-
PDF
- Split View
-
Views
-
Cite
Cite
Taylor Raines Williams, Joel Okoli, Spontaneous resolution of gastric perforation caused by an ingested foreign body: a case report, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab506, https://doi.org/10.1093/jscr/rjab506
Close - Share Icon Share
Abstract
Foreign body ingestions are commonly seen and are usually uneventful. Very rarely, ingested foreign bodies will cause perforation of the gastrointestinal tract, which can lead to peritonitis, abscesses or fistulation. This is the case of a patient with vague abdominal pain after voluntary ingestion of bleach and an ink pen. The ink pen was found lodged in the gastric antral wall on esophagogastroduodenoscopy. The foreign body spontaneously migrated into the gastric lumen and was successfully removed with endoscopy.
INTRODUCTION
Ingestion of a foreign body is a common occurrence in adults, especially those with psychological problems. These foreign bodies will usually pass through the gastrointestinal (GI) tract without event. Less than 1% of these objects will cause perforation of the GI wall, and perforation can lead to a wide range of clinical presentations ranging from acute peritonitis to no symptoms at all [1–4]. The standard treatment for ingested foreign bodies is endoscopic removal but, in some cases, patients will require laparoscopy or laparotomy for removal [7, 8]. We present a case of gastric antral wall perforation caused by a purposefully ingested ink pen in which the gastric defect spontaneously resolved and the foreign body was ultimately removed endoscopically.
CASE PRESENTATION
A 43-year-old incarcerated woman with borderline personality disorder and a long history of swallowing various foreign objects in periods of stress presented to the emergency department after swallowing a cup of bleach. Her surgical history was significant for multiple celiotomies for retrievals of purposefully ingested foreign bodies. During evaluation, she also admitted to swallowing an ink pen 3 weeks prior to swallowing the bleach for which she did not seek medical evaluation. She reported no food intolerance or changes in bowel function secondary to swallowing these objects. She presented with mild abdominal pain and cramping, and her vital signs and laboratory investigations were all within normal limits. Her abdominal exam was notable for mild tenderness to palpation diffusely. Computed tomography (CT) of the abdomen (Fig. 4) showed a linear foreign body in the distal gastric antrum penetrating the inferior wall and extending into the adjacent peritoneal fat. No free air or free fluid was appreciated. Initial esophagogastroduodenoscopy (EGD) was significant for mild erythema and edema to the esophageal and duodenal mucosa as a result of the caustic ingestion, and the pen was found to be deeply perforating the stomach antral wall with no associated ulcer or edema (Fig. 1). The depth at which the foreign body was lodged was uncertain, so there was concern for organ involvement outside of the gastric wall. Repeat EGD was done to assess for manifestations of esophageal, gastric or duodenal injuries from her caustic ingestion, and it revealed normal gastric mucosa (Fig. 2). A joint case was planned with the gastroenterology service for endoscopic foreign body retrieval, possible laparoscopic retrieval and gastric repair and possible open retrieval and gastric repair. The patient was taken to the operating room for the third EGD, which revealed spontaneous migration of the foreign body from the perforation site into the lumen of the gastric body (Fig. 3a). Additionally, there was spontaneous closure of the site of previous perforation (Fig. 3b and c). The ink pen was easily removed transorally using an endoscopic snare, and no further surgical intervention was required. After the procedure, the patient reported complete resolution of her abdominal pain and was able to tolerate a regular diet without problems.
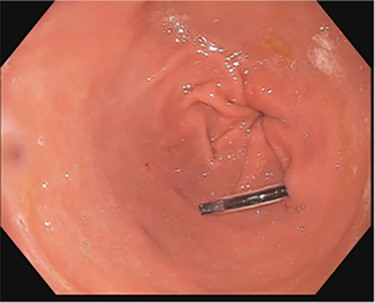
EGD on initial presentation; gastric antrum with foreign body perforating through the gastric wall.
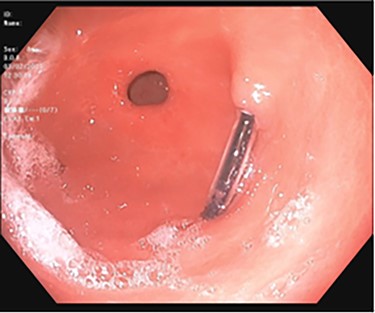
Subsequent EGD 3 days later; gastric antrum with foreign body perforating through the gastric wall; normal gastric mucosa after ingestion of bleach.
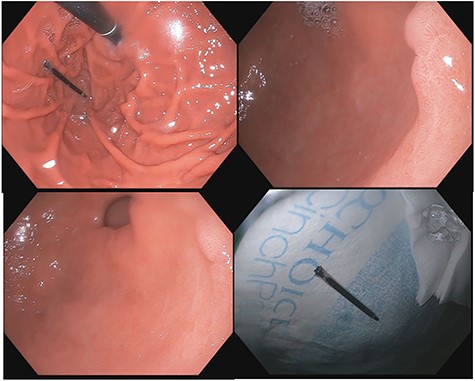
(a–d) Subsequent EGD 1 week later; (a) foreign body in the fundus of the stomach; (b and c) irregularity in the antrum corresponding to site of previous perforation; (d) ink pen after transoral endoscopic removal.
