-
PDF
- Split View
-
Views
-
Cite
Cite
Riccardo Bonomi, Miguel Johnson, Gilles Toussoun, Refining aesthetic approaches to tuberous breast using combined minimally invasive approaches to treat moderate asymmetric tuberous breast, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa373, https://doi.org/10.1093/jscr/rjaa373
Close - Share Icon Share
Abstract
Tuberous breast deformity refers to a deformity of the breast that is characterized by varying degree of herniation of the breast parenchyma, widened nipple areolar complex, constriction of the breast base and may involve some degree of hypoplasia. Tuberous breast deformity is most often seen in young women who commonly presents due to dissatisfaction with breast symmetry, as this can be a source of significant psychosocial distress. Principles of reconstruction are focused on recreating an aesthetically pleasing breast shape and achieving symmetrization. Traditionally, reconstruction commonly involved utilization of breast implants or local flap to achieve these goals. The introduction of fat transfer has led to a paradigm shift in aesthetic breast surgery. Fat grafting is safe and can reliably achieve satisfactory aesthetic results in selected cases and reduces the need for implants or local flaps. Concepts that reduce scar burden allows for even more satisfactory aesthetic outcomes.
INTRODUCTION
Tuberous breast deformity refers to a deformity of the breast clinically presenting with hernia of the parenchyma through the nipple areolar complex (NAC) and may involve varying degree of breast hypoplasia. Several classification systems have been described, however, the Von Heimburg classification is the most widely accepted [1]. Tuberous breast deformity commonly affects young women and may be a source of significant psychosocial distress especially in the pubertal period when it is commonly discovered [2].
The management of tuberous breast deformity remains one of the most challenging breast anomalies to treat, with several described techniques ranging from local flaps and implants insertion as the traditional standard of care. More recently, the use of fat grafting has led to a paradigm shift. This technique allows for decrease scar burden with improved aesthetic results. We present a case that demonstrates improved aesthetic outcomes while minimizing scars.
CASE
A 19-years-old woman presents with asymmetry of her breast and being dissatisfied with their shape since adolescence. She denied any family or personal history of breast disease.
Examination revealed asymmetrical breasts with tuberous deformity worse on the left than the right (Fig. 1). A clinical diagnosis of tuberous breast, von Heimburg Type 2 was noted on the right and Type 1 on the left. The sternal notch to nipple distance was 25 cm on the left and 24 cm on the right, with areolar diameter of 7 cm on the left and 6 cm on the right. The inframammary crease was noted to be more contracted on the left measuring 5 mm higher than the right. Ultrasound evaluation revealed findings in keeping with juvenile breast tissue with no sinister features.
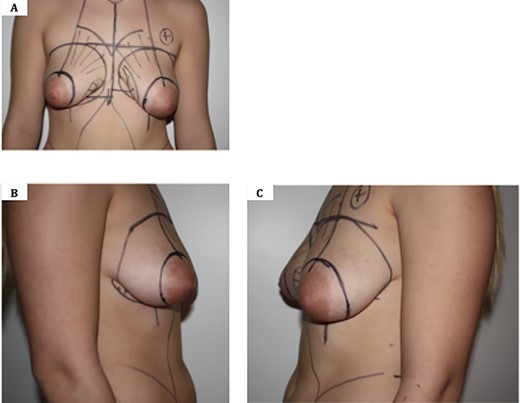
Pre-operative images showing tuberous breast deformity. A. Anterior view; B. Lateral view—right breast; C. Lateral view—left breast. Note asymmetry, widened NAC and herniation of breast parenchyma.
Following counselling, evaluation and a ‘cooling off’ period of 2 weeks, mutual consent was obtained to undertake the combination of a Benelli technique to reduce the areola diameter bilaterally followed by bilateral lipomodelling with a minimally invasive approach to minimize scarring.
Postoperatively, patient was place in a bra and this was maintained for 6 weeks. Follow up consultation at 6 weeks revealed minimal scarring with improved symmetry and volume bilaterally (Fig. 2).
