-
PDF
- Split View
-
Views
-
Cite
Cite
Saeid Safaei, Mirbahador Athari, Parisa Azimi, Ahmadreza Mirbolook, Taravat Yazdanian, Farhad Hamzehzadeh, Simple bone cyst of spinal vertebrae: two case reports and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 11, November 2021, rjab507, https://doi.org/10.1093/jscr/rjab507
Close - Share Icon Share
Abstract
Simple bone cyst (SBC) is not a common lesion in the spine and especially in the vertebral body. We intend to report two cases of SBC located in the vertebral body, and review the literature. Two cases include a 24 year-old male and 26 year-old male with vertebral body lesion of T12 and L5 vertebrae,retrospectively. Both lesions were found to be SBC and confirmed by pathology. Both cases were managed with surgery, the cavity was filled with bone graft and posterior spinal fusion and instrumentation with pedicle screws, and rods were carried out. There was no recurrence. There have been 21 cases of SBCs in English literature, and only 8 cases have been reported in the vertebral body. SBC is a rare benign lesion in the spine and it should be considered in the differential diagnosis when suggested by radiologic investigations.
INTRODUCTION
Simple or solitary bone cysts (SBC) also known as unicameral bone cysts are benign lesions commonly seen in the peripheral skeleton [1]. The exact pathogenesis of the lesion is unknown [2]. They commonly affect the long bones in children and adolescents [1]. The most frequent sites are proximal humerus and proximal femur [1, 3]. The spinal column is not a common site for SBC [4]. It may be asymptomatic, and hence the incidence is unknown. Patient’s age, history, clinical and laboratory data and radiologic findings can help with the diagnosis [5]. Spinal SBC, especially in the vertebral body, is not a common lesion and there is limited data regarding managing these lesions [6–26].
Our goal was to present two cases of SBC who were referred to our department of spine surgery and review the literature.
Case 1
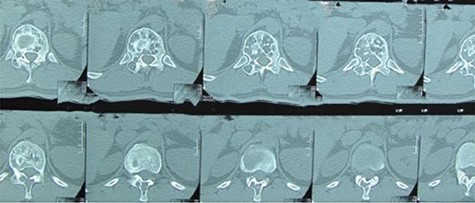
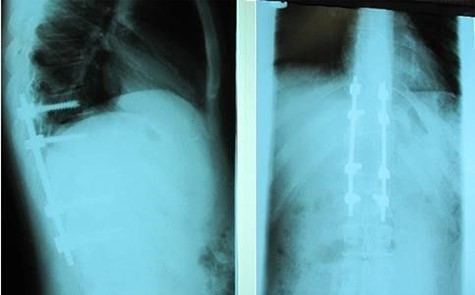
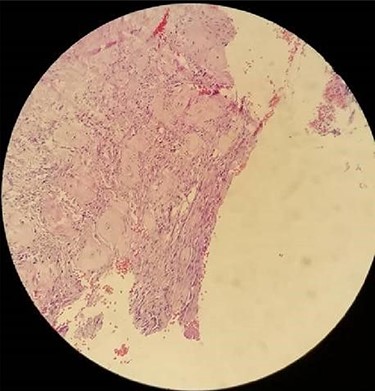
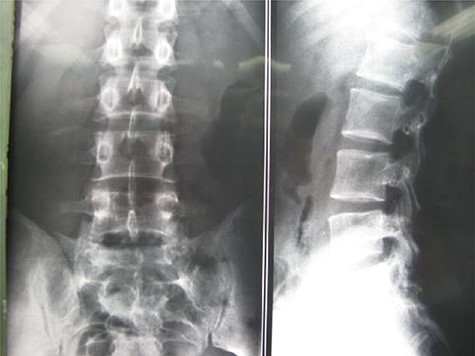
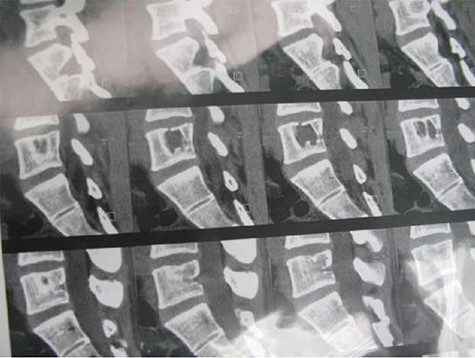