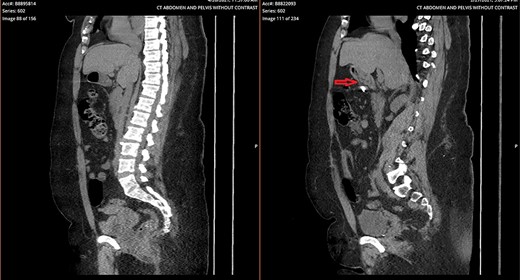
Side-by-side comparison of foreign body perforating through stomach (right) and sealed site of perforation after endoscopic removal (left).
DISCUSSION
The accidental ingestion of foreign bodies is a relatively common occurrence and is usually dietary in origin. In the adult population, fish bones are the most ingested object (up to 84%) [1, 2, 10]. Purposeful ingestion is most common among incarcerated, psychiatric, alcoholic and senile populations. Most ingested foreign objects (80–90%) will pass uneventfully through the GI tract, but <1% of the ingested foreign bodies will cause perforation of the GI tract. Thin, pointed objects have the greatest risk of causing perforation, and these injuries are typically diagnosed by CT scan and endoscopy [2–4, 10].
Perforation tends to occur at sites of anatomic angulation, such as the duodenal loop, duodenojejunal junction, terminal ileum, sigmoid colon and appendix [5, 8, 9]. Gastric perforations are rarer and patients who experience them can have varied clinical presentations, including acute peritonitis, intra-abdominal abscess or completely asymptomatic [11]. Linear objects can migrate into adjacent organs, such as the liver and pancreas, and can cause fistulation or abscess formation [1, 2, 5, 8]. Perforations in the stomach, duodenum and large intestine tend to have non-acute presentations, and up to 92% of them will be asymptomatic [4]. It is likely that the thicker gut wall of the stomach and large intestine causes foreign bodies to perforate more gradually. The adjacent omentum, fibrin and abdominal organs, such as the liver, may also assist in ‘sealing’ the perforation site thereby preventing peritonitis [4, 7]. It is also possible that the same mechanism that promotes spontaneous closure of a percutaneous endoscopic gastrostomy (PEG) tract after inadvertent PEG tube removal plays a role in the healing of the gastric wall following accidental perforation.
After an object has perforated the gastric wall, the foreign body can either lie in the visceral lumen at the site of perforation, pass through the perforation site and lie free in the peritoneal cavity or migrate to a distal organ, or as demonstrated in this case, fall back into the lumen of the stomach [6]. Alternatively, objects can perforate through the gastric wall and can be spontaneously expelled through the anterior abdominal wall [12]. If it falls back into the lumen, it can then either pass through the GI tract uneventfully or can be removed with endoscopic therapy. Given the risk of severe sequelae that can result from an ingested sharp object, endoscopic retrieval is the preferred treatment [11]. For objects that remain lodged in the GI wall, endoscopic treatment is also first-line because it allows the advantages of a non-invasive operation. If the object cannot be removed endoscopically or if the perforation has caused peritonitis, abdominal abscess or a persistent wall defect after removal, laparoscopic or open surgery is indicated [7, 8]. In this case, the object spontaneously dislodged from the gastric antral wall and the wall defect spontaneously resolved, so surgery was not indicated.
CONCLUSIONS
In summary, this was an unusual case of an ingested ink pen that penetrated the gastric antral wall and spontaneously migrated back into the gastric lumen. The gastric wall defect then closed spontaneously ~3 weeks later while the patient remained relatively asymptomatic. The foreign body was successfully removed with endoscopically and the patient recovered without complications.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
We confirm that any aspect of the work covered in this manuscript, that has involved either experimental animals or human patients, has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
CONSENT FOR PUBLICATION
We confirm that consent to publish any individual person’s data in any form has been obtained from those persons. We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing, we confirm that we have followed the regulations of our institutions concerning intellectual property.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
AUTHORS’ CONTRIBUTIONS
T.R.W., MD, was responsible for the primary concept and design, acquisition and interpretation of data, drafting and revision of article and final approval of version to be published. J.O. took care of the revision of article. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. We understand that the corresponding author is the sole contact for the editorial process (including editorial manager and direct communications with the office). She is responsible for communicating with the other authors about the progress, submissions of revisions and final approval of proofs. We confirm that we have provided a current, correct email address which is accessible by the corresponding author.
ACKNOWLEDGEMENTS
I would like to thank Dr Ed Childs, Dr Shaneeta Johnson and the entire Department of Surgery at the Morehouse School of Medicine for their continued support and encouragement of my research endeavors.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
We confirm that there has been no significant financial support for this work which could have influenced its outcome.



