-
PDF
- Split View
-
Views
-
Cite
Cite
Marie Nguyen, Aaron E Lim, Eshwarshanker Jeyarajan, Mary-Ann Koh, Andrew Ng, Phillip Townend, Giant hepatic haemangioma rupture in a patient on direct oral anticoagulant therapy, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa523, https://doi.org/10.1093/jscr/rjaa523
Close - Share Icon Share
Abstract
Rupture of a liver haemangioma is extremely rare, with less than 100 cases reported in the literature. This is the first case known to date reporting a rupture occurring with direct oral anticoagulant therapy. A 76-year-old woman presented with acute abdominal pain and syncope in the context of commencing apixaban 4 weeks prior. Abdominal computed tomography and angiography demonstrated a large heterogenous mass in the left liver lobe with contrast blush suggestive of a bleeding tumour. Urgent transcatheter arterial embolization successfully ceased haemorrhage. Due to persistent compressive symptoms, a left lateral hepatectomy was performed. CD34 immunostaining of the tissue revealed variably sized vessels, which was consistent with a ruptured giant hepatic haemangioma. Our case substantiates the limited available literature regarding ruptured haemangiomas. Combined with previous case reports, this report will significantly contribute to our understanding of the risk factors, diagnosis and surgical indications for ruptured hepatic haemangiomas.
INTRODUCTION
Hepatic haemangiomas are the most common benign tumour of the liver [1]. Mesenchymal in origin, haemangiomas are composed of masses of blood vessels that are atypical in arrangement and size [1]. Most cases are asymptomatic, while few may present with symptoms related to tumour growth or compression of adjacent structures [2]. Rupture is a rare complication either occurring spontaneously or as a consequence of trauma [1–3]. Donati et al. [3] reviewed the 97 cases of ruptured liver haemangiomas published between 1898 and 2010, including two cases occurring with antithrombotic therapy. We present the case of a giant hepatic haemangioma rupture in the context of recent apixaban treatment that was subsequently treated with transcatheter arterial embolization (TAE) followed by left lateral hepatectomy. This is the first case report of a liver haemangioma rupture as a potential complication of direct oral anticoagulant (DOAC) use.
CASE REPORT
A 76-year-old woman presented with three syncopal episodes and a 2-day history of worsening abdominal pain. She had no nausea, vomiting, bowel changes or history of recent trauma. Apixaban (2.5 mg twice a day) was commenced 4 weeks prior for atrial fibrillation. Other past medical history included Parkinson’s disease. She had no history of malignancy or chronic liver disease. On presentation, she was pale, hypotensive (114/44 mmHg) and tachycardic (106 beats/minute). Physical examination demonstrated diffuse abdominal tenderness and distension without any signs of peritoneal irritation. Laboratory investigations revealed low haemoglobin (60 g/L), red blood cell count (2.35 × 1012/L) and haematocrit (0.215 L/L). Mean cell volume (92 fL) and platelets (190 × 109/L) were within range. Coagulation and liver function tests were unremarkable. Contrast-enhanced computerized tomography (CECT) reported a 62 × 83 × 90 mm heterogenous mass in the left lobe of the liver demonstrating contrast blush with large volume haemoperitoneum concerning for a bleeding hepatic neoplasm (Fig. 1). She was stabilized with five units of packed red blood cells before being transferred to our institute.
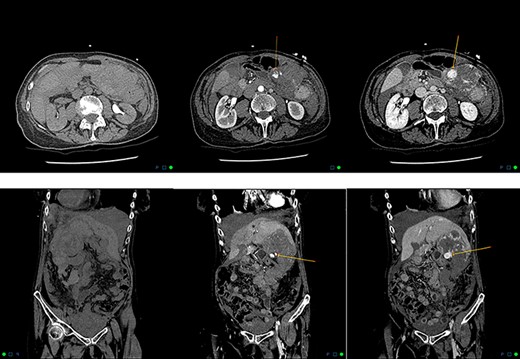
Axial and coronal reformats in non-contrast, arterial and delayed phases demonstrating contrast blush, with pooling within the left hepatic lobe haemangioma consistent with active bleeding.
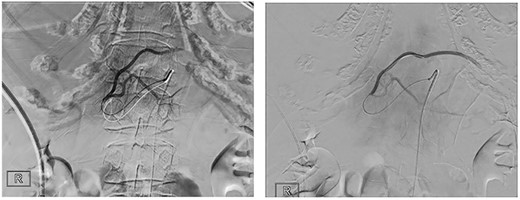
The patient was transferred to the interventional operating room for embolization of the left hepatic artery. Digital subtraction angiography (DSA) showed active contrast agent extravasation (Fig. 2). The tumour was embolized with 500–700 μm beads followed by gel foam. The patient remained hemodynamically stable throughout the procedure.
