3]. The mean development of megaoesophagus is 32–60 months [2, 4, 5].
The cause of megaoesophagus following LAGB is likely to be multifactorial. Poor compliance with diet in psychologically unprepared patients probably contributes to oesophageal dilatation [2]. Also, band slippage or band overinflation can impair relaxation of the lower oesophageal sphincter, leading to oesophageal dilatation. Additionally, patients with insufficient preoperative LOS are more likely to develop oesophageal dilatation and dysmotility despite normal band position and stoma width. In the case of the patient, the authors postulated that the band itself probably impairs LOS relaxation [6].
In the case of this patient, the extent of his megaesophagus resulted in significant compression of the left atrium observed on TTE and CT, which fortunately did not cause haemodynamic compromise or obvious and clinically evident intracardiac thrombus. To our knowledge, compression of the cardiac chambers by oesophageal dilatation is an extremely rare complication of LAGB. A systematic literature review of megaoesophagus in LAGB patients was performed (Table 1).
| Study . | Patient characteristics . | Investigations . | Outcome . |
|---|---|---|---|
| Ahmed et al. (2015) [7]. Image illustration | 50-year-old female with left lobe pneumonia and sepsis. Presented with 1-week fever, productive cough and nausea/vomiting. Laparoscopic gastric banding 10 years ago. Weight loss of 82 kg from 172 kg. | TTE showed a well-circumscribed compressive echogenic mass posterior to the left atrium. CT revealed a dilated oesophagus measuring 5 cm. | Symptom resolution following deflation of the balloon of gastric band.* |
| Leitman et al. (2010) [8]. Case report | 37-year-old man with syncopal episodes post-swallowing. Gastric banding 2 years ago. | Echocardiography revealed a mass, which appeared to compress the left atrium.^ | Symptom resolution following deflation of the balloon of gastric band.* |
| Study . | Patient characteristics . | Investigations . | Outcome . |
|---|---|---|---|
| Ahmed et al. (2015) [7]. Image illustration | 50-year-old female with left lobe pneumonia and sepsis. Presented with 1-week fever, productive cough and nausea/vomiting. Laparoscopic gastric banding 10 years ago. Weight loss of 82 kg from 172 kg. | TTE showed a well-circumscribed compressive echogenic mass posterior to the left atrium. CT revealed a dilated oesophagus measuring 5 cm. | Symptom resolution following deflation of the balloon of gastric band.* |
| Leitman et al. (2010) [8]. Case report | 37-year-old man with syncopal episodes post-swallowing. Gastric banding 2 years ago. | Echocardiography revealed a mass, which appeared to compress the left atrium.^ | Symptom resolution following deflation of the balloon of gastric band.* |
*Unclear if radiological or endoscopic resolution of megaoesophagus.
Unclear of size of megaoesophagus.
| Study . | Patient characteristics . | Investigations . | Outcome . |
|---|---|---|---|
| Ahmed et al. (2015) [7]. Image illustration | 50-year-old female with left lobe pneumonia and sepsis. Presented with 1-week fever, productive cough and nausea/vomiting. Laparoscopic gastric banding 10 years ago. Weight loss of 82 kg from 172 kg. | TTE showed a well-circumscribed compressive echogenic mass posterior to the left atrium. CT revealed a dilated oesophagus measuring 5 cm. | Symptom resolution following deflation of the balloon of gastric band.* |
| Leitman et al. (2010) [8]. Case report | 37-year-old man with syncopal episodes post-swallowing. Gastric banding 2 years ago. | Echocardiography revealed a mass, which appeared to compress the left atrium.^ | Symptom resolution following deflation of the balloon of gastric band.* |
| Study . | Patient characteristics . | Investigations . | Outcome . |
|---|---|---|---|
| Ahmed et al. (2015) [7]. Image illustration | 50-year-old female with left lobe pneumonia and sepsis. Presented with 1-week fever, productive cough and nausea/vomiting. Laparoscopic gastric banding 10 years ago. Weight loss of 82 kg from 172 kg. | TTE showed a well-circumscribed compressive echogenic mass posterior to the left atrium. CT revealed a dilated oesophagus measuring 5 cm. | Symptom resolution following deflation of the balloon of gastric band.* |
| Leitman et al. (2010) [8]. Case report | 37-year-old man with syncopal episodes post-swallowing. Gastric banding 2 years ago. | Echocardiography revealed a mass, which appeared to compress the left atrium.^ | Symptom resolution following deflation of the balloon of gastric band.* |
*Unclear if radiological or endoscopic resolution of megaoesophagus.
Unclear of size of megaoesophagus.
Despite the patient developing megaoesophagus after LAGB, he achieved significant weight loss. A previous study showed that, compared to their counterparts without megaoesophagus, patients with megaoesophagus had lesser weight loss. The authors explained that this was likely due to the oesophagus being as an additional space for food [2].
The immediate management of megaoesophagus involves deflation of the gastric band and then band removal. In their review of 257 patients who had undergone LAGB, Arias and colleagues reported megaoesophagus in five patients, all of whom improved their symptoms following band removal [2]. In our case, the decision was made to remove the gastric band to good effect.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



