-
PDF
- Split View
-
Views
-
Cite
Cite
Herbert Oye, Arham Aslam, An usually early presentation of peripheral arterial disease in a 30-year-old woman, Journal of Surgical Case Reports, Volume 2021, Issue 10, October 2021, rjab457, https://doi.org/10.1093/jscr/rjab457
Close - Share Icon Share
Abstract
Peripheral vascular disease is commonly thought to be a disease of elderly patients. However, with certain environmental factors and predetermined genetics, it can present much earlier in life. This case report demonstrates a case of severe peripheral vascular disease in a 30-year-old woman with an 11-year history of smoking. We report the case of a 30-year-old woman who presented to our clinic with a 9-year history of peripheral vascular disease. She complained of worsening claudication in both lower extremities and intermittent pain at rest. A CT arteriogram was conducted and showed significant stenosis of both left and right iliac arteries, as well as stenosis of the distal aorta. In the setting of certain genetic and environmental factors, the presentation of peripheral vascular disease can occur significantly earlier in life.
INTRODUCTION
With roughly 6.5 million Americans over the age of 40 affected by peripheral vascular disease [1], it is commonly thought to be a disease of the aged. In the setting of certain risk factors, such as diabetes, hypercholesterolemia, hypertension and smoking, atherosclerotic plaques take years to build-up enough to cause significant stenosis. Although all vessels may be affected, the lower extremities are more commonly involved in the symptoms of peripheral vascular disease. We report the case of a 30-year-old woman who presented to our clinic with worsening symptoms of peripheral vascular disease.
CASE PRESENTATION
The patient was a 30-year-old woman who was diagnosed with peripheral vascular disease 9 years prior to this encounter. She presented to our clinic with complaints of worsening pain in the lower extremities with activity and sometimes pain at rest. The patient had a medical history of hypertension and admitted to non-compliance with medication. She has been smoking cigarettes for 11 years and usually consumes 1 pack per day. In addition, she reported a strong family history of coronary artery disease. The patient was taken to the office-based lab located within the clinic and was prepared sterilely for a catheter arteriogram.
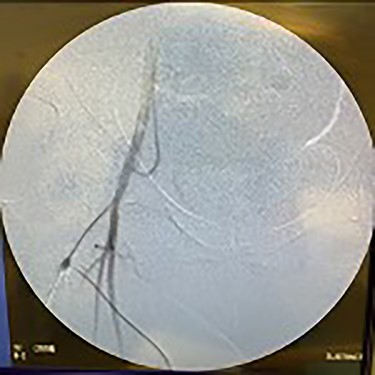
Catheter arteriogram results showed significant occlusion of the left iliac artery (Figs 3 and 4), the right iliac artery (Fig. 1), as well as the distal abdominal aorta (Fig. 2). There were numerous collateral vessels noted, indicating the presence of long-standing proximal stenosis (Fig. 1). The decision was made to use angioplasty to help widen the areas of stenosis. An 8 mm × 40 mm Passeo balloon was advanced from the right femoral artery into the left iliac artery (Fig. 7) and insufflated to 6 mmHg (Fig. 6). The balloon was allowed to remain expanded for 1 min and then was deflated. Next, the distal aorta was repaired in a similar fashion. The balloon was advanced into the distal aorta from the right femoral access and insufflated to 12 mmHg (Fig. 8). The balloon was allowed to remain expanded for 90 s.

Fluoroscopy of right iliac artery showing vast collateral vascular formation, indicating long-standing proximal obstruction.


Fluoroscopy of bilateral iliac arteries showing significant arterial disease.

Fluoroscopy of bilateral iliac arteries showing significant arterial disease.





Fluoroscopy showing dilation of the distal aorta post-angioplasty.


Fluoroscopy showing dilation of the right iliac vessel post-angioplasty.



Lastly, the right iliac artery (Fig. 5) was treated using the same method (Fig. 10). After completion of the angioplasty procedure, catheter arteriogram was repeated to visualize the effectiveness of the procedure in relieving the extensive stenosis. The imaging revealed almost complete restoration of the diameter of both left and right iliac arteries (Figs 11 and 12). The distal aorta also showed improved diameter after the procedure (Fig. 9). Angiogram of both lower extremities was also performed. The catheter was passed distal to the stenosis that was previously present in the left iliac artery, to help visualize perfusion of its distal branches (Figs 13 and 14). The catheter was removed from the right femoral artery and reinserted in a distal fashion, to help visualize downstream perfusion. The right popliteal artery was well visualized on angiogram (Fig. 15), signifying strong perfusion. The patient was strongly advised to discontinue smoking cigarettes. In addition, the patient was advised to maintain regular physical exercise as tolerated and take baby aspirin daily to prevent thrombotic events.
DISCUSSION
The patient in this case developed peripheral vascular disease at an unusually early age than is expected. This may be a result of modifiable risk factors, such as hypertension, obesity and smoking. While pain in the lower extremities in young adults is commonly caused by trauma or muscular pathologies, the differential of peripheral arterial disease should also be considered. This is especially true in the setting of comorbid conditions and risk factors. The treatment of peripheral arterial disease focuses on reducing exposure to the risk factors, such as quitting smoking and regular exercise. Pharmacological options include antiplatelet agents, such as aspirin, to prevent thrombotic events. Cilostazol, a phosphodiesterase-3 inhibitor, has been shown to reduce the symptoms of claudication in patients with peripheral arterial disease.
The unique nature of significant peripheral arterial disease in a relatively young patient with a strong family history of coronary artery disease and smoking, carries significant comorbidity concerns for the future. We elected not to stent the vessels at this time, due to the small caliber of the vessels. With continued smoking, the placement of stents in this patient’s vessels may induce thrombosis.
CONCLUSION
Endovascular intervention in this young patient in the form of angioplasty alone, showed good promise and avoided the need for stenting. Endovascular intervention can delay the need for a major aortobifemoral bypass in this young patient, as well as thrombotic complications associated with stenting.