A 24-year-old male presented with acute low back pain with no prior traumatic events. Physical examination was unremarkable except for tenderness over the lower thoracic spine. The laboratory tests including complete blood count, renal function tests, alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase, serum calcium, serum phosphorus and parathyroid hormone were all within normal limits. Initially, the patient was treated conservatively but the pain did not improve. Lumbar X-ray showed mild height loss and fracture of the superior endplate of T12 vertebra (Fig. 1). Computed tomography (CT) showed a multi-lobulated osteolytic lesion within the T12 body with extension to the right pedicle and transverse process (Fig. 2). Magnetic resonance imaging (MRI) revealed a well-defined lesion with low signal intensity on T1 and high signal intensity on T2 weighted images (Fig. 3). The bone scan showed a cold spot at the site of the lesion. The patient underwent surgery and excisional biopsy through the posterior approach. A large clear fluid-filled cavity was curetted and the cavity was filled with an autologous bone graft from iliac crest. Posterior spinal fusion was performed with instrumentation with pedicle screws from T10 to L2 and a mixture of autologous bone graft and allograft was used to achieve better fusion (Fig. 4). Pathology report confirmed the diagnosis of SBC and the patient received no further treatment (Fig. 5). The patient had no recurrence in 10-year follow up.
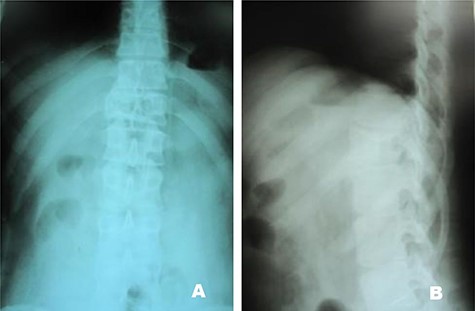
Case 1, (A): Anterior–posterior; (B): Lateral pre-operative X-ray.
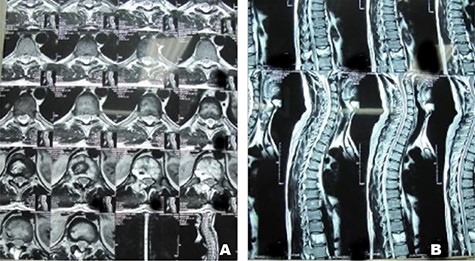
Case 1, (A): Axial T2-weighted MR image of twelfth thoracic spine vertebrae; (B): Sagittal T2-weightedimages of thoracic spine vertebrae.
Case 2
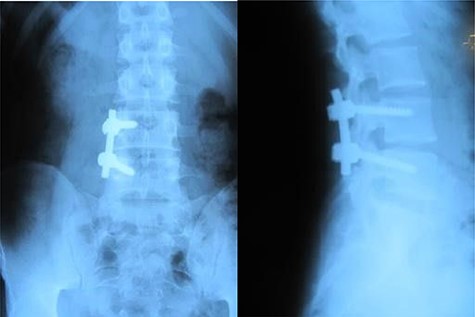
A 26-year-old male presented with pain over the lower lumbar area. Physical examination and laboratory tests were unremarkable with no neurologic deficit. X-ray and CT scans showed a lytic lesion with a sclerotic border in the right half of the body of the L5 vertebra (Figs 6 and 7). MRI showed a well-defined low signal lesion in T1 weighted images and high signal lesion in T2 weighted images (Fig. 8). The bone scan was negative. The patient underwent surgery and the lesion was extracted through the right pedicle and the remaining cavity was filled with an autologous bone graft from the iliac crest and right-side posterior fusion was done from L4 to L5 (Fig. 9). The pathology report was consistent with SBC. The patient had no recurrence seven years after surgery.
