-
PDF
- Split View
-
Views
-
Cite
Cite
Taiki Sunakawa, Kenju Ko, Ryo Moriyasu, Yasunori Nishida, Noriaki Otagiri, Katsunori Tauchi, Emergency surgery for acute cholecystitis associated with cholecystocolonic fistula caused by gallbladder cancer: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa305, https://doi.org/10.1093/jscr/rjaa305
Close - Share Icon Share
Abstract
Preoperative diagnosis of cholecystocolonic fistula (CCF) is difficult and the contribution of gallbladder cancer or colon cancer is unclear when there is associated malignancy. We present a case that was diagnosed with acute cholecystitis associated with CCF by multidetector computed tomography (MDCT) preoperatively and malignant neoplasm during emergency surgery. She was finally diagnosed with gallbladder cancer after the operation and underwent a two-stage surgery for regional lymph node dissection. Gallbladder cancer can be a primary malignant cancer causing CCF, whereas MDCT is useful for preoperative diagnosis of CCF. A treatment plan in consideration of gallbladder cancer is advisable for CCF associated with malignant tumor.
INTRODUCTION
The Tokyo Guideline currently recommends early cholecystectomy for acute cholecystitis, and emergency surgery for this disease is increasing. Cholecystocolonic fistula (CCF) is a rare complication of cholecystitis, and preoperative diagnosis of CCF is generally difficult. Here, we present a case of CCF diagnosed preoperatively that was associated with gallbladder cancer.
CASE REPORT
An 80-year-old woman presented to our emergency department with right upper abdominal pain. She had been treated conservatively for acute gallstone cholecystitis about 40 years before. Thereafter, she had been diagnosed with cholelithiasis several times and followed without therapy.
Physical examination showed only severe right upper abdominal tenderness. She had a slight fever, with otherwise normal vital signs. White blood cell, C-reactive protein and total bilirubin level were elevated by 11 300/mm3, 21.2 mg/dl and 1.8 mg/dl, respectively, according to blood tests. Other blood test results were within normal range.
Abdominal ultrasound showed gallbladder wall thickness and many gallstones. Multidetector computed tomography (MDCT) with intravenous contrast material revealed gallbladder distension, a thick-walled gallbladder and inflammation in pericholecystic soft tissues (Fig. 1). Air in the gallbladder and a fistulous connection between the gallbladder and transverse colon were also detected. The diameter of the fistula was ~2 cm. However, tumorous lesions inside the gallbladder were not confirmed.
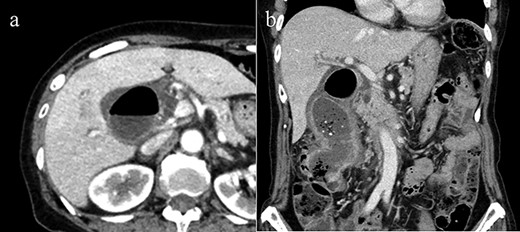
(a) Axial CT image reveals pneumobilia and wall thickness of the gallbladder, but did not show fistulous connection with the colon clearly. (b) Coronal view of CT demonstrates CCF. No CT imaging angle could clearly show the tumorous lesion.
She was diagnosed with acute cholecystitis secondary to CCF and scheduled for emergency cholecystectomy and partial colectomy. However, intraoperative exploration revealed induration of gallbladder fundus, and colonic or gallbladder cancer associated with CCF was suspected (Fig. 2). Gallbladder aspiration was conducted and yellowish-white cloudy aspirate that indicated the infection was observed. Then, intraoperative cholangiogram showed the known fistula and the location of the bile duct. Intraoperative rapid diagnosis was unavailable due to the emergency operation, and she only underwent cholecystectomy and partial colectomy according to the preoperative plan.
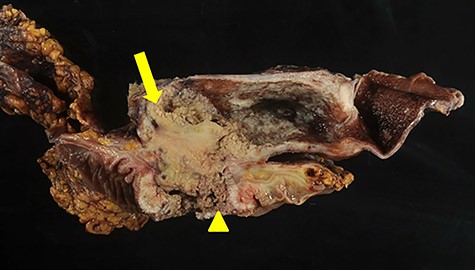
Gross appearance reveals tumor mass within the gallbladder (arrow), adhesion between gallbladder and adjacent colon and fistulous formation (arrowhead).
Evaluation of the pathologic specimen showed squamous cell carcinoma of the gallbladder that infiltrated the transverse colon and formed the CCF (Fig. 3). Surgical margins and resected lymph nodes were all negative. She had regional lymph node dissection 1 month after the first operation, and no metastasis was found.
