-
PDF
- Split View
-
Views
-
Cite
Cite
Kristopher Bujold-Pitre, Olivier Mailloux, Diverticulitis of the appendix—case report and literature review, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab488, https://doi.org/10.1093/jscr/rjab488
Close - Share Icon Share
ABSTRACT
Appendiceal diverticulitis is a rare diagnostic most often mistaken for an acute appendicitis.
A 72-year-old man presented with a transfixing abdominal pain for 48 hours. Appendicitis was diagnosed on computed tomography scan, but a neoplasm could not be excluded. A laparoscopic hemicolectomy was performed after a surgical consensus considering the neoplastic appearance of the lesion and anatomical feature. Histopathology finally revealed an appendiceal diverticulitis.
Appendiceal diverticulum is a rare condition. Most will lead to an appendiceal diverticulitis, which present similarly to an appendicitis. Perforation rate and mortality rate are much higher in appendiceal diverticulitis than in appendicitis. Furthermore, appendiceal diverticular disease is strongly associated with neoplasms, especially mucinous neoplasms and thus pseudomyxoma peritonei.
Considering the high complication rate and malignant association, an appendicectomy in case of an appendiceal diverticulitis or of an incidental finding of appendiceal diverticulosis should be recommended to the patient.
INTRODUCTION
Diverticulitis of the appendix is a rare diagnostic most often mistaken for an acute appendicitis due to its alike presentation. In fewer cases, diverticulitis of the appendix can be interpreted as a neoplastic lesion of the appendix. We hereby present such a case with a literature review of the subject.
CASE REPORT
A 72-year-old man was referred to the emergency room (ER) by his physician for a 48-hour abdominal pain. The pain was located in the left upper quadrant and was characterized as initially transfixing but had mostly subsided by the time the patient consulted to the ER. The patient’s medical record was significant for an iatrogenic hypothyroidism, a right inguinal herniorrhaphy and two negative colonoscopies. The physical examination showed a soft abdomen and no fever. The total white blood cells count was 13.0 × 109. A computed tomography (CT) scan was performed and revealed an enlarged appendix filled with liquid with surrounding fat stranding compatible with an acute appendicitis, although a mucocele could not be excluded (see Fig. 1).

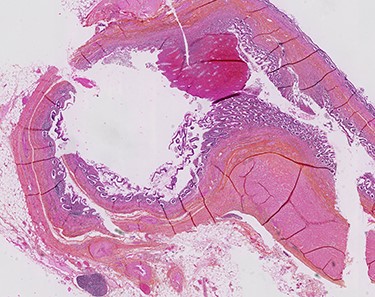
A diagnostic laparoscopy was performed and revealed a whitish granulomatous appendix and a thickened caecum with chronic-like peritoneal adherences. Because of the neoplastic suspicion and anatomic features, a right hemicolectomy with intracorporeal anastomosis was performed after reaching a surgical consensus. The pathology report confirmed a secondary appendicitis on multiple inflamed appendiceal diverticula (see Fig. 2). No neoplasm was identified. The patient was discharged without complication.
DISCUSSION
Appendiceal diverticula are classified as congenital or acquired. Congenital diverticula are true diverticula and are exceptional for approximately 50 cases has been reported [1]. Congenital diverticula are found on the antimesenteric line of the appendix and are thought to be associated with developmental or congenital anomalies such as trisomy 13 or 15 [2].
Acquired diverticula are pseudodiverticula and are an uncommon finding with a prevalence of 1.4% according to a study of 50 thousand autopsies [2]. They are most commonly seen in older adults (>30 year old) and in men (ratio M:F 1.8:1) [3]. Incidence is more important in patient with cystic fibrosis, reaching 14% [2]. They usually present as multiple small diverticula (2–5 mm) on the distal third of the appendix and are mostly found on its mesenteric line. This supports the theory that they are caused by an elevated pressure in the appendix resulting in herniations of the mucosa through the vascular hiatuses of the appendix. The pressure rises from an obstruction caused by a fecalith, an adhesion or a tumor. A chronic obstruction results in an appendiceal diverticulitis [2, 4]. Furthermore, the active submucosal lymphoid tissues make the appendix prone to inflammation episodes and therefore weakening its muscle layer [2]. These episodes could explain that there is no association between appendiceal diverticulosis and sigmoid diverticulosis [3].
Appendiceal diverticulosis is commonly asymptomatic. It is estimated that two-thirds will evolve to an acute or a chronic diverticulitis. Thus, the presentation varies from a mild right iliac fossa pain extending over the years to an episodic intense pain. In the case of an acute presentation, the pain does not usually start around the periumbilical region and is not as commonly associated with gastrointestinal symptoms as appendicitis. Fever and leukocytosis are common findings [2]. Appendiceal diverticulitis is usually a perioperative or a pathologic diagnosis. CT can be useful to distinguish appendicitis from appendiceal diverticulitis but has a 50% false positive rate [2]. It is still a rare radiological finding, as less than 7% of appendiceal diverticulitis are diagnosed on CT [3]. The Lipton classification divides appendiceal diverticulosis and diverticulitis into four subtypes [5]:
Acute diverticulitis;
Appendicitis with acute diverticulitis;
Appendicitis with diverticulum;
Appendix with diverticulum.
The most frequent complication of appendiceal diverticular disease is perforation. The perforation rate of appendicitis is estimated at 6.6% while it rises at 27% when associated with a diverticulum. An acute diverticulitis has a perforation rate of 66%, explaining the 30-fold more mortality of appendiceal diverticulitis compared to appendicitis. Other reported complications are abscesses or cysts formation, peritonitis, massive hemorrhage and vesicoappendiceal fistula. Congenital appendiceal diverticula are less associated with complications [2].
Appendiceal diverticular disease is associated with appendiceal neoplasms. The incidence of appendiceal neoplasms is 1.28% and rises at 26.94% in presence of diverticula. More than half of the neoplasms are low grade mucinous neoplasms (LGMN). It is unclear if the LGMN causes the elevated pressure resulting in diverticula or if it develops within the diverticula and weaken its walls. Because of its strong association with LGMN, appendiceal diverticular disease is thought to be associated with pseudomyxoma peritonei [2, 3]. The presence of serosal and/or mesoappendiceal mucin should raise concerns of a neoplastic process [6].
CONCLUSION
Appendiceal diverticular disease is an uncommon diagnosis that can easily be overlooked. Because of its strong association with appendiceal neoplasms, a thorough examination of appendix should be done after each appendicectomy as well as a careful inspection of the abdominal cavity. Considering the high complication rate, mortality rate and malignant association, an urgent appendicectomy in case of an appendiceal diverticulitis and an elective appendicectomy in case of an incidental finding of appendiceal diverticulosis should be recommended to the patient. If appendectomy cannot be done safely, a laparoscopic right hemicolectomy may be considered after discussion with the patient.
AUTHORS' CONTRIBUTIONS
Kristopher Bujold-Pitre is a medical student and has written the paper. Dr Olivier Mailloux is the Chief of Surgery CISSS Côte-Nord and clinical instructor at Université Laval. He was the operating surgeon and has reviewed the paper.
CONFLICT OF INTEREST STATEMENT
None declared.