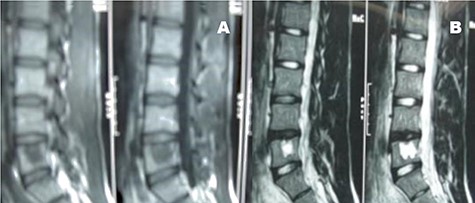
Case 2, Sagittal T2-weighted and T1-weighted MR images of lumbar vertebrae show the body and homogeneous cystic lesion of L5.
DISCUSSION
This study presents two cases of spinal SBC managed surgically with no recurrence in long-term follow-up. Table 1 gives a summary of previously reported SBCs of the vertebral column in English literature [6–26]. The diagnosis of spinal SBC may be difficult and delayed until operative treatment when it is confirmed by histological assessment. Hence, spinal SBC should be considered in the differential diagnosis of spinal lesions.
Summary of 2 new cases and 21 reported cases of bone cyst of lumbar vertebral body
| Author (ref.) . | Year . | Country . | Age/Gender . | Location in spine . | Level . | Involved sites . | Treatment . | Follow-up . | Outcome in last follow-up . |
|---|---|---|---|---|---|---|---|---|---|
| Dawson et al. [6] | 1976 | USA | 37/M | Cervical | C4 | Body | Curettage and bone graft | 10 months | Complete cyst obliteration and no recurrence |
| Wu et al. [7] | 1981 | USA | 30/M | Lumbar | L3 | Spinous process | Resection | 1 years | No recurrence |
| Brodsky et al. [8] | 1986 | USA | 31/M | Lumbar | L1 | Body | Curettage and bone graft | 3 years | No recurrence |
| Matsumoto et al. [9] | 1990 | Japan | 40/M | Lumbar | L2 | Body | Curettage with bone graft | 7 years | He remained free of symptoms in the back and had a high level of sports activity. |
| Nakagawa et al. [10] | 1994 | Japan | 63/F | Cervical | C5 | Body | Excision | 13 months | Pain resolved; paresthesia improved and no recurrence |
| Park CK et al. [11] | 1997 | South Korea | 12/F | Cervical | C2 | Spinous process | Curettage without bone graft | 2 years | Good prognosis and no recurrence |
| Shen Q et al. [12] | 1998 | China | 4/M | Cervical | C2 | Body and odontoid | Curettage with bone graft | 2.5 years | The post-operative recovery was uneventful, but the child wore a plaster collar for three months. at last follow-up male was well. |
| Zenmyo et al. [13] | 2000 | Japan | 13/F | Cervical | C7 | Spinous process | Surgical exploration, curettage, filled w/ hydroxyapatite | NA | After surgery pain resolved |
| Lee et al. [14] | 2000 | Taiwan | 14/M | Cervical | C7 | Spinous process and lamina | Surgical exploration, curettage, removal of SP | NA | Pain resolved |
| Chang et al. [15] | 2001 | South Korea | 25/M | Lumbar | L5 | Lamina | Excision | 1 year | The patient was satisfied and no recurrence |
| Snell et al. [16]. | 2001 | USA | 10/F | Cervical | C7 | Body and lateral mass | Excision and fusion | 1 year | She was without complain and no recurrence |
| Tsirikos et al. [17] | 2002 | USA | 17/F | Thoracic | T9 | Spinous process and lamina | Excision | NA | Good prognosis and no recurrence |
| Ha et al. [18] | 2003 | South Korea | 53/F | Lumbar | L1 | Pedicle | Surgical resection | 7 years | A favorable result was achieved and no recurrence |
| Coskun Bet al. [19] | 2004 | Turkey | 26/F | Cervical | C4 | Spinous process | Excision | NA | Good prognosis and no recurrence |
| Ogata et al. [20] | 2004 | Japan | 50/F | Lumbar | L3 | Pedicle | Curettage | NA | The patient’s low back pain decreased and no recurrence |
| Huang ZY et al. [21] | 2014 | China | 32/F | Cervical | C2 | Body and odontoid | Curettage and bone graft | 1 year | Good prognosis and no recurrence |
| Nayman et al. [22] | 2015 | Turkey | 34/M | Lumbar | L3 | Body | NA | NA | NA |
| Funayama T et al. [23]. | 2016 | Italy | 16/F | Lumbar | L4 | Body | Percutaneous steroid injection | 7 months | The patient was asymptomatic and the beginning of bony healing was evident. |
