-
PDF
- Split View
-
Views
-
Cite
Cite
Aghyad Kudra Danial, Mario Bedon, Nour Kalaji, Nasri Nasra, Hayat Khalil, Isolated complete transection of common hepatic artery in a fall accident: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa350, https://doi.org/10.1093/jscr/rjaa350
Close - Share Icon Share
Abstract
Blunt abdominal trauma is the most frequent external injury to the abdomen, which is rarely due to falling. However, not often does a blunt trauma cause injury to the common hepatic artery. Isolated injury of the common hepatic artery has rarely been reported in the literature. This report describes an unusual case of a falling accident from a height of 5 meters that results in complete transection of the common hepatic artery, yet all other abdominal organs are normal. The case was initially diagnosed by a Focused Assessment with Sonography in Trauma exam and confirmed with an exploratory laparotomy. The successful management would be an end-to-end anastomosis of the dissected artery. We hope we would raise awareness of such injury in order to facilitate its diagnosis and management and improve its outcome.
INTRODUCTION
Intra-abdominal injuries result most commonly from blunt trauma [1], which often occurs due to motor vehicle accidents and less likely to falling. The majority of blunt trauma cases occur before the age of 45 with a significant male predominance. The spleen is the most affected organ in blunt abdominal injuries, followed by the liver and the small intestine [2]. Abdominal injury in a fall is extremely rare and often detrimental, as other body parts (e.g. the chest and head) are usually affected [3]. Injury to the hepatic arteries is now increasingly iatrogenic, resulting in aneurysms that can rupture [4]. A dissected artery is a rare consequence of a blunt trauma, whereby arterial occlusion or pseudoaneurysm may develop more frequently [5]. We present to you the first case of an isolated completely transected common hepatic artery (CHA) injury (without damage to the liver or other organs) in a 27-year-old Iranian man due to a fall accident, which can be tricky to diagnose at first sight.
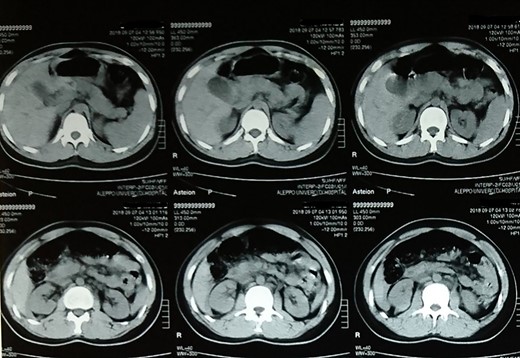
Follow-up computed tomography scan of the abdomen showing no abnormalities.
CASE REPORT
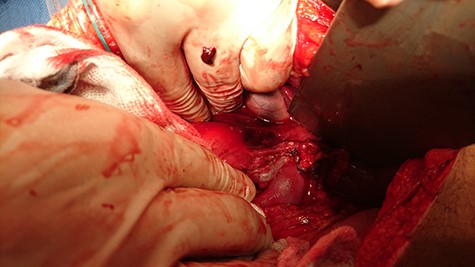
A 27-year-old Iranian man presented to the surgical emergency department with a complaint of falling from a height of 5 meters. He landed striking his abdomen on a flat hard surface. The patient weighed 70 kg and had no history of coagulation disorder or anticoagulation therapy. He arrived after 18 min and was assessed by the airway, breathing, circulation (ABC) approach. On examination, the patient was awake, responsive and in pain. The airway tract was patent. No lacerations or ecchymoses were identified on the chest wall skin. Respiratory sounds were clearly heard on both sides. His blood pressure was 90/50 mm Hg and his pulse rate 120 bpm. The patient expressed a generalized abdominal pain and rebound tenderness in the right hypochondrium. A laceration was identified in the right upper quadrant. A Focused Assessment with Sonography in Trauma exam revealed approximately 1500 ml of free fluid in Morrison’s space and the pelvis. Chest radiography was completely normal; no pleural effusion, pneumothorax or broken ribs were seen. Two peripheral IV lines were inserted and IV isotonic saline fluids were administered. He was transferred then to the operating room and underwent an exploratory laparotomy via midline incision. Two liters of blood was found in the abdominal cavity and packing of the four abdominal quadrants was performed to temporarily stop the bleeding. A completely transected common hepatic artery was recognized. The bleeding was controlled and the dissected artery was reattached by an end-to-end anastomosis with a Prolene (monofilament polypropylene) suture 5-0 (Fig. 1). Examination of the remaining abdominal organs revealed nothing abnormal. During surgery, X-ray radiography of the lumbar spine and pelvis was performed and showed no abnormalities. A drain was placed in Morison’s space. Four units of whole blood and four units of fresh frozen plasma were transferred to the patient.
On the first day after surgery, the patient’s overall condition was stable. On the fourth day, the drainage tube was removed and a computed tomography scan of the abdomen was performed, which was normal (Fig. 2). Afterwards, the patient was discharged and did not report any further complaint.
DISCUSSION
Blunt trauma to the abdomen is a very frequent complaint, amounting ~70% of intra-abdominal injuries presenting to the Emergency Department. Mortality in abdominal blunt trauma is significant, with ~25% of cases leading to death [1]. Males present the majority of cases (70%). Most cases occur due to motor vehicle accidents, but only a minority (6%) result from falling accidents. The spleen ranked as the first of the most affected organ in blunt traumas, followed by the liver, small intestine and kidney [2]. The head, spine and extremities are the main targets of fall accidents at home or work, whereas the abdomen is rarely injured (2.12%) [3]. Blunt insults to a visceral artery can produce several pathological forms: pseudoaneurysm (the most common) [4], occlusion [5] or partial/complete transection. In contrast to transections, pseudoaneurysms of the hepatic artery may produce peritoneal symptoms days to months after the initial injury [6]. If the proper hepatic artery is damaged, a hematoma may arise in the porta hepatis and compress adjacent structures without any sign of hemoperitoneum [7], but the injury in our case presented with a significant abdominal bleeding since CHA is located outside of porta hepatis.
The literature lacks reported cases of isolated complete hepatic artery transection as a result of trauma. The main goal of this case report is to orient surgeons to investigate CHA injury in patients with extensive hemoperitoneum caused by relatively weaker blows to the abdomen. The blow may not be forceful enough to damage major abdominal organs, in contrast to situations where an impactful hit (as in automobile accidents) has a higher chance of damaging not only the hepatic arteries but other abdominal organs and other sections of the body [6]. The uniqueness of this case arises from the fact that of all abdominal parts, only CHA was damaged, which implies CHA may be the first target of relatively weaker abdominal injuries in a patient with no previous illnesses. One theory to explain this case might be that CHA is usually located somewhat perpendicularly to its usual origin and its major branches. Hence, CHA lies in a location where the forces inflicted by the blunt trauma may join to overwhelm the artery, causing it to transect. This theory must be criticized.
According to Jurkovich et al. [8], artery ligation is preferred over primary repair when the situation demands blood replacement, because primary repair is time-consuming and may be easily complicated. However, that would be the case if the arterial injury is associated with other traumas, but in our patient the insult was limited to CHA, and we judged that the situation should be best managed with an end-to-end anastomosis.
We think that the literature should be equipped to help surgeons in producing an initial prediction of the causes of injuries. This would save time wasted on indecisive examinations in situations that demand quick diagonses. We hope this case would contribute to the perfection of medical knowledge in emergencies.



