-
PDF
- Split View
-
Views
-
Cite
Cite
Keaton Cooley-Rieders, Carlos E Donayre, Ariana M Nelson, Central venous catheter placement leading to an emergent paramedian sternotomy: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa368, https://doi.org/10.1093/jscr/rjaa368
Close - Share Icon Share
Abstract
Perioperative cardiac tamponade during central venous catheter placement is rare. We present a case of tamponade from pulmonary artery injury during dialysis catheter placement resulting in complicated sternotomy and hospital course. A 52-year-old female experienced intraoperative hypotension, rapidly identified as tamponade, that was treated with an emergent paramedian sternotomy. Patient experienced postdischarge dehiscence and osteomyelitis requiring multiple reoperations. This case is the first report of a deviated paramedian sternotomy performed mainly through ribs. The complications experienced outline the importance of effective multidisciplinary knowledge of best practices to stabilize tamponade pathology, mitigating morbidity and mortality.
INTRODUCTION
Below is a case of a rare complication associated with central venous catheter placement. Pulmonary trunk damage as a result of this procedure is only the 8th reported in literature [1]. Additionally, it describes the complication of a sternotomy performed involving the ribs below the sternal notch. This case report highlights the risks and morbidity inherent to an emergent midline sternotomy. It also discusses the utility of pericardiocentesis as the initial treatment of pericardial tamponade.
CASE PRESENTATION
A 52-year-old female with end-stage renal disease on hemodialysis, hypertension, hyperlipidemia, coronary artery disease, heart failure with preserved ejection fraction, and insulin-dependent type 2 diabetes mellitus presented with 2 weeks of right upper extremity swelling. The swelling was attributed to right subclavian vein stenosis, presence of right internal jugular tunneled dialysis catheter, and functional right brachial-antecubital arteriovenous fistula. She was scheduled for removal of the right dialysis catheter, placement of left dialysis catheter, central venography with possible angioplasty and stenting of the right subclavian vein under general anesthesia.
After uncomplicated induction of anesthesia, the patient was anticoagulated with 4000 units of intravenous heparin. The right internal jugular dialysis catheter was removed over a wire placed into the superior vena cava. A large clot was detected in the right subclavian vein, which was treated with angioplasty via the cephalic vein using a 14-mm balloon, resulting in improvement in venous flow. Both access points were closed, and anticoagulation was reversed with 25 mg protamine sulfate 65 minutes after initial heparin bolus. The surgical team then encountered resistance while placing a microwire via the left internal jugular vein into the left subclavian vein for left dialysis catheter placement. After several attempts, the wire was placed under fluoroscopic guidance and the dilator was advanced. During dilator advancement, seen in Fig. 1, resistance was encountered at the cavoatrial junction. Immediately thereafter, the patient experienced profound hypotension and received cardiopulmonary resuscitation (CPR). Intraoperative transesophageal echocardiography imaging demonstrated pericardial tamponade with partial clot. The surgeon obtained large bore vascular access and placed an arterial line in the femoral artery. CPR was stopped after return of spontaneous circulation, with the patient being responsive to vasopressors and further resuscitated with 9 units packed red blood cells, 9 units fresh frozen plasma and 2 units of platelets.
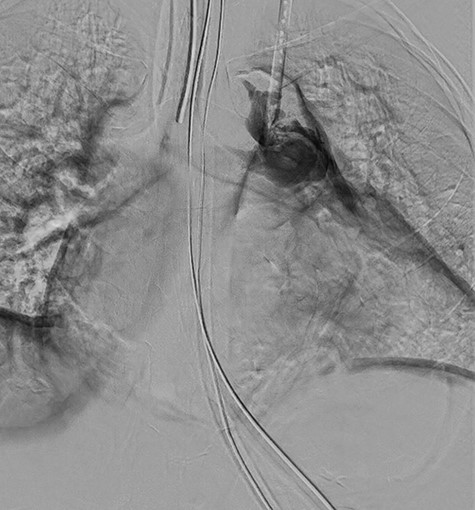
Digital subtraction angiography from operating room fluoroscopy.
The trauma service attending was paged emergently to relieve tamponade and evacuate the clot. A sternotomy was performed left of midline that transected four ribs inferior to the sternal notch. The pericardium was opened and blood with clot was removed with improvement in hemodynamics. Upon arrival of the cardiothoracic team, the mediastinum was explored and a minimally bleeding lesion in the left subclavian vein was identified and closed. On further examination, there was a nonbleeding puncture in the left pulmonary trunk in proximity to the breach in the subclavian. This was the presumed etiology of tamponade and was reinforced with a single pledgeted suture.