| Fazeli MA et al. [24] | 2016 | Iran | 28/F | Lumbar | L5 | Body | Conservative | NA | NA |
| Boude et al. [25] | 2017 | Colombia | 13/F | Cervical | C2 | Body | Curettage and excision | 1 year | Good prognosis and no recurrence |
| Kaoa et al. [26] | 2020 | China | 17/F | Lumbar | L4 | All columns | Excision and reconstruction | 10 years | Good prognosis and no recurrence |
| Present study case 1 | 2020 | Iran | 24/M | Thoracic | T12 | Body and right pedicle and transverse process | Surgical resection and fusion | 10 years | Good prognosis and no recurrence |
| Present study case 2 | 2020 | Iran | 26/M | Lumbar | L5 | Body | Surgical resection and fusion | 7 years | Good prognosis and no recurrence |
| Author (ref.) . | Year . | Country . | Age/Gender . | Location in spine . | Level . | Involved sites . | Treatment . | Follow-up . | Outcome in last follow-up . |
|---|---|---|---|---|---|---|---|---|---|
| Dawson et al. [6] | 1976 | USA | 37/M | Cervical | C4 | Body | Curettage and bone graft | 10 months | Complete cyst obliteration and no recurrence |
| Wu et al. [7] | 1981 | USA | 30/M | Lumbar | L3 | Spinous process | Resection | 1 years | No recurrence |
| Brodsky et al. [8] | 1986 | USA | 31/M | Lumbar | L1 | Body | Curettage and bone graft | 3 years | No recurrence |
| Matsumoto et al. [9] | 1990 | Japan | 40/M | Lumbar | L2 | Body | Curettage with bone graft | 7 years | He remained free of symptoms in the back and had a high level of sports activity. |
| Nakagawa et al. [10] | 1994 | Japan | 63/F | Cervical | C5 | Body | Excision | 13 months | Pain resolved; paresthesia improved and no recurrence |
| Park CK et al. [11] | 1997 | South Korea | 12/F | Cervical | C2 | Spinous process | Curettage without bone graft | 2 years | Good prognosis and no recurrence |
| Shen Q et al. [12] | 1998 | China | 4/M | Cervical | C2 | Body and odontoid | Curettage with bone graft | 2.5 years | The post-operative recovery was uneventful, but the child wore a plaster collar for three months. at last follow-up male was well. |
| Zenmyo et al. [13] | 2000 | Japan | 13/F | Cervical | C7 | Spinous process | Surgical exploration, curettage, filled w/ hydroxyapatite | NA | After surgery pain resolved |
| Lee et al. [14] | 2000 | Taiwan | 14/M | Cervical | C7 | Spinous process and lamina | Surgical exploration, curettage, removal of SP | NA | Pain resolved |
| Chang et al. [15] | 2001 | South Korea | 25/M | Lumbar | L5 | Lamina | Excision | 1 year | The patient was satisfied and no recurrence |
| Snell et al. [16]. | 2001 | USA | 10/F | Cervical | C7 | Body and lateral mass | Excision and fusion | 1 year | She was without complain and no recurrence |
| Tsirikos et al. [17] | 2002 | USA | 17/F | Thoracic | T9 | Spinous process and lamina | Excision | NA | Good prognosis and no recurrence |
| Ha et al. [18] | 2003 | South Korea | 53/F | Lumbar | L1 | Pedicle | Surgical resection | 7 years | A favorable result was achieved and no recurrence |
| Coskun Bet al. [19] | 2004 | Turkey | 26/F | Cervical | C4 | Spinous process | Excision | NA | Good prognosis and no recurrence |
| Ogata et al. [20] | 2004 | Japan | 50/F | Lumbar | L3 | Pedicle | Curettage | NA | The patient’s low back pain decreased and no recurrence |
| Huang ZY et al. [21] | 2014 | China | 32/F | Cervical | C2 | Body and odontoid | Curettage and bone graft | 1 year | Good prognosis and no recurrence |
| Nayman et al. [22] | 2015 | Turkey | 34/M | Lumbar | L3 | Body | NA | NA | NA |
