-
PDF
- Split View
-
Views
-
Cite
Cite
Aaron Rockliff, Maree Loveluck, Adrian Yeoh, Retrograde intussusception post Roux-en-y gastric bypass, Journal of Surgical Case Reports, Volume 2021, Issue 1, January 2021, rjaa452, https://doi.org/10.1093/jscr/rjaa452
Close - Share Icon Share
Abstract
A 72-year-old female presented to the emergency department with a short history of abdominal pain and vomiting, having undergone laparoscopic Roux-en-y gastric bypass (RYGBP) 3 years earlier. Computed tomography imaging revealed intussusception causing small bowel obstruction, so she was taken emergently to theatre. Intra-operative findings were of a retrograde intussusception at the jejunojejunostomy. Retrograde intussusception in patients post RYGBP has a unique pathophysiology and management.
INTRODUCTION
Intussusception is a rare cause for small bowel obstruction in the adult population in which the bowel ‘telescopes’ into itself along the flow of peristalsis. We present a case of retrograde intussusception in a patient who had previously undergone laparoscopic Roux-en-y gastric bypass (LRYGBP) surgery.
CASE REPORT
A 72-year-old female presented to the emergency department with 12 h of severe abdominal pain. She had previously undergone a LRYGBP 3 years earlier resulting in 60 kg of weight loss. On further questioning, the patient reported that she had complete obstipation for 24 h. Computerized tomography (CT) scan demonstrated a jejunal intussusception at the site of the jejunojejunal anastomosis (Fig. 1).
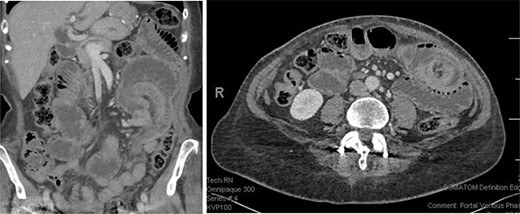
On the left coronal reconstruction showing the area of intussusception (top right); on the right an axial reconstruction showing the classical target sign suggesting intussusception (top right).
The patient was taken to theatre for exploratory laparoscopy, which was converted to a mini-laparotomy due to multiple intra-abdominal adhesions. Operative findings were of a distended alimentary and pancreaticoduodenal limb with obstruction caused by intussusception of the common channel just distal to the anastomosis. Interestingly, the direction of the intussusception was against the flow of peristalsis (Fig. 2).
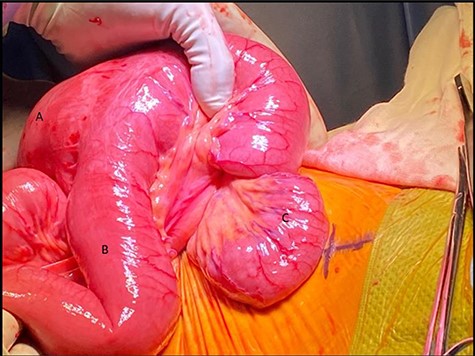
Intra-operative photo showing (A) alimentary limb, (B) pancreaticobilliary limb and (C) common limb with retrograde intussusception extending proximally into the anastomosis.
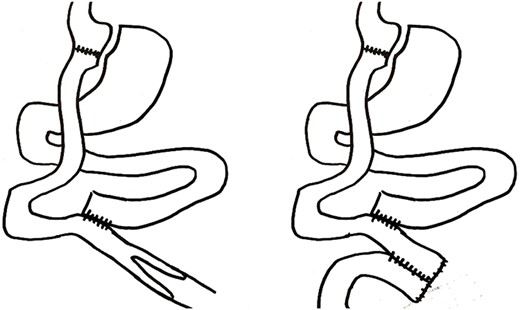
The intussusception was reduced, and the affected segment was found to be oedematous but viable, no obvious lead point was identified. The oedematous segment was resected to allow inspection of the proximal bowel and exclude any lead point, and the bowel anastomosed with a stapled side-to-side technique to prevent further intussusception by creating an S-bend in the reconstructed anatomy (Fig. 3). Post-operatively the patient recovered well and was discharged home on Day 6 of their admission. Oral diet was commenced the day following her operation and she had passage of stool in the same day. Histology of the resected segment showed infarction of the mucosa, but no other pathology.
DISCUSSION
Small bowel obstruction is a common complication of LRYGBP, affecting between 1.5 and 5% of patients [1]. Patients who have had this surgery often present differently and sometimes in extremis, with abdominal pain being the most common presenting complaint. Vomiting is less common in this population, affecting only 46% of patients, likely due to the small size of the gastric pouch [1]. Common causes for small bowel obstruction in this population include internal hernia, adhesions, incisional hernia and jejuno-jejunal stricture [2].
Intussusception is a rarer cause of small bowel obstruction in patients post LRYGBP with a reported incidence of 0.07–0.6% [3]. In this group, the direction of the intussusception is almost always retrograde. One theory for this is that after separating the jejunum from the duodenal pacemaker cells during the Roux-en-y gastric bypass (RYGBP) surgery, ectopic pacemaker cells can arise elsewhere, which can propagate migrating motility complexes (MMCs) in both directions [4].
Case reports of similar cases consistently report the absence of a lead point for the intussusception [3]. Combined with the prevalence of retrograde intussusception, these finding suggest a different pathogenesis in these patients. Retrograde MMCs may meet with anterograde MMCs and form a lead point; thinning of the mesentery with significant weight loss may increase risk; and reactive lymph nodes, adhesions or surgical material can contribute to lead point formation [5].
The literature is conflicting as to what is best done in this situation. Some reports suggest that routinely resecting the affected segment of bowel may not be necessary in every case. If the bowel is viable, reduction with or without enteropexy results in shorter hospital stay, with similar rates of complication when compared to resection [6]. Other literature suggests that enteropexy alone resulted in very high rates of recurrence, which subjects patients to a further operation for the recurrence in the future [7].
In conclusion, retrograde intussusception is an uncommon but documented complication of RYGBP surgery. Due to altered anatomy, these patients can present differently, so a high index of suspicion is required for patients who have had this surgery presenting with abdominal pain. If retrograde intussusception is found intraoperatively current options include reduction and fixation with enteropexy or resection.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
Publication was funded by the Royal Hobart Hospital General Surgery Department.



