-
PDF
- Split View
-
Views
-
Cite
Cite
Lauren M Turner, Phillip Jeans, Stephen Robson, A pedunculated small bowel gastrointestinal stromal tumour (GIST) masquerading as an ovarian tumour, Journal of Surgical Case Reports, Volume 2021, Issue 12, December 2021, rjab514, https://doi.org/10.1093/jscr/rjab514
Close - Share Icon Share
Abstract
While gastro-intestinal stromal tumours (GIST) are the most common non-epithelial neoplasms of the gastrointestinal tract, 10% occur externally. Symptomatology is therefore broad, dependent on location. A 42-year-old female presented to the Emergency Department after 12 hours of severe right lower abdominal, preceded by vague pain over two weeks. Imaging revealed a right-sided 7.5 × 5.8 × 5.6 cm ovarian cystic lesion, suspicious for torsion. Laparoscopically, the lesion was densely adherent to small and large bowel, and she was proceeded to resection of an assumed primary ovarian neoplasm. Histopathology revealed an infarcted epithelioid GIST, high-grade with clear margins (stage pT3). There are only 24 cases of GISTs pre-operatively mistaken for gynaecological neoplasms. Additionally, there are reports of GISTs metastasizing to ovaries. Both computed tomography and ultrasound are non-specific, including hypo- and hyperechoic features. In all published cases, imaging was not able to identify presumed gynaecological neoplasms as GISTS. Differential diagnoses for pelvic masses should include non-gynaecological tumours.
INTRODUCTION
Gastro-intestinal stromal tumours (GISTs) are the most common non-epithelial tumours of the gastrointestinal tract. While they represent <1% of GI tumours, they make up ~80% of all non-epithelial tumours [1]. The majority occur in the stomach and small intestine, although they can occur anywhere from the oesophagus to anus [1]. About 10% arise outside of the GIT, for example the pancreas, retroperitoneum or mesentery: a small proportion arise in locations giving rise to incorrect preoperative diagnoses [2]. GISTs are associated with a number of symptoms including GI bleeding, obstruction, perforation, dysphagia, pain or an abdominal mass, depending on their location. Pre-operative diagnosis is difficult as imaging is heterogeneous with non-specific features. Here, we present an unusual case of an ovarian-cyst appearing pedunculated GIST, originating adjacent to the ileo-caecal junction.
CASE REPORT
A 42-year-old Australian woman posted with the Australian Government to a developing nation during the COVID-19 pandemic experienced the sudden onset of acute severe lower abdominal pain. The acute episode had been preceded by several vague episodes of pain for ~2 weeks. Assessment at the local hospital revealed a right-sided cystic lesion in the pelvis measuring 7.5 × 5.8 × 5.6 cm appearing to arise from the right ovary. The lesion was suggestive either of an endometriotic or haemorrhagic cyst or, possibly, a mucinous ovarian tumour.
The pain settled somewhat and the patient contacted an Australian medical team for advice. The clinical picture suggested partial torsion of an ovarian cystic lesion and, due to the risk of a complete torsion and ovarian tumour infarction, advice was given to the Government that the patient be repatriated to Australia in view of the extreme pressure on medical resources where she was. However, the patient suffered another severe episode of pain suggestive of complete torsion and laparoscopy was undertaken. The images were captured on a phone camera and sent to Australia—the surgeons found a large cystic lesion apparently contiguous with the right ovary (Fig. 1) that was densely adherent to the small bowel and sigmoid colon. Further conservative management with analgesia was given and the patient was flown to Australia to undergo COVID-19 quarantine. She had an ongoing requirement for analgesics but no further acute episodes. Upon release from quarantine local ultrasound revealed a heterogeneous solid and cystic lesion of unchanged dimensions ‘strongly suggestive of primary ovarian neoplasia’ (Fig. 2). The remainder of the examination was normal Her CA-125 level was 15 kU/L (NR < 36).
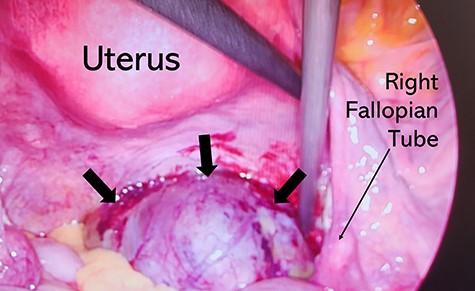
Intraoperative photograph demonstrating a large cystic lesion appearing to be contiguous with the right ovary.