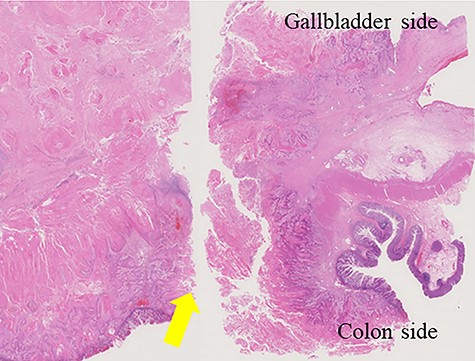
Invasion of gallbladder’s squamous cell carcinoma to the transverse colon and formation of the cholecystcolonic fistula (arrow).
The patient was discharged without any adverse events and has been free of recurrence for >15 months.
DISCUSSION
CCF is a rare illness and the second most common cholecystoenteric fistula after cholecystoduodenal fistula. The incidence of CCF is reported to be 0.06–0.14% in those who underwent cholecystectomy [1]. Preoperative diagnosis rate of CCF is only 7.9% in those undergoing cholecystectomy [2]. CCF is a complication of biliary disease and usually associated with chronic gallbladder inflammation caused by gallstones. Our patient course provided two important clinical suggestions. First, gallbladder cancer should be considered as a possible cause of CCF. Second, MDCT is a very useful modality for detecting CCF preoperatively.
In general, gallbladder cancer is more probable compared with colon cancer as a malignant disease contributing to CCF. Most CCF cases are uncommon complications of chronic gallbladder inflammation caused by gallstones. Other factors of CCF have been reported, such as trauma, previous surgery, cholecystostomy, iatrogenic abdominal wounds or malignant disease. In a previous report, the incidence of CCF caused by gallbladder cancer comprised 1.7% of CCF cases [1]. Another case report demonstrated a patient who had CCF caused by gallbladder cancer and was misdiagnosed with colon cancer preoperatively [3]. Yet another case of CCF was diagnosed with gallbladder cancer by fine needle aspiration cytology and computed tomography (CT) imaging revealed a fistulous connection with the adjacent colon [4]. According to our research, no CCF cases were caused by colon cancer. In fact, a previous report suggested that CCF always originated from gallbladder disease with some exceptions of rare pathologies [1]. Thus, we recommend that gallbladder cancer should be considered as a probable reason if a malignant disease is suspected as a cause of CCF. In our case, as the original cancer site was unconfirmed intraoperatively because we could not perform intraoperative rapid diagnosis; we, therefore, carried out a two-stage surgery for lymph node dissection. Generally, chronic inflammation of gallbladder is a primary cause of CCF and a tumor-related CCF is quite rare. Therefore, in most cases of CCF, it is not necessary to think of lymph node dissection in surgical management of CCF. However, in cases where rapid biopsy is not available and the patient is too fragile to reoperate, one could consider gallbladder cancer as the cause and perform one-step surgery including regional lymph node dissection based on gallbladder cancer.
We diagnosed CCF preoperatively by MDCT with intravenous contrast material. A variety of diagnostic imaging techniques have been reported to diagnose CCF, but the methods to detect CCF effectively and the features of imaging findings for CCF are controversial. In the literature, the preoperative diagnosis of CCF has been made with barium enema, ultrasound, abdominal plain X-ray, colonoscopy, hepatobiliary imaging or endoscopic retrograde cholangiography. While all these methods might be valuable to detect CCF in some cases, it is disputable which technique is best to diagnose CCF. In some reports, the presence of pneumobilia or atrophic gallbladder is suggestive of CCF [3–7]. CT reveals these findings clearly, and recent advances in CT imaging has improved its ability to diagnose CCF. MDCT is a minimally invasive way to diagnose CCF, and we suggest that MDCT is currently the most ideal method to detect this disease. In fact, MDCT of our case showed these imaging features and demonstrated the fistula connection between the gallbladder and the adjacent colon. She was consequently diagnosed with CCF preoperatively.
In conclusion, CCF of this patient was caused by gallbladder cancer and MDCT showed the fistulous connection and some imaging characteristics of CCF. We recommend that gallbladder cancer is suspected as the malignant tumor from which the CCF originates as there has been no reported case of CCF associated with colon cancer. Furthermore, MDCT is a very effective tool to find CCF preoperatively. Further case reports are necessary for more information about CCF caused by malignant illness and effective CCF detection tools.
CONFLICT OF INTEREST STATEMENT
None declared.



