-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmad E Al-Mulla, Ali Altabeekh, Ahmad Al-Jafar, Shaimaa Dashti, Successful laparoscopic extraction of trichobezoar due to Rapunzel syndrome: first reported case in Kuwait, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab532, https://doi.org/10.1093/jscr/rjab532
Close - Share Icon Share
Abstract
Rapunzel syndrome is a rare condition typically found in young female patients with mental or psychiatric disorders. It manifests as a large trichobezoar extending beyond the pylorus into the small intestine and leads to various adverse conditions. Early diagnosis and prompt management are crucial to avoiding complications. These bezoars are extracted endoscopically, laparoscopically and via open surgery (most common). In this current report, we discuss a successful laparoscopic extraction of a trichobezoar in a 12-year-old girl with acute abdominal pain due to small-bowel obstruction. We describe our technique compared with others’ techniques and include a literature review on this topic.
INTRODUCTION
Bezoar is defined as an indigestible mass in the gastrointestinal tract, especially in the stomach [1]. The second most common bezoar is the trichobezoar, which occurs in young female psychiatric patients [2]. Trichobezoars are usually confined to the stomach. In extremely rare cases, they extend beyond the pylorus and into the small intestine, which is known as Rapunzel syndrome (RS) [3]. This rare case report describes the unusual presentation of abdominal pain in a 12-year-old girl that was managed laparoscopically.
CASE PRESENTATION
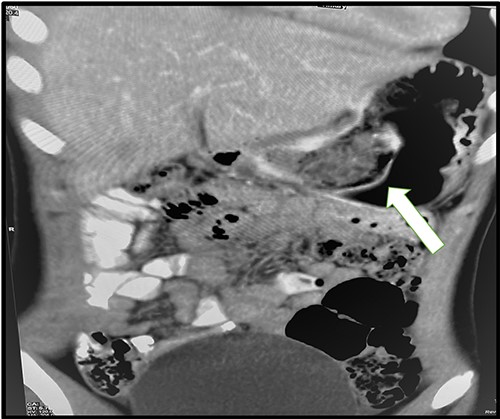
A 12-year-old girl presented to our surgical emergency department complaining of a 5-day history of severe colicky epigastric and right upper quadrant (RUQ) pain associated with vomiting, nausea and anorexia. The patient had been experiencing similar symptoms for the past month. She was otherwise healthy with no previous medical history. According to her family, she was an active child and top in her class at school. On examination, her vitals were as follows: pulse 110 bpm, blood pressure 120/70 mmHg and temperature 37°C. Abdominal examination revealed epigastric and RUQ tenderness. Laboratory tests revealed a normal complete blood count, renal function test, liver function test, C-reactive protein and coagulation profile; however, she had elevated amylase (141 U), lipase (138 U/L) and urine amylase (1776 U/L). The abdominal ultrasound was unremarkable. The patient was admitted to the surgical ward and kept fasting with intravenous fluids, an anti-spasmodic and painkillers. However, she did not improve symptomatically; her lipase increased (148 U/L), and her abdominal pain became more aggravated. A computed tomography (CT) scan of the abdomen and pelvis revealed only minimal pelvic fluid with a foreign body at the pylorus and first part of the duodenum (Fig. 1). An endoscopic attempt to extract was unsuccessful due to the size of the bezoar as well as the high possibility for respiratory tract obstruction.
Therefore, the family was consulted about removing the bezoar surgically. The procedure was performed laparoscopically with three working ports: two working 5-mm ports and one 11-mm camera port. A 5-cm gastrostomy at the body of the stomach was done (Fig. 2). A large bezoar was found at the pylorus, extending to the duodenum. The large bezoar was removed with an endo grasper, and the stomach was closed with a Vicryl suture. An Endo-leak test was performed, and the specimen was removed from the umbilical port with an endo bag. The bezoar was extracted with no spillage in the abdominal cavity, and none remained in the stomach (Fig. 3).