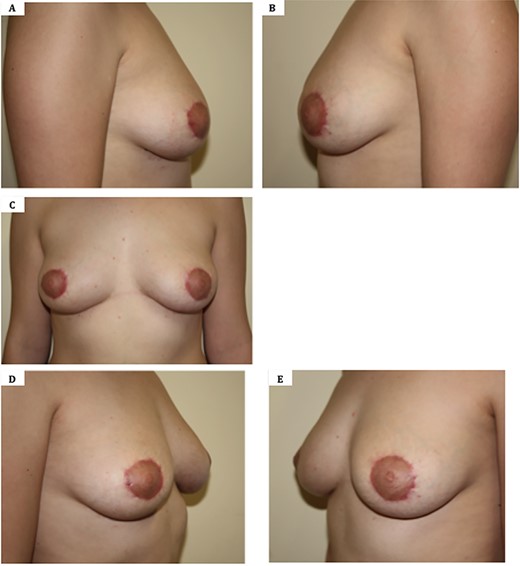
Six weeks post-operative images following correction of tuberous breast deformity using a Benelli approach to reduce NAC size followed by fat grafting. A. Lateral view—Right breast; B. Lateral view—left breast; C. Anterior view; D. Oblique view; E. Oblique view.
TECHNIQUE
Benelli periareolar markings were performed preoperatively in erect position and confirm intraoperatively (Fig. 1). Markings were also made to targeted quadrants for lipomodelling.
Intraoperatively, following general aesthesia, NAC is reduced to 4 cm through the Benelli type of incision. Multiple percutaneous fasciotomies are then performed in a radial fashion using an 18-gauge needle, especially in the inframammary area to allow a more natural distribution of fat and improve shape in medial quadrant.
Fat is then harvested from the back and abdomen using the Coleman technique ``300 cc from back and 120 cc from the abdomen''. Fat is then centrifuged. Following centrifuging, 140 cc of fat is injected in the right breast and 80 in the left one. Symmetry is confirmed intraoperatively by sitting the patient upright. The periareolar wound is then closed and dressings applied.
DISCUSSION
Tuberous breast deformity involves a group of deformity of the breast clinically presenting with varying degree of:
Contracted skin envelope both horizontally and vertically.
Constricted breast base.
Breast parenchyma volume reduction.
An abnormally elevated inframammary fold.
Herniation of the breast parenchyma into the areola.
Based on the original description by Rees and Aston [3], several classifications have since been introduced in an attempt to proposed treatment options for each group. The most widely accepted system which is still used today is the Von Heimburg classification [1]. Other authors have produced similar classification systems [4]. Traditionally, several approaches have been described to correct tuberous breast deformity. These largely involve a combination of correction of the herniation, NAC reduction, breast remodeling techniques and the employment of implants [1].
Pacifico and Kang [5] proposed a more objective assessment of tuberous breast and introduced the ‘Northwood Index’ derived from the ratio of areolar herniation to areolar diameter (herniation divided by diameter). Using this objective measure they later proposed areolar reduction/tightening alone would be ‘curative’ for patients with adequate breast volume and the use of autologous or implant based augmentation when there is a hypoplastic component. Despite their simplified surgical approach to this challenging problem, these techniques invariably result in a significant scar burden as techniques commonly involves a periareolar scar and an inframammary scar to create an implant pocket.
Since the popularization of lipofilling techniques by Coleman [6], there has been a paradigm shift in breast reconstruction [7]. Furthermore, there has been an increasing trend towards improving aesthetic outcomes, as evidence by patient-reported satisfaction outcome measures. Fat grafting is safe, long lasting and offers a versatile option to patients with tuberous breast disorder and can produce excellent aesthetic results in selected patients [8]. It confers a more natural feel and long lasting results as it changes with physiological changes in weight over time. Moreover, fat grafting negates the need for an implant and associated complications in selected patients.
In our proposed technique, minimal scaring can be achieved with the use of a periareolar incision, which appropriately reduces the areolar size. Breast herniation may be corrected by the use of an 18-gauge needle to break up any deep fibrous septae, which are causing a constriction of the breast. This also allows an equal distribution of the glandular tissue in the lower pole and along the inframammary fold. The fat infiltration cannula may also serve as invaluable tool to break deep fibrous septa and in particular, Cooper’s ligaments allowing for improved contouring.
Limiting scar burden has now become one of the important tenets of aesthetic surgery and this 1' is further validated by the SCAR-Q patient outcome scores [9]. Our technique provides satisfactory correction of the tuberous deformity utilizing less scarring than traditionally proposed and that is still practiced today [8].
While our case demonstrates satisfactory aesthetic outcomes, the limitation of this technique is that it may not be applicable to all grades of tuberous breast deformity, especially the more severe types. Fat grafting may however serves as an adjunct in the management of severe deformities.
ACKNOWLEDGMENT
None.
FUNDING
None.
Reference
Author notes
Co-first authors.