| Funayama T et al. [23]. | 2016 | Italy | 16/F | Lumbar | L4 | Body | Percutaneous steroid injection | 7 months | The patient was asymptomatic and the beginning of bony healing was evident. |
| Fazeli MA et al. [24] | 2016 | Iran | 28/F | Lumbar | L5 | Body | Conservative | NA | NA |
| Boude et al. [25] | 2017 | Colombia | 13/F | Cervical | C2 | Body | Curettage and excision | 1 year | Good prognosis and no recurrence |
| Kaoa et al. [26] | 2020 | China | 17/F | Lumbar | L4 | All columns | Excision and reconstruction | 10 years | Good prognosis and no recurrence |
| Present study case 1 | 2020 | Iran | 24/M | Thoracic | T12 | Body and right pedicle and transverse process | Surgical resection and fusion | 10 years | Good prognosis and no recurrence |
| Present study case 2 | 2020 | Iran | 26/M | Lumbar | L5 | Body | Surgical resection and fusion | 7 years | Good prognosis and no recurrence |
NA: not available; SP: spinous process.
Summary of 2 new cases and 21 reported cases of bone cyst of lumbar vertebral body
| Author (ref.) . | Year . | Country . | Age/Gender . | Location in spine . | Level . | Involved sites . | Treatment . | Follow-up . | Outcome in last follow-up . |
|---|---|---|---|---|---|---|---|---|---|
| Dawson et al. [6] | 1976 | USA | 37/M | Cervical | C4 | Body | Curettage and bone graft | 10 months | Complete cyst obliteration and no recurrence |
| Wu et al. [7] | 1981 | USA | 30/M | Lumbar | L3 | Spinous process | Resection | 1 years | No recurrence |
| Brodsky et al. [8] | 1986 | USA | 31/M | Lumbar | L1 | Body | Curettage and bone graft | 3 years | No recurrence |
| Matsumoto et al. [9] | 1990 | Japan | 40/M | Lumbar | L2 | Body | Curettage with bone graft | 7 years | He remained free of symptoms in the back and had a high level of sports activity. |
| Nakagawa et al. [10] | 1994 | Japan | 63/F | Cervical | C5 | Body | Excision | 13 months | Pain resolved; paresthesia improved and no recurrence |
| Park CK et al. [11] | 1997 | South Korea | 12/F | Cervical | C2 | Spinous process | Curettage without bone graft | 2 years | Good prognosis and no recurrence |
| Shen Q et al. [12] | 1998 | China | 4/M | Cervical | C2 | Body and odontoid | Curettage with bone graft | 2.5 years | The post-operative recovery was uneventful, but the child wore a plaster collar for three months. at last follow-up male was well. |
| Zenmyo et al. [13] | 2000 | Japan | 13/F | Cervical | C7 | Spinous process | Surgical exploration, curettage, filled w/ hydroxyapatite | NA | After surgery pain resolved |
| Lee et al. [14] | 2000 | Taiwan | 14/M | Cervical | C7 | Spinous process and lamina | Surgical exploration, curettage, removal of SP | NA | Pain resolved |
| Chang et al. [15] | 2001 | South Korea | 25/M | Lumbar | L5 | Lamina | Excision | 1 year | The patient was satisfied and no recurrence |
| Snell et al. [16]. | 2001 | USA | 10/F | Cervical | C7 | Body and lateral mass | Excision and fusion | 1 year | She was without complain and no recurrence |
| Tsirikos et al. [17] | 2002 | USA | 17/F | Thoracic | T9 | Spinous process and lamina | Excision | NA | Good prognosis and no recurrence |
| Ha et al. [18] | 2003 | South Korea | 53/F | Lumbar | L1 | Pedicle | Surgical resection | 7 years | A favorable result was achieved and no recurrence |
| Coskun Bet al. [19] | 2004 | Turkey | 26/F | Cervical | C4 | Spinous process | Excision | NA | Good prognosis and no recurrence |
| Ogata et al. [20] | 2004 | Japan | 50/F | Lumbar | L3 | Pedicle | Curettage | NA | The patient’s low back pain decreased and no recurrence |
| Huang ZY et al. [21] | 2014 | China | 32/F | Cervical | C2 | Body and odontoid | Curettage and bone graft | 1 year | Good prognosis and no recurrence |