POST-OPERATIVE
The post-operative recovery was unremarkable. The patient stayed for 3 days and was given broad-spectrum antibiotics. She was discharged after resuming a normal diet and regular bowel habits, and she was also referred to a psychiatrist for further follow-up. Her first outpatient visit was uneventful; she had no abdominal pain, no change in appetite and no change in bowel habit, and her wounds were clean. The psychiatric clinic had followed up with her, and she had resumed school and was doing well.
DISCUSSION
Bezoars can be classified into four main types: phytobezoars, trichobezoars, pharmacobezoars and lactobezoars [4]. Trichotillomania and trichophagia are common in young women aged 13–20 years who have intellectual disabilities or psychiatric disorders [2]. Trichotillomania is an impulse control disorder characterized by the repetitive urge to pull out one’s hair, leading to hair loss. Many of these patients also ingest their hair and animal hair as well as rug, synthetic and natural fibres [5]. The slippery nature of the hair traps it within the gastric folds, leading to bezoar formation [6]. RS is a unique manifestation of an advanced gastric trichobezoar, first described in literature by Vaughn et al. in 1968. RS has three standard features: (i) trichobezoar in the stomach, (ii) long hair strands that extend from the stomach to the small intestine and sometimes the large bowel and (iii) gastrointestinal symptoms [7]. It is typically asymptomatic until the bezoar reaches a substantial size, which leads to abdominal discomfort (37%), weight loss and anorexia (38%), later developing into nausea or postprandial vomiting (38%) and abdominal cramps [8]. Physical examination often shows a palpable mobile abdominal mass (70%) and loss of scalp and eyebrow hair as well as eyelashes [9]. Long-standing gastric bezoars lead to adverse complications, such as obstruction, perforation, bleeding, intussusception, peritonitis, ulceration, obstructive jaundice, weight loss, pancreatitis and mortality [10]. In our case, the patient presented with acute abdominal pain with a CT scan suggestive of small bowel obstruction. Elevation of lipase and amylase was due to migration of the bezoar to the ampulla of Vater, causing spasms and congestion of the sphincter of Oddi, resulting in bile regurgitation and trypsin activation once the pressure in the bowel was higher than in the pancreatic duct [11]. Diagnosis of trichobezoar can be made by ultrasound, CT scan, barium meal and endoscopy.
RS treatment aims to extract the trichobezoar endoscopically, laparoscopically or via open surgery. Upper endoscopy is less invasive and more cost-effective; however, it is not recommended in these cases due to its lower success rate and potential for airway obstruction and respiratory arrest. Most cases are primarily managed with open surgery, which was described in a retrospective study of seven cases of gastric bezoars; all patients required exploratory laparotomy [12]. The first laparoscopic extraction of a bezoar was conducted in 1998; only a few cases that were successfully managed laparoscopically are mentioned in the literature.


There are three techniques are described in the literature. First, Don et al. described passing a 10-mm port into the gastric wall to create an intra-gastric port, followed by removing the specimen with a gastroscope [13]. Second, Kanetala et al. described a similar approach using two gastric ports to cut the bezoar into small fragments and removing them via gastroscopy; both approaches are time-consuming [13, 14]. The third technique, described by Shami et al. [15], was used in our case. In our case, we performed a gastrotomy, extracting the specimen with a grasper and placing it in a Endo-bag then removing it through the 10-mm camera port. We did not experience any spillage or post-operative infection. A laparoscopic approach is also an option; however, it can be time-consuming and technically challenging cases. There is as of yet no gold standard procedure due to the rarity of the disease; however, it should be performed with attention to patient safety and outcomes.
CONCLUSION
RS is an extensive form of trichobezoar, it can present a variety of complications. Imaging is an essential tool to diagnose the disorder because it presents with vague symptoms. Trichobezoar must be considered in the differential diagnosis of a young female with pancreatitis. Management is primarily by open surgery, but it can be performed laparoscopically (dependent on the patient’s clinical characteristics).
ACKNOWLEDGEMENTS
Special thanks to all members of our surgical department and the head of the department, Dr Khaled Al Bassam, for his special interest in continuing publication and documentation. Also, I would like to extend my appreciation to the management at Farwaniya Hospital and their exceptional data reservation and electronic filing system; without it, this project could not have happened.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



