-
PDF
- Split View
-
Views
-
Cite
Cite
Aya N Farfour, Noor A AbuOmar, Fahad I Alsohaibani, Large lipoma of the ascending colon: a case report and review of literature, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa354, https://doi.org/10.1093/jscr/rjaa354
Close - Share Icon Share
Abstract
Gastrointestinal lipomas are a rare benign non-epithelial neoplasms derived from mature adipocytes. The colon is the commonest organ involved in the entire digestive tract and has an incidence rate ~4.4% in autopsy series. Most of the colonic lipomas are asymptomatic and incidentally detected. Lipomas need to be distinguished from true neoplasia, because in most cases they do not need to be resected unless when they cause a clear symptom or they are large in size. Surgical rather than endoscopic resection is preferred for lipomas > 2 cm to avoid complications such as bleeding and perforation. We report a case of a 56-year-old female, a known case of locally advanced breast cancer and positive adenomatous polyposis coli mutation, who was found to have 4 cm ascending colon lipoma by imaging and confirmed by colonoscopy and histopathology.
INTRODUCTION
Lipomas of the colon are a benign growth of adipose tissue found in the submucosa. They are often incidentally detected during imaging, colonoscopy, surgery or autopsy. The first colonic lipoma was reported by Bauer in 1757 [1]. After the adenomatous polyp, colonic lipomas are the second most common benign tumors of the colon. The incidence of colonic lipomas ranges from 0.2 to 4.4% [2]. The colon is the most frequently involved segment of the digestive system, accounting for 65–75% of lipomas [1]. The majority of lipomas are asymptomatic and their size is usually <2 cm [3]. Malignant transformation has never been reported; although when examined histologically, some lipomas have atypical ‘pseudosarcomatous’ features [4].
CASE REPORT
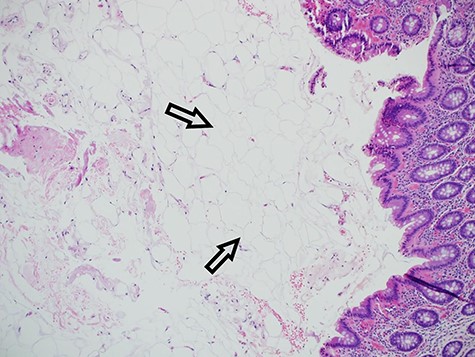
Our patient is 56-year-old female, a known case of locally advanced breast carcinoma. She was initially managed by chemotherapy followed by modified radical mastectomy then adjuvant radiotherapy and chemotherapy. The patient gave a positive family history of colon cancer; therefore, genetic testing for adenomatous polyposis coli (APC) mutation and surveillance colonoscopy were recommended by genetic counselor. The APC gene mutation came to be positive and as part of the work up for her primary disease, computed tomography (CT) scan of the abdomen performed and showed evidence of 4 cm intraluminal lesion in the ascending colon suggestive of lipoma without bowel obstruction (Fig. 1). As a result of these findings, colonoscopy was performed and it revealed a large smooth intraluminal subepithelial lesion in the ascending colon occupying one third of the lumen circumference (Fig. 2). With the use of biopsy forceps, indentation of the tumor can be seen, which is as known as “pillow sign” and once a biopsy taken, a fatty yellowish material was seen protruding from the biopsy site suggestive of lipoma (Fig. 3). Histopathological examination showed multiple fragment of normal colonic mucosa and fragments of mature adipose tissue consistent with lipoma (Fig. 4, black arrows). Clinically, the patient denied history of abdominal pain, rectal bleeding, changes in her bowel habit and intestinal obstruction symptoms. She denied any personal history of malignancy or lipoma. On physical examination, there was no evidence of any lipomas in particular her scalp, limbs or trunk. Although she has no gastrointestinal symptoms attributed to the lipoma, given that it is large in size and she is in clinical and radiological remission, we referred her for the opinion of colorectal surgery.

CT showing a lipoma arising from the wall of the ascending colon without causing obstruction.
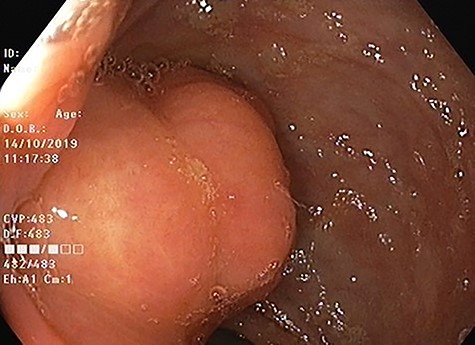
Colonoscopic image of ascending colon lipoma showing normal mucosa.