Abdominal ultrasound imaging demonstrating a heterogeneous solid and cystic lesion 75 × 53 mm.
The following morning laparoscopy was performed with peritoneal washings taken for cytology. Present was a large round mass encased in adhesions to the right ovary and fallopian tube, small bowel, anterior rectum and sigmoid colon. A laparotomy was performed and the mass carefully dissected free. It appeared to arise on a pedicle from the small bowel, ~90 cm from the ileo-caecal junction. Histopathology revealed a largely infarcted solid lesion with areas characteristic for a GIST of the epithelioid type (positive for dog 1/CD 117 (KIT protein), negative for Sox 10/cytokeratin). (Fig. 3) The appearances were of a high-grade tumour with clear margins at stage pT3. The adjacent small bowel was normal with no evidence of invasion. The patient had an uncomplicated post-operative recovery.
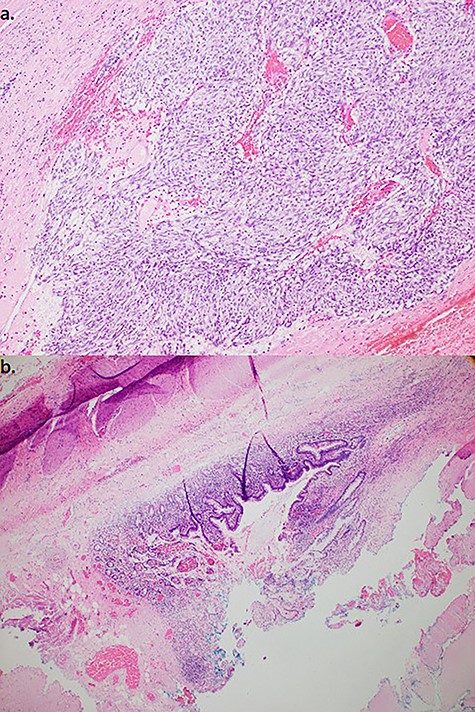
(a). Resected specimen (100×) stained with Haematoxylin and Eosin demonstrated epitheloid type cells composed in nests and (b). adjacent small bowel mucosa/muscularis. Immunohistochemistry (not shown)—10% tumour cells positive for Ki67, positive staining for CD117, negative staining for CD68, SMA and desmin, consistent with GIST.
DISCUSSION
GISTS are frequently difficult to diagnose with certainty on imaging due to their typically heterogeneous, non-specific features [3]. A small number of cases (24) have been reported in which a GIST is thought to be a gynaecological neoplasm until surgery. The origins of these tumours include the bowel, stomach, rectovaginal septum, uterus and ovary [4–7]—in none of the published cases was the correct diagnosis made beforehand. To add complexity, there are several reports of small bowel or stomach GISTs metastasizing to the ovary [8].
The appearance of a GIST on imaging makes preoperative diagnosis challenging [3]. Ultrasound appearance of the tumours can be atypical and include both hypo- and hyperechoic masses [9, 10]. Computed tomography (CT) imaging might have the greatest diagnostic utility allowing determination of the extent of invasion in the GI wall and surrounding organs, the possibility of resection, and the presence or absence of likely metastatic disease. However, in none of the previously reported cases was CT able to define the origin of the tumour in cases thought to be of gynaecological origin. The detection of a pelvic mass should always raise consideration of non-gynaecological tumours with appropriate pre-operative planning.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Lee Bornman for his assistance in supplying pathological images.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING STATEMENT
The authors received no financial support for the research, authorship and/or publication of this article.
References
- ultrasonography
- computed tomography
- epithelium
- cysts
- emergency service, hospital
- genital neoplasms, female
- intestine, large
- intestine, small
- intestines
- ovarian neoplasms
- pain
- abdomen
- diagnostic imaging
- neoplasms
- ovary
- pelvic mass
- gastrointestinal tract
- stromal neoplasm
- gastrointestinal stromal tumor
- histopathology tests