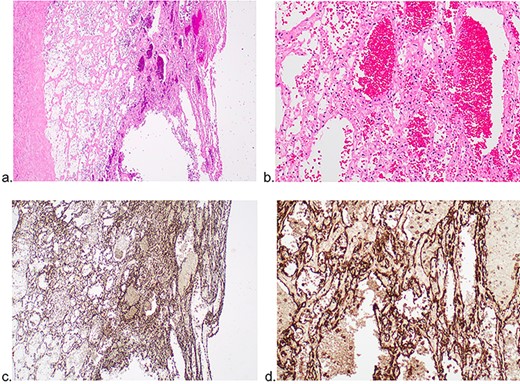
Pathological examination of hepatic mass revealing infarcted tissue and haemorrhage. Preserved areas of variably sized vessels shown.
Given the large size of mass and the patient’s continued symptoms of suppressed satiety and anorexia, a decision was made to perform an open left lateral hepatectomy Day 3 post-embolization. Laparotomy through rooftop incision revealed moderate hemoperitoneum and confinement of a necrotic liver lesion to Segment III. The lesion was not actively bleeding. A stapled left lateral sectionectomy was performed.
Histology showed variably sized dilated spaces within the infarcted and haemorrhagic tissue, mostly showing necrotic nuclei with focal viable bland nuclei lining the spaces. Immunohistochemistry with CD34 staining was positive in these cells (Fig. 3): (a) H&E, ×40, (b) H&E, ×400, (c) CD34 immunohistochemistry ×40 and (d) CD34 immunohistochemistry ×400. Adjacent liver parenchyma demonstrated preserved architecture. The overall features were consistent with an infarcted haemangioma.
Postoperatively, the patient successfully recovered and was transferred to rehabilitation.
DISCUSSION
Hepatic haemangiomas have an estimated prevalence of 0.4% to 7.3–20% in the general population [1, 2]. They are often asymptomatic and detected incidentally on imaging as small (<4 cm) solitary nodules. Diameters exceeding 4 or 5 cm are considered ‘giant haemangiomas’, with few reaching 20 cm [2, 3]. Spontaneous rupture is an extremely rare complication which can present as sudden abdominal pain and hypovolemic shock [1, 4]. Current literatures regarding risk factors for rupture are limited and conflicting. A 2011 literature review reported no correlation between haemangioma sizes with the risk of rupture [3]. Conversely, a more recent retrospective cohort study found that haemangiomas greater than 4 cm, when peripherally located and exophytic, were more likely to rupture [1].
This is the first case report concerning the rupture of a hepatic haemangioma occurring with recent DOAC treatment. As literature in this area is limited, a causative link may be speculated. A PubMed search yielded two relevant cases regarding antithrombotic therapy and hepatic haemangioma rupture. This may be partially due to the insufficient reporting of concurrent medications in some published cases, which is compounded by the fact that rupture is extremely rare. The small number of cases limits any meaningful statistical measure. In one case, bleeding from a cavernous liver haemangioma occurred with streptokinase therapy [5]. Another case documented a giant haemangioma rupture in a woman after acenocoumarol (vitamin K antagonist) treatment [6]. Unlike vitamin K antagonists, the plasma concentration of DOACs is not detectable by a simple blood test nor is there a reversal agent available. Hence, the risk of bleeding prior to rupture is not quantifiable.
As histology was limited post-embolization, clinical and radiological correlation was required. CD34 staining highlighted poorly preserved vessels of varying calibres, which is often seen in haemangiomas [7]. In the setting of haemorrhage, appropriate radiological features and no evidence of cirrhosis or liver disease, a haemangioma was favoured over hepatocellular carcinoma.
The early use of TAE in managing intraperitoneal haemorrhage was shown in our case to be successful in stopping haemorrhage. However, the tumour continued to elicit compressive symptoms and hence surgical intervention was pursued. Surgical resection and enucleation are traditionally the treatments of choice for symptomatic or ruptured haemangiomas [2, 8]. Surgery also provides useful tissue confirmation as needle liver biopsy carries the risk of haemorrhage [2]. Embolization performed as a bridging technique prior to surgical resection has been shown to stabilize patients and reduce intraoperative blood loss [3, 9, 10]. The long-term success rate of embolization alone, however, has not been well studied [1, 3]. Other less common therapies include surgical ligation, radiofrequency ablation and liver transplant [4, 8].
In conclusion, rupture of a liver haemangioma is rare, with less than 100 reported cases in literature. This is the first report known to date concerning a rupture occurring with recent DOAC therapy. Our case substantiates the limited available literature regarding validity of preoperative TAE and its utility in improving surgical outcomes. Previous case reports combined with this report will significantly contribute to our understanding of the risk factors and surgical indications for ruptured hepatic haemangiomas.
CONSENT
Full informed consent was provided by the patient for the writing of this case and the use of associated images.
ACKNOWLEDGEMENTS
Histology images provided by Pathology Queensland.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