| Nayman et al. [22] | 2015 | Turkey | 34/M | Lumbar | L3 | Body | NA | NA | NA |
| Funayama T et al. [23]. | 2016 | Italy | 16/F | Lumbar | L4 | Body | Percutaneous steroid injection | 7 months | The patient was asymptomatic and the beginning of bony healing was evident. |
| Fazeli MA et al. [24] | 2016 | Iran | 28/F | Lumbar | L5 | Body | Conservative | NA | NA |
| Boude et al. [25] | 2017 | Colombia | 13/F | Cervical | C2 | Body | Curettage and excision | 1 year | Good prognosis and no recurrence |
| Kaoa et al. [26] | 2020 | China | 17/F | Lumbar | L4 | All columns | Excision and reconstruction | 10 years | Good prognosis and no recurrence |
| Present study case 1 | 2020 | Iran | 24/M | Thoracic | T12 | Body and right pedicle and transverse process | Surgical resection and fusion | 10 years | Good prognosis and no recurrence |
| Present study case 2 | 2020 | Iran | 26/M | Lumbar | L5 | Body | Surgical resection and fusion | 7 years | Good prognosis and no recurrence |
| Author (ref.) . | Year . | Country . | Age/Gender . | Location in spine . | Level . | Involved sites . | Treatment . | Follow-up . | Outcome in last follow-up . |
|---|---|---|---|---|---|---|---|---|---|
| Dawson et al. [6] | 1976 | USA | 37/M | Cervical | C4 | Body | Curettage and bone graft | 10 months | Complete cyst obliteration and no recurrence |
| Wu et al. [7] | 1981 | USA | 30/M | Lumbar | L3 | Spinous process | Resection | 1 years | No recurrence |
| Brodsky et al. [8] | 1986 | USA | 31/M | Lumbar | L1 | Body | Curettage and bone graft | 3 years | No recurrence |
| Matsumoto et al. [9] | 1990 | Japan | 40/M | Lumbar | L2 | Body | Curettage with bone graft | 7 years | He remained free of symptoms in the back and had a high level of sports activity. |
| Nakagawa et al. [10] | 1994 | Japan | 63/F | Cervical | C5 | Body | Excision | 13 months | Pain resolved; paresthesia improved and no recurrence |
| Park CK et al. [11] | 1997 | South Korea | 12/F | Cervical | C2 | Spinous process | Curettage without bone graft | 2 years | Good prognosis and no recurrence |
| Shen Q et al. [12] | 1998 | China | 4/M | Cervical | C2 | Body and odontoid | Curettage with bone graft | 2.5 years | The post-operative recovery was uneventful, but the child wore a plaster collar for three months. at last follow-up male was well. |
| Zenmyo et al. [13] | 2000 | Japan | 13/F | Cervical | C7 | Spinous process | Surgical exploration, curettage, filled w/ hydroxyapatite | NA | After surgery pain resolved |
| Lee et al. [14] | 2000 | Taiwan | 14/M | Cervical | C7 | Spinous process and lamina | Surgical exploration, curettage, removal of SP | NA | Pain resolved |
| Chang et al. [15] | 2001 | South Korea | 25/M | Lumbar | L5 | Lamina | Excision | 1 year | The patient was satisfied and no recurrence |
| Snell et al. [16]. | 2001 | USA | 10/F | Cervical | C7 | Body and lateral mass | Excision and fusion | 1 year | She was without complain and no recurrence |
| Tsirikos et al. [17] | 2002 | USA | 17/F | Thoracic | T9 | Spinous process and lamina | Excision | NA | Good prognosis and no recurrence |
| Ha et al. [18] | 2003 | South Korea | 53/F | Lumbar | L1 | Pedicle | Surgical resection | 7 years | A favorable result was achieved and no recurrence |
| Coskun Bet al. [19] | 2004 | Turkey | 26/F | Cervical | C4 | Spinous process | Excision | NA | Good prognosis and no recurrence |
| Ogata et al. [20] | 2004 | Japan | 50/F | Lumbar | L3 | Pedicle | Curettage | NA | The patient’s low back pain decreased and no recurrence |