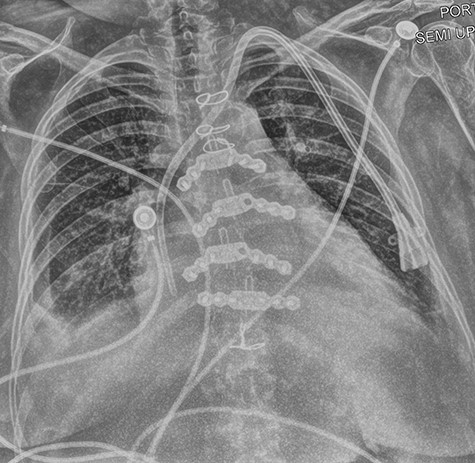
A left internal jugular tunneled dialysis catheter was placed under direct visualization with the tip below the cavoatrial junction for dialysis in the postoperative period. Mediastinal drains were placed, and the sternum was closed with two titanium plates, screws and wires. Chest x-ray can bee seen in Fig. 2.
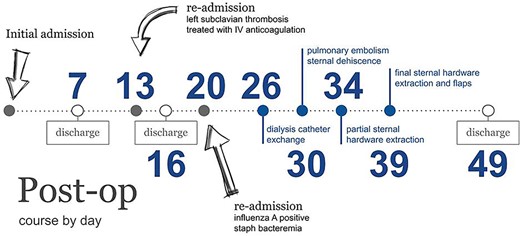
Patient was discharged on post-op day 7, however had a complicated course post discharge with readmissions for central venous thrombosis, pulmonary emboli, sternal dehiscence with osteomyelitis secondary to coagulase negative staphylococcus, bacteremia with the same organism, complicated hardware extraction with sternal reconstruction and flaps. Overview of complications can be seen in Fig. 3. At time of writing, the patient had been seen at outpatient follow-up and was doing well, with removal of her tunneled dialysis catheter and a working right upper arm arteriovenous fistula.
Informed consent for publication was obtained from patient per institutional policies, and sufficiently deidentified to protect privacy.
DISCUSSION/REVIEW OF LITERATURE
The case above describes the first published case of a deviated sternotomy primarily through ribs. Searching for literature to find this complication yielded no reports. Some limited research existed examining paramedian and asymmetric technique, suggesting that increased asymmetry was associated with higher risk of dehiscence, deep sternal wound infections, and instability secondary to unequal distribution of mechanical forces [2–4]. Further, literature on all complications associated with sternotomy in retrospective studies suggested that these incidents similarly impact surgeons regardless of experience [2].
Placement of a guidewire or central venous catheter into the pulmonary artery is a rare complication with the case described above is only the 8th reported instance in literature. All cases that have been reported in the literature report high morbidity but patient survival and positive outcomes [1].
Studies examining iatrogenic causes of pericardial tamponade were primarily related to interventional cardiology procedures or cardiac surgery [5–7]. Management of effusions in this setting was primarily via pericardiocentesis [6]. The percentage of patients requiring surgical treatment after placement of a drainage catheter ranged from 12.7 to 24% [6, 8]. Additionally, improvement in tamponade physiology with this technique was high at approximately 97% [6]. Complication rates at 1.2 to 17.3% [6–8] suggest that pericardiocentesis, especially with ultrasound guidance appeared to be the best initial management approach, either providing definitive treatment or served as a bridge to further intervention.
CONCLUSION
The treatment delivered in the case report definitively managed the patient’s condition through evacuation of pericardial clot. With iatrogenic pericardial tamponade being rare outside of interventional cardiology or cardiac surgery procedures, this case report provides an opportunity to highlight alternative initial treatments. Ultrasound-guided pericardiocentesis has significantly less morbidity, an excellent safety profile, and can be used as a bridge to definitive treatment if required. Based on literature, a majority of patients treated with this modality would ultimately not require further intervention.
The technical errors and inherent risks of median sternotomy seen in this case were consistent with other reports in the literature. In the case, it is likely that sternotomy would have ultimately been required for repair of subclavian vein and evacuation of clot, but in a more controlled environment, the likelihood of paramedian sternotomy complication would undoubtedly be lower, and it is possible that a complicated postoperative course could have been avoided or minimized.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
FUNDING
The authors were provided no funding for the above case report.