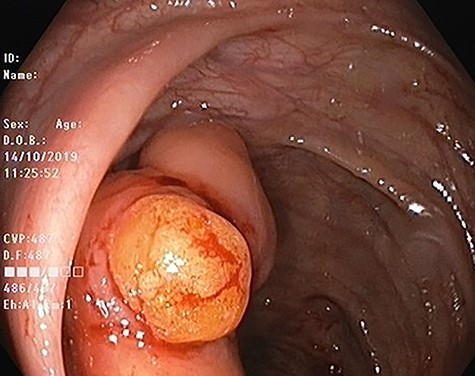
Colonic lipoma after biopsy showing typical yellowish adispose tissue.
DISCUSSION
Lipomas are benign tumors of unknown etiology that are sometimes found in the colon and may cause symptoms through blood loss and bowel obstruction. Several studies have shown that the most common site of colonic lipomas is the ascending colon near the ileocecal valve (45%). Colonic lipomas tend to be solitary but in 10–20% can be multiple. The age at diagnosis ranges within 50–70 years, and are more commonly seen in women [5]. The mean size of the reported colonic lipomas was 5.09 cm with a range from 0.35 to 10 cm and only 30% of them exceed 2 cm in diameter [1]. The most frequent origin of colonic lipoma is the submucosa in 90% of cases but occasionally it extends into the muscularis propria or subserosa. Giant lipoma may be misinterpreted as a premalignant adenomatous polyp, mainly when arising in the left colon [5].
Most of the colonic lipomas cause no significant symptoms and the size of the lipoma is the main predictor of symptoms development. Lipomas > 2 cm in diameter are likely to be symptomatic. The most common symptoms are intermittent crampy abdominal pain, altered bowel habits and chronic blood loss. Giant colonic lipomas can present with acute complications such as rectal bleeding, intestinal obstruction or intussusception [6].
Colonic lipomas are mostly found incidentally during colonoscopy or a CT scan. In contrast-enhanced abdominal CT scan, colonic lipoma has a uniform appearance with smooth border characteristic and fatty densitometric values between 80 and 120 Hounsfield units and that can help differentiate a benign colonic lipoma from other disease processes [7]. On the other hand, magnetic resonance imaging can detect lipomas with a signal intensity characteristic of adipose tissue on T1-weighted and fat-suppressing images [8]. Barium enema usually reveals a filling defect; however, this finding is nonspecific of colonic lipoma or any other type of colonic neoplasm. Occasionally, barium enema show ‘squeeze sign’, in which a radiolucent, spherical filling defect with well-defined margins can be shown to change size and shape in response to peristalsis [9].
Endoscopically, colonic lipoma is recognized easily as a well-delineated, soft, round or ovoid, yellowish sessile or pedunculated mass. Although the mucosa overlying the lipoma is usually intact, however, in rare cases ulcerations and erythema can be seen on the mucosa, which may lead to impression of malignancy. Because of the lipomas’ location in the submucosa, three endoscopic signs may contribute to the diagnosis: the ‘cushion sign’ (probing the polyp with a closed biopsy forceps will often yield a pillow-like indentation), the ‘tenting effect’ (grasping the overlying mucosa with biopsy forceps presents a tent-like appearance), and the ‘naked fat sign’ (biopsies may result in an extrusion of yellowish fat) [4]. Endoscopic ultrasonography (EUS) can be used to distinguish lipoma from other submucosal lesions such as leiomyoma and schwannoma. On EUS, lipoma appears as hyperechoic lesions with regular borders in the three layers. EUS is also useful in the determination of a possible extension into the muscularis propria before attempting endoscopic resection.
For management of colonic lipomas, a follow-up is sufficient for a small and asymptomatic lesion. However, symptomatic lipoma or asymptomatic but >2 cm in size should be considered for resection. Treatment options are various and include endoscopic and surgical resections. Endoscopic resection is preferred for symptomatic lipomas with a diameter < 2 cm or pedunculated lipomas. Colonic lipoma is >2 cm, endoscopic resection is associated with a high rate of complications such as hemorrhage and perforation. According to Jiang and colleagues [10], surgical intervention is warranted when the lipoma is >4 cm in size; there is an unclear preoperative diagnosis; the lipoma has associated intussusception and the patient is symptomatic; there is involvement of the muscular or serosal layer; or the lesion cannot be resected endoscopically. The choice of surgical intervention method depends on the lipoma size, location and the presence of comorbidities. Recurrence of colon lipoma after surgical treatment has not been documented.
AUTHOR CONTRIBUTIONS
All authors contributed equally to this article.
CONFLICT OF INTEREST STATEMENT
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
FUNDING
The authors received no financial support for the research, authorship, and/or publication of this article.
ETHICAL APPROVAL
Our institution does not require ethical approval for reporting individual cases or case series.