| Huang ZY et al. [21] | 2014 | China | 32/F | Cervical | C2 | Body and odontoid | Curettage and bone graft | 1 year | Good prognosis and no recurrence |
| Nayman et al. [22] | 2015 | Turkey | 34/M | Lumbar | L3 | Body | NA | NA | NA |
| Funayama T et al. [23]. | 2016 | Italy | 16/F | Lumbar | L4 | Body | Percutaneous steroid injection | 7 months | The patient was asymptomatic and the beginning of bony healing was evident. |
| Fazeli MA et al. [24] | 2016 | Iran | 28/F | Lumbar | L5 | Body | Conservative | NA | NA |
| Boude et al. [25] | 2017 | Colombia | 13/F | Cervical | C2 | Body | Curettage and excision | 1 year | Good prognosis and no recurrence |
| Kaoa et al. [26] | 2020 | China | 17/F | Lumbar | L4 | All columns | Excision and reconstruction | 10 years | Good prognosis and no recurrence |
| Present study case 1 | 2020 | Iran | 24/M | Thoracic | T12 | Body and right pedicle and transverse process | Surgical resection and fusion | 10 years | Good prognosis and no recurrence |
| Present study case 2 | 2020 | Iran | 26/M | Lumbar | L5 | Body | Surgical resection and fusion | 7 years | Good prognosis and no recurrence |
NA: not available; SP: spinous process.
Differential diagnosis of the spinal lesion can be narrowed by patients’ age, history, laboratory test, imaging studies and location of the tumor. The most common differential diagnoses for SBC are aneurysmal bone cyst, brown tumor (hyperparathyroidism), infection and less commonly giant cell tumor. Every spine lesion should be approached carefully and pathologic confirmation is prudent. In our cases, due to benign course of disease and imaging that suggested a benign lesion, we decided to do an open biopsy and definite surgery at the same time. It should be stated that if any sign of malignant lesion was encountered, the surgery would have stopped and only biopsy would have been performed.
To the best of our knowledge, 21 cases of SBCs affecting the vertebra have been reported in the English literature. SBCs were found in cervical (n = 10, 47.6%), lumbar (n = 10, 47.6%) and thoracic (n = 1, 4.8%) regions. Although, SBCs can involve one or multiple parts of the vertebra (body, pedicle, lamina or spinous process), only eight cases of SBC in the vertebral body were reported. (Table 1). The reported cases were more common in women (n = 13, 61.9%) than men (n = 8, 38.1%). The reported age ranges from 4 to 50 years, which is usually presented in the second decade [27]. Usually, diagnosis of SBC disease is based on pathologic confirmation due to its rarity and non-specific clinical presentation.
Management of SBC of the spine is not well described. Spine Instability Neoplastic Score can be used to evaluate spine instability [28, 29]. Corticosteroid injection had been described for lesion in the peripheral skeleton can be considered when the risk of fracture is low [30, 23]. At present, there is no gold standard for treatment for SBCs and Surgery may not be the optimal treatment for patients except for large lesions or pathologic fracture [21]. Majority of cases in the literature were treated surgically, including resection and curettage with or without bone grafting, and no recurrence has been reported (Table 1). Both of our patients were confirmed by pathology report and had a good prognosis and no recurrence in long-term follow-up (10 and 7 years).
We recommend SBC as a differential diagnosis in young patients with an unremarkable laboratory tests and suggestive imaging.
In conclusion, this study presents two cases of SBCs and reviews the literature. Surgery shows promising outcomes in large SBCs in the vertebral body with a high risk of fracture.



